Published online Jul 6, 2024. doi: 10.12998/wjcc.v12.i19.3767
Revised: April 27, 2024
Accepted: May 14, 2024
Published online: July 6, 2024
Processing time: 110 Days and 21.8 Hours
Arthroscopic rotator cuff repair is a common surgical treatment for rotator cuff injuries (RCIs). Although this procedure has certain clinical advantages, it requi
To investigate the effect of integrated traditional Chinese medicine and Western medicine (TCM-WM) under the multidisciplinary team (MDT) model on the postoperative recovery of patients undergoing arthroscopic surgery for RCIs.
This study enrolled 100 patients who underwent arthroscopic rotator cuff repair for RCIs at the Seventh People’s Hospital of Shanghai University of Traditional Chinese Medicine between June 2021 and May 2024. They were divided into a control group (n = 48) that received routine rehabilitation treatment and an experimental group (n = 52) that received TCM-WM under the MDT model (e.g., acupuncture, TCM traumatology and orthopedics, and rehabilitation). The results of the Constant–Murley Shoulder Score (CMS), Visual Analogue Scale (VAS), Shoulder Pain and Disability Index (SPADI), muscular strength evaluation, and shoulder range of motion (ROM) assessments were analyzed.
After treatment, the experimental group showed significantly higher CMS scores in terms of pain, functional activity, shoulder joint mobility, and muscular strength than the baseline and those of the control group. The experimental group also exhibited significantly lower VAS and SPADI scores than the baseline and those of the control group. In addition, the experimental group showed significantly enhanced muscular strength (forward flexor and external and internal rotator muscles) and shoulder ROM (forward flexion, abduction, and lateral abduction) after treatment compared with the control group.
TCM-WM under the MDT model improved shoulder joint function, relieved postoperative pain, promoted postoperative functional recovery, and facilitated the recovery of muscular strength and shoulder ROM in patients with RCIs who underwent arthroscopic rotator cuff repair.
Core Tip: This study explored the impact of integrated traditional Chinese medicine and Western medicine (TCM-WM) on the recovery of 100 patients with rotator cuff injuries (RCIs) who underwent arthroscopic rotator cuff repair. The control group underwent routine rehabilitation treatment, whereas the experimental group underwent TCM-WM under the multidisciplinary team model, including acupuncture and moxibustion, TCM traumatology and orthopedics, and rehabilitation. We confirmed that TCM–WM has significant clinical advantages in accelerating the recovery of patients with RCIs after arthroscopic surgery, particularly in improving shoulder joint function, pain, functional impairment, muscle strength, and shoulder joint range of motion. The results indicate the potential of TCM–WM as an alternative therapeutic option for patients with RCIs.
- Citation: Cao DP, Yin L, Wang YF, Liu BL. Application of multidisciplinary team-based integrated traditional Chinese medicine and Western medicine in rotator cuff injury patients undergoing arthroscopic surgery. World J Clin Cases 2024; 12(19): 3767-3775
- URL: https://www.wjgnet.com/2307-8960/full/v12/i19/3767.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i19.3767
The rotator cuff is composed of the supraspinatus, infraspinatus, subscapularis, and teres minor, all of which contribute to the dynamic and stable human shoulder joint structure[1,2]. Lesions in this area can cause shoulder pain, dysfunction, and limitations in daily activities. In particular, rotator cuff injury (RCI) is a common cause of rotator cuff lesions[3]. RCIs usually originate from trauma and are closely related to acute tears in young patients and degenerative tears in elderly patients[4,5]. According to epidemiological data, the risk of RCIs increases with age, ranging from as low as 9.7% in young patients to as high as 62.0% in patients aged > 80 years[6]. The management of RCIs is mainly conservative and surgical. Conservative treatment is mainly implemented in patients with mild to moderate RCIs. Although conservative treatment has a good curative effect, patients may experience significant systemic and local adverse reactions[7]. Surgical treatment, specifically, arthroscopic rotator cuff repair, is often performed in patients with a poor response after 3–6 months of conservative treatment or in those with large full-thickness rotator cuff tears[8]. Arthroscopic rotator cuff repair is superior to open surgery in reducing deltoid trauma, shortening hospital stay, and preventing postoperative joint stiffness. However, postoperative rehabilitation management is needed to ensure therapeutic efficacy[9,10]. This study analyzed the data of patients with RCIs who underwent arthroscopic rotator cuff repair to explore the influence of different rehabilitation management interventions on postoperative recovery.
