Published online Jul 6, 2024. doi: 10.12998/wjcc.v12.i19.3925
Revised: April 12, 2024
Accepted: April 29, 2024
Published online: July 6, 2024
Processing time: 136 Days and 19.5 Hours
Esophageal cancer is the sixth leading cause of cancer-related death and eighth most common cancer, affecting > 450000 people worldwide. Esophageal squa
A 61-year-old esophageal cancer patient was found to have lung and brain meta
Postoperative pathology and immunohistochemistry confirmed EACC with rare anal metastasis. More exploration of EACC diagnosis and treatment is needed.
Core Tip: Adenoid cystic carcinoma of the esophagus is easily misdiagnosed by endoscopic pathology. Surgical pathology and immunohistochemistry are the gold standards for diagnosis and at present, surgery is still our preferred treatment option. Adjuvant chemotherapy and targeted therapy are given for patients with distant metastasis. Whilst radiotherapy can be used locally, there has not been a precise study on optimal chemotherapy regimens. More research is needed to explore treatment options for esophageal adenoid cystic carcinoma.
- Citation: Xu L, Xu R, Sun J. Anal metastasis in esophageal cancer: A case report. World J Clin Cases 2024; 12(19): 3925-3930
- URL: https://www.wjgnet.com/2307-8960/full/v12/i19/3925.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i19.3925
Esophageal cancer is the sixth leading cause of cancer-related death and the eighth most common cancer worldwide, affecting more than 450000 people worldwide[1]. The incidence of esophageal cancer is rapidly increasing. Esophageal carcinoma is characterized by its high mortality, poor prognosis at diagnosis, and variability based on geographic location[2]. Esophageal squamous cell carcinoma is the main histological type worldwide. However, in some countries, including the United States, United Kingdom, Australia, and Western Europe countries (Finland, France, Norway), the adenocarcinoma subtype predominates, whereas squamous cell carcinoma is the second most common[3]. The number of esophageal cancer cases in China accounts for 53.7% of the world's esophageal cancer population[4]. The progression of esophageal cancer is relatively insidious, with most patients already at a middle or advanced stage at the time of diagnosis. Squamous cell carcinoma is still the most common in China. Alcohol consumption, smoking, and genetics are high-risk factors for esophageal squamous cell carcinoma, whereas drinking, smoking, Barrett's esophagus, and obesity are high-risk factors for esophageal adenocarcinoma[3]. The liver is the most common distant metastatic site in esophageal cancer, followed by lymph nodes, lung, bone and brain[5]. Esophageal cancer with anal metastasis is rare in clinical practice. Here, we describe a patient with esophageal cancer who developed anal metastasis after 4 years of regular chemotherapy.
A 61-year-old male was admitted to hospital with mild choking after drinking alcohol.
Five years previously, the patient was similarly admitted to hospital with mild choking after drinking alcohol. The pa
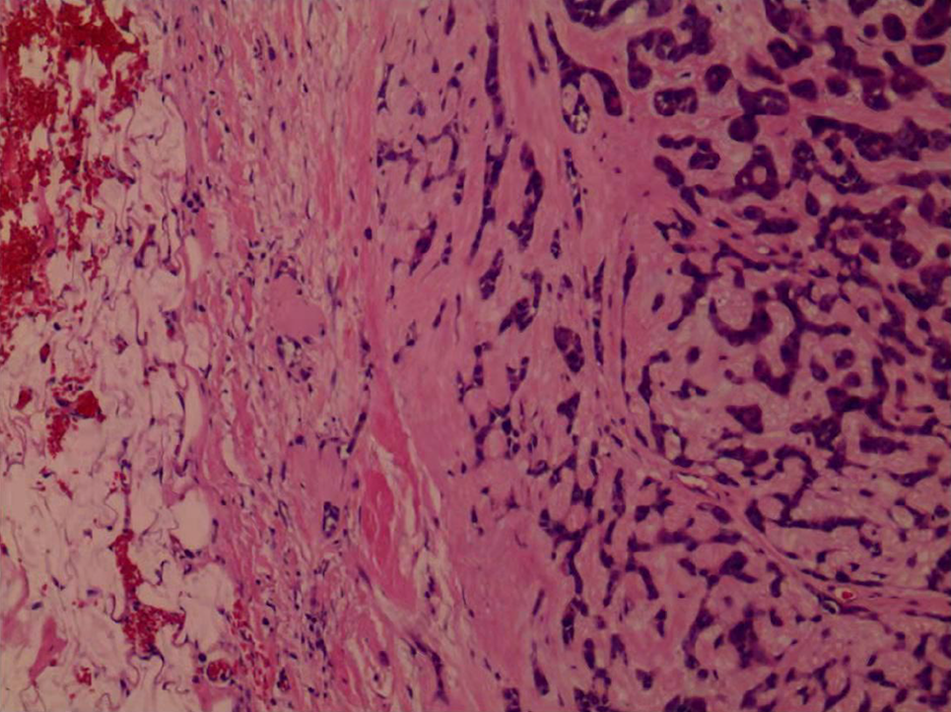
The thoracic surgeon referred the patient to the Oncology Department first for chemotherapy. The oncologist prescribed Lipusol, cisplatin, and Seggio chemotherapy for four cycles. Following chemotherapy, the patient underwent thoracic surgery. Postoperative pathology and immunohistochemistry showed esophageal adenoid cystic carcinoma (EACC) (Figure 2).