Traditional Chinese medicine (TCM) classifies RCIs as “muscular rheumatism”, “shoulder arthralgia” and “tendon-muscle injury” and believes that the occurrence of the disease is strongly associated with “deficiency, evil, and blood stasis”[11]. Its internal cause is related to the deficiency of vital qi in patients, which occurs in old age and infirmity; lung-qi deficiency; liver-kidney deficiency; muscular malnutrition; and loss of joint lubrication. The external cause is related to external evil, strain, and trauma[12,13]. Acupuncture and moxibustion, among the commonly used treatment methods in TCM, offer clinical advantages, such as a simple procedure, remarkable effects, cost-effectiveness, safety, and no side effects[14]. It significantly relieves shoulder pain in patients with RCI through its analgesic activity[15]. The treatment principles for bone injury in TCM are restoring vital qi, removing blood stasis, dredging meridians, and eliminating pathogenic factors. The treatment schemes include treatment based on syndrome differentiation (Jinbi Decoction and manipulation therapy, such as three-step nine-manipulation for the shoulder) and external treatment like Wizi Powder hot compress therapy. This study explored the integration of characteristic TCM diagnosis and treatment, such as acupuncture and moxibustion, TCM oral administration and external treatments, and characteristic TCM techniques, into the multidisciplinary team (MDT) model that implements modern rehabilitation interventions to achieve the best curative effect after rotator cuff repair.
This study selected 100 patients with RCI admitted to the Seventh People’s Hospital of Shanghai University of Traditional Chinese Medicine from June 2021 to May 2024 as research subjects, including 48 who underwent routine rehabilitation treatment (control group) and 52 who underwent Traditional Chinese Medicine and Western medicine (TCM-WM) (experimental group) under the MDT model. TCM-WM included acupuncture and moxibustion, TCM traumatology and orthopedics, and rehabilitation. The two groups were clinically comparable, as the differences in general data were not statistically significant (P > 0.05).
Inclusion criteria: Patients meeting the diagnosis criteria for RCIs [acute trauma or chronic strain, shoulder pain, weakness, and limited range of motion (ROM)], with a confirmed diagnosis of RCI by magnetic resonance imaging; patients with RCIs eligible for arthroscopic repair; patients who can tolerate surgical anesthesia with no surgical contraindications and can cooperate with surgical treatment; patients who can actively cooperate with the postoperative rehabilitation program; patients who can undergo acupuncture and moxibustion, TCM external and oral therapeutic applications; and patients with sound cognitive function, normal expression skills, and no major underlying diseases.
Exclusion criteria: Frozen shoulder; huge, irreparable tears; glenohumeral osteoarthritis, upper limb peripheral nerve injury, or acromioclavicular joint arthritis; minor RCIs that can be treated conservatively; shoulder fracture, dislocation, and brachial plexus injury; obvious joint adhesions; joint instability; multiple injuries, such as fractures, including hairline fractures; mental illness or communication disorders; and intolerance or allergies to TCM.
The control group underwent routine rehabilitation treatment. The interventions included biceps brachii training, elbow flexion and extension, and pendulum exercises 2-8 d after surgery, wearing a shoulder joint abduction brace regularly, and practicing non-weight-bearing joint abduction and swinging. The exercises were performed 2–8 times a day, with an intensity suitable for patients without muscle fatigue.
The experimental group underwent TCM–WM under the MDT model, the interventions for which included acupuncture and moxibustion, TCM traumatology and orthopedics, and rehabilitation.
Acupuncture and moxibustion therapy: Following the principle that “by stimulating the meridians, diseases in the organs corresponding to the meridians can be treated”, the acupoints around the shoulder joint were selected: Jiansanzhen (Jianyu, Jianqian, and Jianzhen), Jianliao, Tianzong, Naoshu, and Ashi. Acupoints were selected along the meridian and at the distal end according to the location of the patient’s lesion, the Yuji acupoint of the Hand-Taiyin meridian was selected for anterior shoulder pain; in cases of acromion pain, the Sanjian acupoint of the Large Intestine Meridian of Hand–Yangming was selected; and for back pain, the Houxi acupoint of the Small Intestine Meridian of Hand–Taiyang was selected.
Treatment steps of warm-needle moxibustion of Lu’s acupuncture and moxibustion: The patient takes a sitting position during treatment. After routine disinfection, 0.30 mm × 40 mm disposable sterile acupuncture needles were quickly and vertically inserted 1.0–1.2 inches into the acupoints. After obtaining the needling response, twisting-twirling and reinforcing-reducing manipulations were performed at each acupoint for 1 min. Next, a moxa stick approximately 2 cm in length and 2 cm in diameter was inserted into the needle handle and then lit from below for moxibustion. A notched piece of paper was placed at the contact point between the needle body and the skin to prevent scalding. The whole treatment process lasted 30 min.
TCM prescription: Jinbi Decoction consists of Radix Astragali preparata (9 g), Codonopsis pilosula (12 g), Radix Angelicae Sinensis (9 g), Radix Paeoniae Alba preparata (12 g), Rhizoma Chuanxiong (12 g), Radix Rehmanniae (9 g), peach kernel (9 g), Radix Angelicae Pubescentis (9 g), olibanum (9 g), Trogopterus Dung (12 g), Radix Gentianae Macrophyllae (9 g), Rhizoma Cyperi (12 g), Radix Cyathulae (9 g), Lumbricus (9 g), and Radix Glycyrrhizae preparata (6 g). Preparation and administration: The drugs were decocted with water to a volume of 400 mL for warm administration twice daily (once in the morning and once in the evening), one dose a day. Additional preparations in case of concurrent syndromes: For cold: Aconiti Lateralis Radix praeparata (9 g), cinnamon (12g), asarum (9 g), and ginger (12g); for phlegm-dampness: Fructus Arctii (12 g), Rhizoma Pinelliae (12 g), Poria cocos (12 g), and Semen Plantaginis (9 g).
Manipulation therapy (three-step nine-manipulation for the shoulder): (1) Tendon regulation: Point kneading of acupoints, such as Jiaji, Jianjing, Tianzong, Jianyu, Quchi, and Hegu, is first performed, followed by rolling manipulation of the affected trapezius, supraspinatus, and deltoid; (2) bone setting: First, the affected shoulder is gradually pulled and extended in the abducent position, and then the affected limb is pulled and stretched after bending the elbow and lifting the head. Thereafter, pulling manipulation of the affected shoulder in the adduction position, internal and external rotation after abduction, and manipulation to the backward position were performed. The extension range is dependent on the patient’s tolerance, and the manipulations are performed 1–2 times in each direction; and (3) pulse dredging: The massage therapist rubs the patient’s affected shoulder with the palms, buckles the patient’s wrist, and rotates the affected shoulder in the abduction position. The massage therapist then holds the wrist of the patient’s affected limb with both hands and shakes the patient’s affected shoulder by pulling and shaking manipulations. The above intervention was performed step by step according to the patient’s postoperative recovery and was performed 2–3 times a week as appropriate.
Hot compresses and acupoint application were performed using Wuzi Powder and Sanxiang Powder. Wuzi Powder consists of Raphani Semen, Fructus Psoraleae, Perillae Fructus, white mustard seeds, and Cuscuta chinensis Lam. Sanxiang Powder is composed of Radix Aucklandiae, Flos Caryophylli, Fructus Foeniculi, Radix Angelicae Dahuricae, and Cortex Cinnamomi.