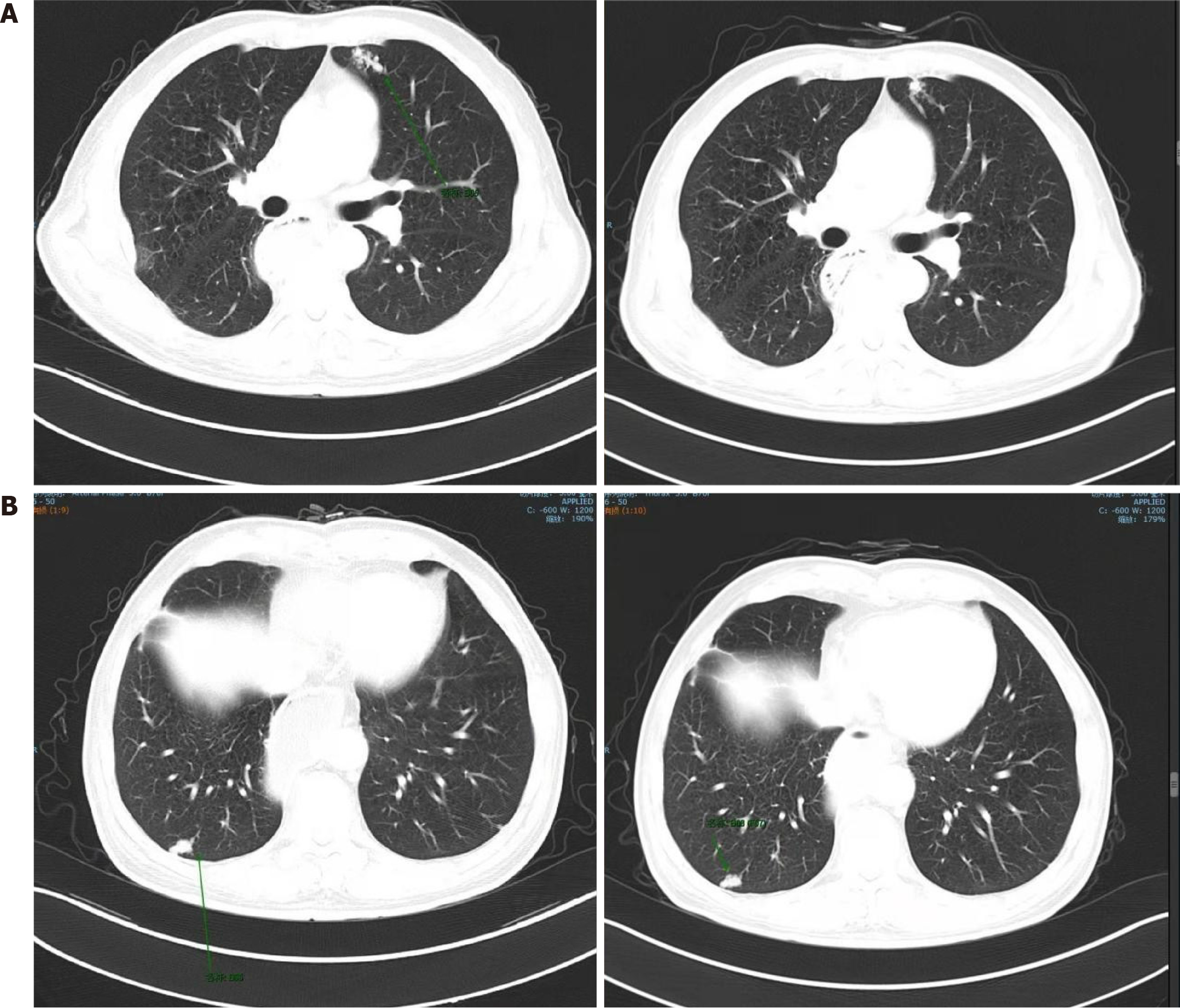
Following surgery, the oncologist administered paclitaxel liposome + Seggio chemotherapy. A CT scan in December 2019 identified patchy and lumpy soft tissue density shadows in both lungs, which had increased in size compared with those observed on a CT performed in September 2019 (Figure 3). Subsequently, irinotecan and anlotinib chemotherapy was administered to the patient. After six cycles, the patient stopped the combined chemotherapy.