The rehabilitation treatment plan was developed based on the MDT model. In the acute edema stage (1–7 d after surgery), patients underwent interventions, such as ice compress, laser therapy, and muscular pumps (fist-clenching and ball-pinching), to reduce swelling and relieve pain. They were also instructed on shoulder pendulum movements, active movements of the elbow and wrist joints, and passive activity training (angle of passive abduction ≥ 30°). At 2–6 wk postoperatively, the following training regimen was performed to promote the healing of rotator cuff tissue and prevent adhesion and muscle atrophy of the shoulder joint and surrounding tissue: relaxing the muscles around the shoulder joint; continuing passive activity training of the shoulder joint (angle of passive abduction ≥ 30°); performing scapular control exercises (isometric contraction of muscles around the scapula). At 7–12 wk postoperatively, active movement and muscular strength training of the rotator cuff muscle were intensified to promote shoulder joint stability and restore shoulder ROM. Joint ROM training was continued to achieve maximum all-angle ROM in all planes and at the furthest possible range with little to no pain. At weeks 6–8, a gradual transition from passive movement training to rotator cuff muscle group-assisted activity training was initiated. Starting from the eighth week, the intensity of muscular strength training of the rotator cuff and resistance training of the rotator cuff muscle group and biceps brachii were increased. Shoulder proprioception, nerve control, and shoulder joint functional training [activities of daily living (ADL) training] were performed.
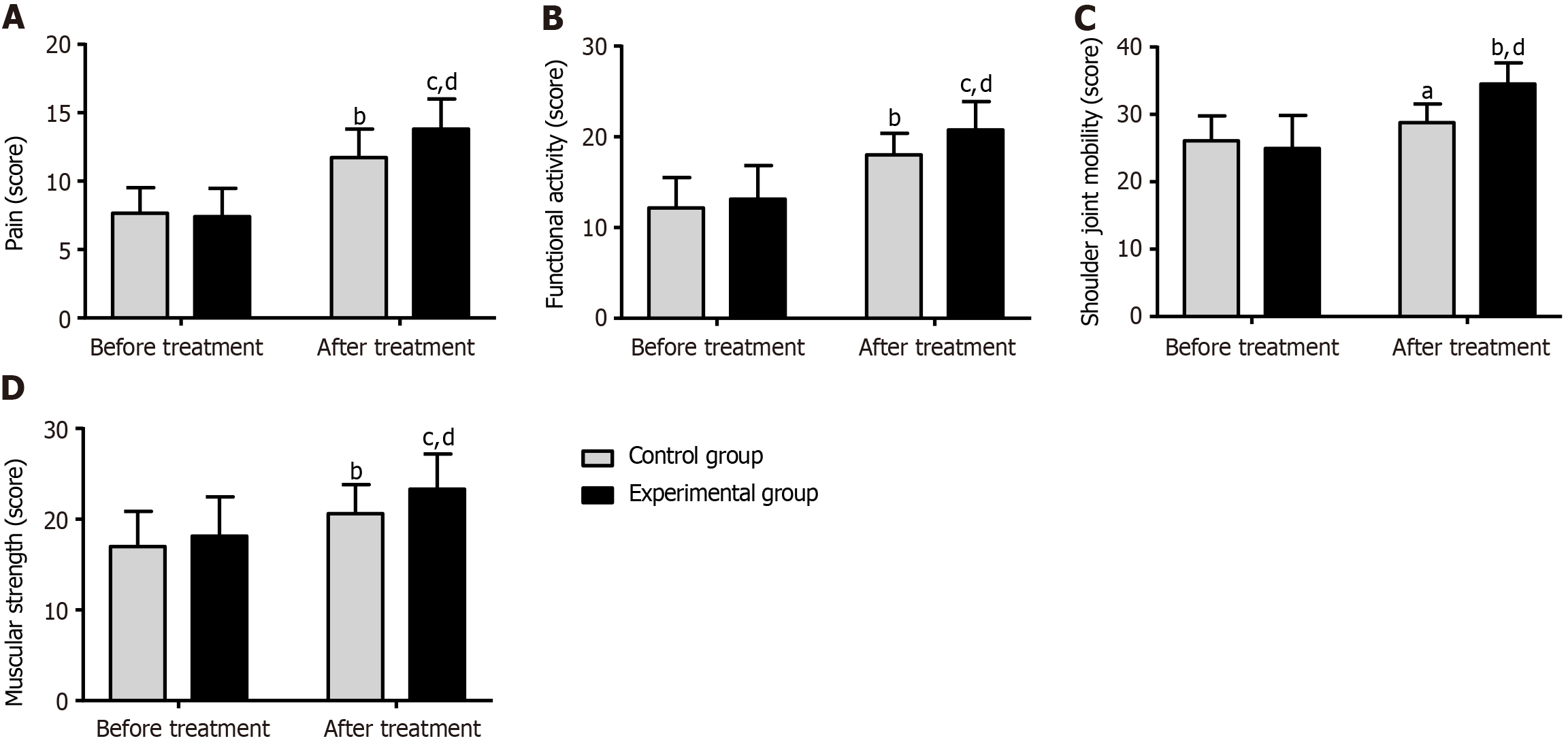
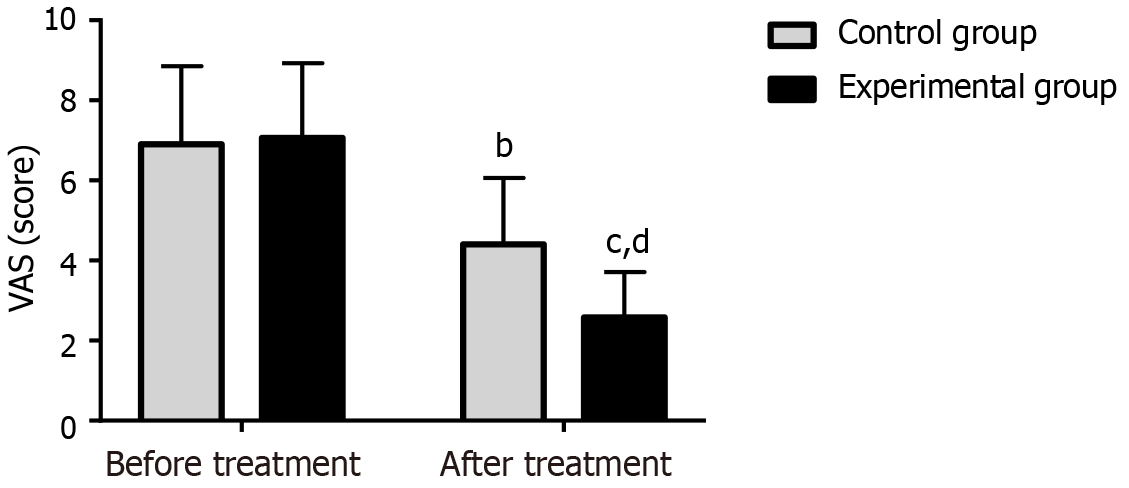
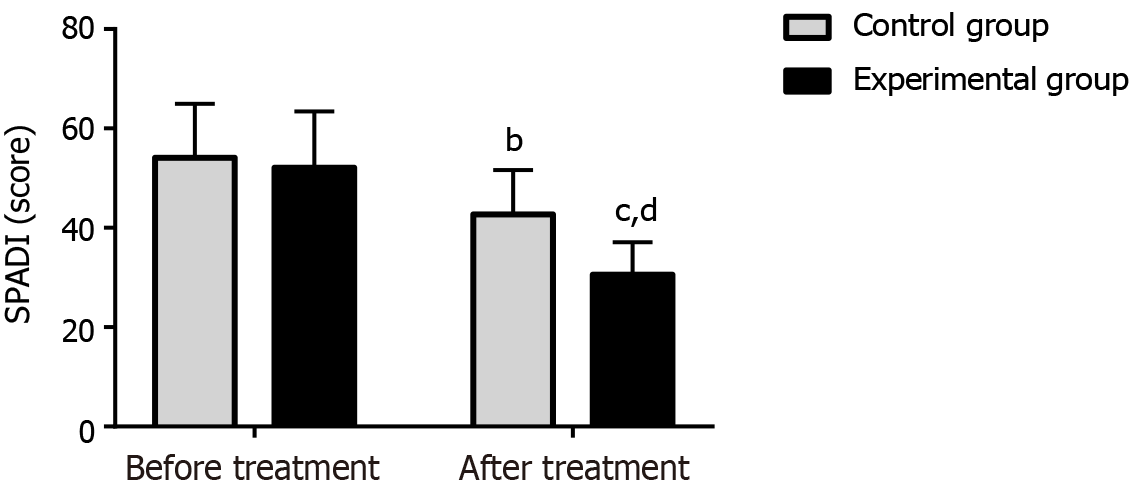
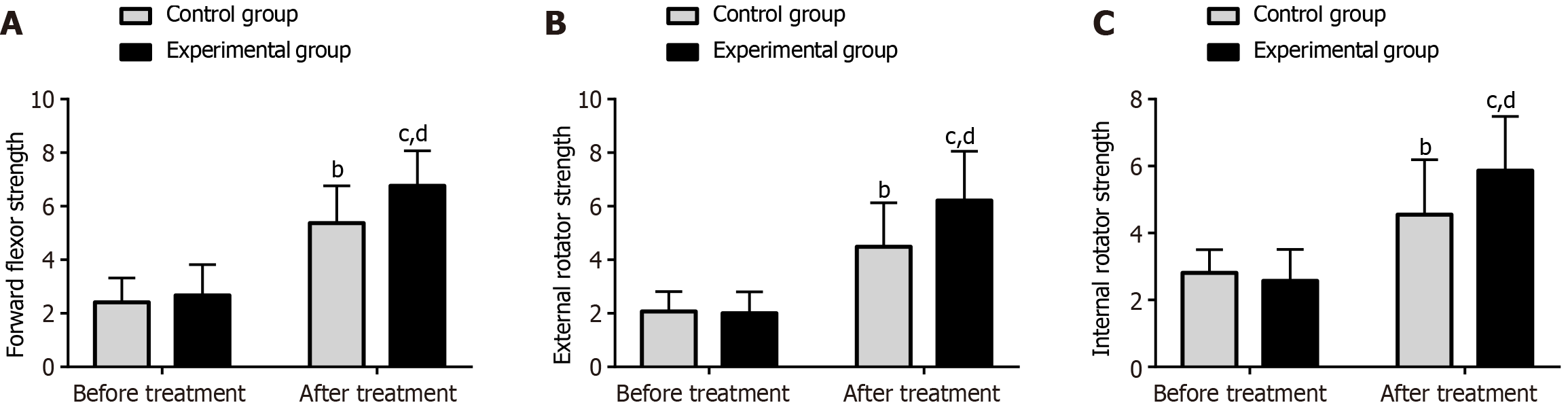
(1) Shoulder joint function assessment. Shoulder function levels were assessed using the Constant–Murley Score (CMS) before and after treatment, mainly from the aspects of pain (15 points), functional activity (15 points), shoulder joint mobility (40 points), and muscular strength (25 points). A high score indicates a well-functioning shoulder; (2) Pain score. The pain intensity experienced by the subjects was evaluated using the Visual Analogue Scale (VAS; score range: 0–10); the score is proportional to the pain intensity experienced; (3) the Shoulder Pain and Disability Index (SPADI; score range: 0–130) was used for assessment, with a higher score corresponding to greater shoulder pain and dysfunction; (4) muscular strength evaluation. The muscular strength of patients before and after treatment, as demonstrated by forward flexion and external and internal rotation, was measured using the muscle condition rapid measurement system; and (5) shoulder ROM. ROM (forward flexion, abduction, and lateral rotation) was evaluated using a protractor with patients in a normal sitting position. The long axis of the humerus was used as the moving arm during the measurement. In measuring shoulder joint forward flexion and abduction, the acromion was used as the axis, and the midline of the body was used as the fixed arm. In the lateral abduction measurement, the olecranon was used as the axis.
The measurement data are expressed as mean ± SD of the mean, the between- and within-group (before and after treatment) comparisons of which were performed using the independent sample and paired t-tests, respectively. Count data are expressed as number (percentage), and between-group comparisons were performed using the χ2 test. The data were analyzed using SPSS 21.0. Statistical significance was indicated by P < 0.05 for all analyses.