The patient had no history of acute or chronic infectious diseases, heart disease, hypertension or diabetes, or surgery other than laparoscopic radical rectum resection.
The patient did not have any relevant family medical history.
The patient was slightly underweight (body mass index 18.3 kg/m2). No other significant changes were detected.
An immunohistochemical pathology report showed CD117 (+), CK7 (-), CK5/6 (+), CK8/18 (+), P63 (+), P40 (+), S-100 (+), DOG-1 (+), and Calponin (+).
The patient underwent regular CT scans during his hospitalization.
Based on findings on hematoxylin and eosin sections and the patient’s clinical history, the patient was diagnosed with a poorly differentiated carcinoma of the esophagus.
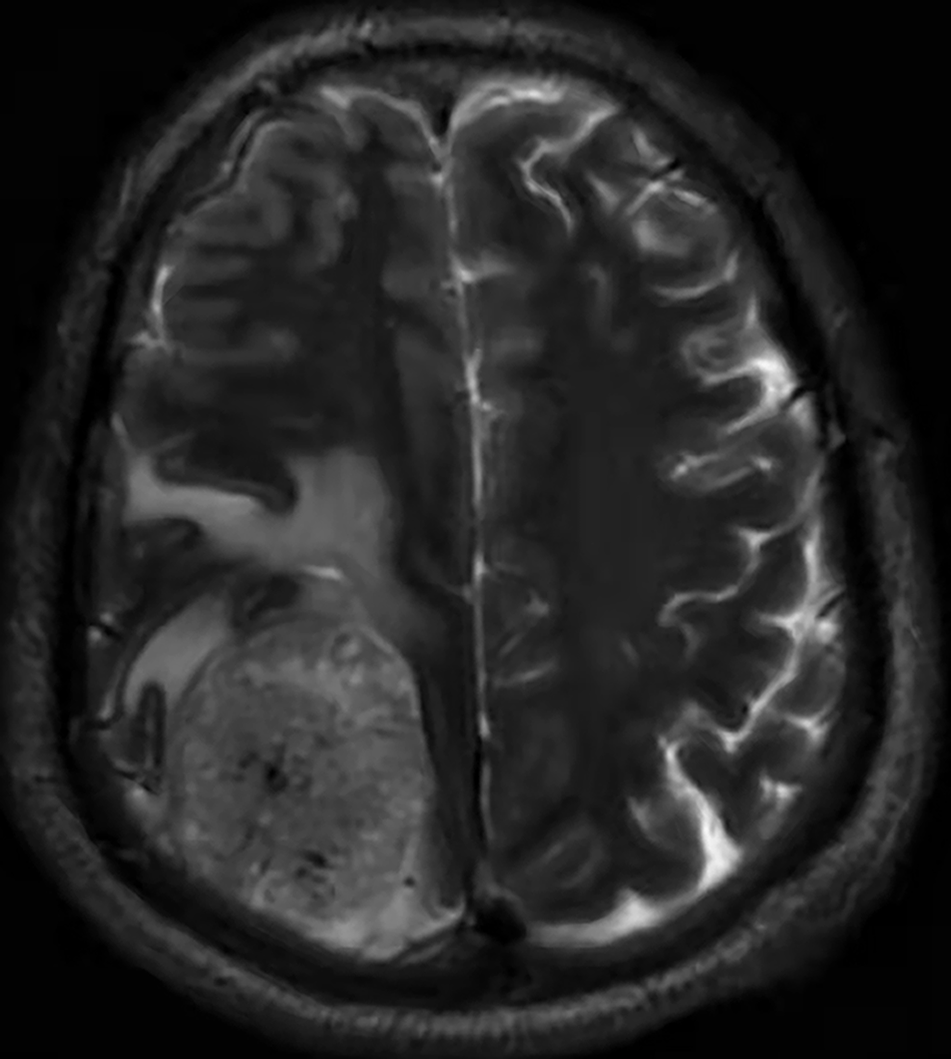
The patient was administered two cycles of chemotherapy including anti-PD-1, oxaliplatin, capecitabine, and anlotinib. On February 16, 2022, owing to mobility impairment of both lower extremities, the patient underwent cranial magnetic resonance imaging that revealed multiple abnormal signals in the brain. The largest was located in the right parietal lobe (Figure 4).
After a 3-mo follow-up, the patient passed away due to disease progression with brain metastases.
We report a case of esophageal cancer with anal metastasis after regular chemotherapy. Wu et al[5] conducted a study including patients from the SEER database diagnosed with esophageal cancer between 2010 and 2014. This study analyzed the distribution of different distant metastatic sites in 1470 patients and observed a total of 2243 distant metastasis. The liver was the most common site of metastasis (727, 32.4%), followed by distant lymph nodes (637, 28.4%), lung (459, 20.5%), bone (344, 15.3%), and brain (76, 3.4%). EACC is a very rare type of esophageal cancer[6]. The tendency of EACC to metastasize is roughly the same as that of adenoid cystic carcinoma (ACC). The probability of distant metastasis in ACC ranges from 40% to 50%[7] with the lung being the most common site (approximately 80%), followed by the bone and liver. Lymph node invasion is rare, and the probability of lymph node metastasis is generally lower than 10%[8]. Kaur et al[9] observed 22 EACC cases since 2004, for which the incidence of lung metastasis was 27.3%, and the rate of lymph node metastasis was 9.1%. In addition, from 35 cases of EACC in Japan analyzed by Sawada et al[10], only 1 of the 25 cases, in which the tumor invaded the submembranous or myometrial aura, showed lymph node metastasis.
The clinical manifestations and endoscopic manifestations of EACC are nonspecific. Biopsy specimens are often misdiagnosed as adenocarcinoma or squamous cell carcinoma as they are frequently too small, too shallow, and stored in compound carcinoma[8]. In the clinic, post-operative pathology and additional immunohistochemistry have become the gold standard for the diagnosis of EACC.
In terms of treatment, surgical resection remains the first choice for patients with EACC[7-10]. Chemotherapy and targeted immunotherapy can be reserved treatment options for patients with metastatic EACC; however, there is little reported experience of chemotherapy use in EACC. Some reports suggest that doxorubicin-based combination chemotherapy is effective for ACC of the salivary glands. For example, Petursson et al[11] used doxorubicin, cyclophosphamide, vincristine, and cisplatin chemotherapy to treat a case of EACC, and the patient achieved complete remission. In another case, a patient with pulmonary recurrence 5 years after EACC radical resection was administered cisplatin- or irinotecan-based chemotherapy, following which the patient's condition was stable for more than half a year. Radiation therapy can be used for localized disease in non-operable patients. More research is needed to support the formulation of treatment plans for EACC patients. A randomized open-label clinical trial[12] has also confirmed that compared to chemotherapy alone, the combination of nivolumab and chemotherapy significantly improves both overall survival and progression-free survival in patients. Kelly et al[13] also found similar results through clinical trials. This suggests that immunotherapy has become an indispensable treatment modality for esophageal adenocarcinoma. However, the specific treatment plan still needs to be selected based on individual patient circumstances and clinical advice from healthcare providers. Furthermore, when a patient complains of an anal bulge or finds blood in the stool[14], clinicians need to be aware of the possibilities of anal metastasis. Immunohistochemistry can help clinicians distinguish whether new growths are primary or metastatic, so as to formulate a more accurate treatment plan.
EACC is a relatively rare type of esophageal cancer. There are few comprehensive clinical reports, but many individual cases are reported. At present, surgical resection is still the main treatment. Chemotherapy and targeted therapy can be reserved for patients with metastatic EACC. Radiotherapy can be used for localized disease in non-operable patients. In this case, the patient was misdiagnosed following endoscopic puncture pathology. Postoperative pathology and immunohistochemistry confirmed the EACC diagnosis. Postoperative chemotherapy and immunotherapy were continued without radiotherapy. Finally, the patient developed brain metastases and achieved PD.