No significant differences were observed between the experimental and control groups in sex, age, disease course, lesion site, cause of injury, hypertension, and hyperglycemia (P > 0.05) (Table 1).
| Indicators | Control group (n = 48) | Experimental group (n = 52) | χ2/t | P value |
| Sex (male/female) | 26/22 | 32/20 | 0.557 | 0.456 |
| Age (yr) | 46.58 ± 7.51 | 47.44 ± 7.69 | 0.565 | 0.573 |
| Disease course (months) | 10.71 ± 2.51 | 10.13 ± 2.00 | 1.283 | 0.203 |
| Lesion site (left shoulder/right shoulder/both shoulders) | 22/15/11 | 26/20/6 | 2.362 | 0.307 |
| Cause of injury (traffic accidents/sports/acupuncture) | 28/17/3 | 30/15/7 | 1.637 | 0.441 |
| Hypertension (with/without) | 12/36 | 10/42 | 0.484 | 0.487 |
| Hyperglycemia (with/without) | 5/43 | 4/48 | 0.226 | 0.634 |
The two groups showed no significant differences in pretreatment scores for functional activity, shoulder joint mobility, and muscular strength (P > 0.05). However, the scores of both groups significantly increased posttreatment (P < 0.05), with significantly higher scores in the experimental group than in the control group (P < 0.05) (Figure 1).
No significant inter-group difference was observed in pretreatment VAS scores (P > 0.05). The scores decreased significantly after treatment (P < 0.05), with a more significant reduction observed in the experimental group than in the control group (P < 0.05) (Figure 2).
The pretreatment SPADI scores were comparable between the two patient groups (P > 0.05). However, the SPADI scores decreased significantly in both groups after treatment (P < 0.05), with significantly lower SPADI scores in the experimental group (P < 0.05) (Figure 3).
The two groups of patients showed no notable differences in muscular strength of the forward flexor and external and internal rotator muscles before treatment (P > 0.05). After treatment, the scores of both groups increased significantly (P < 0.05), with higher scores in the experimental group than in the control group (P < 0.05) (Figure 4).
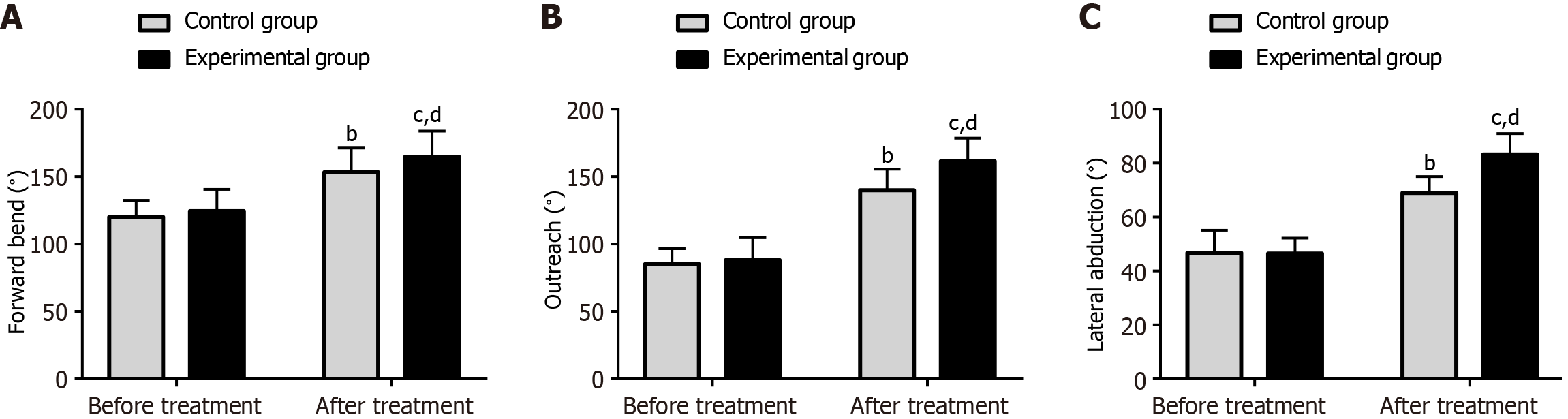
No significant differences were observed in pretreatment ROM between the two groups in terms of forward flexion, abduction, and lateral abduction (P > 0.05). After treatment, the ROM of both groups improved significantly (P < 0.05), with more significant improvements observed in the experimental group (P < 0.05) (Figure 5).