Thank you to Director Sun J for providing the clinical case, and gratitude to Xu L and Xu R for writing and revising the article.
| 1. | Pennathur A, Gibson MK, Jobe BA, Luketich JD. Oesophageal carcinoma. Lancet. 2013;381:400-412. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1956] [Cited by in RCA: 1961] [Article Influence: 163.4] [Reference Citation Analysis (5)] |
| 2. | Uhlenhopp DJ, Then EO, Sunkara T, Gaduputi V. Epidemiology of esophageal cancer: update in global trends, etiology and risk factors. Clin J Gastroenterol. 2020;13:1010-1021. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 116] [Cited by in RCA: 436] [Article Influence: 87.2] [Reference Citation Analysis (1)] |
| 3. | Domper Arnal MJ, Ferrández Arenas Á, Lanas Arbeloa Á. Esophageal cancer: Risk factors, screening and endoscopic treatment in Western and Eastern countries. World J Gastroenterol. 2015;21:7933-7943. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 554] [Cited by in RCA: 748] [Article Influence: 74.8] [Reference Citation Analysis (15)] |
| 4. | Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68:394-424. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53206] [Cited by in RCA: 55853] [Article Influence: 7979.0] [Reference Citation Analysis (132)] |
| 5. | Wu SG, Zhang WW, Sun JY, Li FY, Lin Q, He ZY. Patterns of Distant Metastasis Between Histological Types in Esophageal Cancer. Front Oncol. 2018;8:302. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 31] [Cited by in RCA: 60] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 6. | Bradley PJ. Adenoid cystic carcinoma evaluation and management: progress with optimism! Curr Opin Otolaryngol Head Neck Surg. 2017;25:147-153. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 40] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 7. | Nightingale J, Lum B, Ladwa R, Simpson F, Panizza B. Adenoid cystic carcinoma: a review of clinical features, treatment targets and advances in improving the immune response to monoclonal antibody therapy. Biochim Biophys Acta Rev Cancer. 2021;1875:188523. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 31] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 8. | Guo XF, Mao T, Gu ZT, Fang WT, Chen WH, Shao JC. Adenoid cystic carcinoma of the esophagus: report of two cases and review of the Chinese literature. Diagn Pathol. 2012;7:179. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 10] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 9. | Kaur J, Goyal S, Muzumder S, Bhasker S, Mohanti BK, Rath GK. Outcome of surgery and post-operative radiotherapy for major salivary gland carcinoma: ten year experience from a single institute. Asian Pac J Cancer Prev. 2014;15:8259-8263. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 22] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 10. | Sawada G, Moon J, Saito A, Odagiri K, Kimura Y, Takahashi G, Yamashita S, Inoue M, Irei T, Nakahira S, Shimizu Y, Tominaga H, Kuraoka K, Taniyama K, Hatanaka N. A case of adenoid cystic carcinoma of the esophagus. Surg Case Rep. 2015;1:119. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 13] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 11. | Petursson SR. Adenoid cystic carcinoma of the esophagus. Complete response to combination chemotherapy. Cancer. 1986;57:1464-1467. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 12. | Janjigian YY, Shitara K, Moehler M, Garrido M, Salman P, Shen L, Wyrwicz L, Yamaguchi K, Skoczylas T, Campos Bragagnoli A, Liu T, Schenker M, Yanez P, Tehfe M, Kowalyszyn R, Karamouzis MV, Bruges R, Zander T, Pazo-Cid R, Hitre E, Feeney K, Cleary JM, Poulart V, Cullen D, Lei M, Xiao H, Kondo K, Li M, Ajani JA. First-line nivolumab plus chemotherapy vs chemotherapy alone for advanced gastric, gastro-oesophageal junction, and oesophageal adenocarcinoma (CheckMate 649): a randomised, open-label, phase 3 trial. Lancet. 2021;398:27-40. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1962] [Cited by in RCA: 1904] [Article Influence: 476.0] [Reference Citation Analysis (1)] |
| 13. | Kelly RJ, Ajani JA, Kuzdzal J, Zander T, Van Cutsem E, Piessen G, Mendez G, Feliciano J, Motoyama S, Lièvre A, Uronis H, Elimova E, Grootscholten C, Geboes K, Zafar S, Snow S, Ko AH, Feeney K, Schenker M, Kocon P, Zhang J, Zhu L, Lei M, Singh P, Kondo K, Cleary JM, Moehler M; CheckMate 577 Investigators. Adjuvant Nivolumab in Resected Esophageal or Gastroesophageal Junction Cancer. N Engl J Med. 2021;384:1191-1203. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 469] [Cited by in RCA: 1091] [Article Influence: 272.8] [Reference Citation Analysis (0)] |
| 14. | Ciombor KK, Ernst RD, Brown G. Diagnosis and Diagnostic Imaging of Anal Canal Cancer. Surg Oncol Clin N Am. 2017;26:45-55. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 20] [Article Influence: 2.5] [Reference Citation Analysis (0)] |