The basic pathogenesis of RCIs in the context of TCM involves the obstruction of shoulder meridians and the dystrophy of bones and muscles. Although the lesion is in the shoulder, it can cause discomfort in the neck, back, and arms[16]. Moreover, RCIs are predominantly observed in elderly patients, who are at greater perioperative risk and exhibit longer postoperative recovery times. Therefore, improper management of the treatment and rehabilitation of patients with RCI can cause various problems, such as prolonged hospital stays, increased medical costs, delayed recovery, long-term chronic pain, and decreased satisfaction[17]. We believe that scientific, effective, and timely management should be provided for patients with RCIs undergoing arthroscopic rotator cuff repair to minimize the risk of the abovementioned problems and ensure maximum therapeutic efficacy.
In this study, both groups of patients with RCIs underwent arthroscopic rotator cuff repair, with the control group undergoing routine rehabilitation treatment and the experimental group undergoing TCM-WM under the MDT model, mainly including acupuncture and moxibustion, TCM orthopedics and traumatology, and rehabilitation. The therapeutic mechanism of the Jinbi Decoction administered in this study involves supplementing qi and removing stasis. The Astragalus membranaceus and C. pilosula components of this prescription can benefit qi, replenish blood, and promote blood circulation. Angelica sinensis, Ligusticum Chuanxiong, and peach kernel promote blood circulation and remove blood stasis, while Trogopterus Dung and Lumbricus can dredge channels, reduce swelling, and relieve pain. Rhizoma Cyperi is mainly used for regulating qi, promoting blood circulation, and relieving arthralgia. Radix Gentianae Macrophyllae can dispel wind and eliminate dampness, while Radix Paeoniae Alba and Radix Glycyrrhizae can effectively relieve spasms and pain. Achyranthes bidentata can strengthen the waist and tonify the kidney, promote blood circulation, and remove blood stasis. The combination of these compounds can restore healthy qi, remove blood stasis, dredge meridians, and eliminate evil[18-22]. We found that the CMS scores for pain, functional activity, shoulder joint mobility, and muscular strength improved significantly in the experimental group after treatment, higher than the baseline and those in the control group, indicating that the administration of TCM-WM in patients with RCIs under the MDT model is beneficial for improving shoulder joint function. This may be because, in addition to rehabilitation, the experimental group also underwent acupuncture and moxibustion, was administered the Jinbi Decoction, and received manipulation therapy. Furthermore, the efficacy of TCM treatment for RCIs has been previously demonstrated[23]. Yang et al[24] found that warm-needle moxibustion relieved limb spasticity in patients with post-stroke spasticity and improved their motor function and ADL, which is similar to our findings.
Pain assessment revealed that the posttreatment VAS scores in the experimental group were significantly lower than the baseline and those in the control group, demonstrating the significant postoperative pain relief exerted by TCM-WM under the MDT model for patients with RCI who underwent arthroscopic rotator cuff repair. A systematic review and meta-analysis found that manipulation therapy induces pain relief in patients with rotator cuff tendinopathy, which is similar to our findings[25]. The posttreatment SPADI scores in the experimental group were significantly lower than the baseline and those in the control group, indicating that TCM-WM under the MDT model can effectively mitigate shoulder pain and dysfunction in patients with RCI. In particular, warm-needle moxibustion may have significantly promoted upper limb mobility and reduced pain. The therapeutic mechanism may be related to the upregulated secretion of opioid peptides, which are important neurohormones in the body that play a crucial role in pain transmission in the nervous system. Acupuncture stimulation increases the concentration of endogenous opioid peptides in tissues, thereby increasing the pain threshold, promoting analgesia, and correcting inflammatory changes around the affected tissues. In addition, warm-needle moxibustion combines the stimulating effects of acupuncture and moxibustion to synergistically stimulate corresponding acupoints, meridians, and moxibustion, thereby contributing significantly to therapeutic efficacy. The analysis of muscular strength (forward flexor and external and internal rotator muscles) revealed that the experimental group showed significantly better performance and improvement in muscular strength than the control group, indicating the superior therapeutic effect of TCM–WM under the MDT model on muscular strength rehabilitation. The experimental group also significantly improved posttreatment ROM in the aspects of flexion, abduction, and lateral abduction after treatment, compared with the control group. Therefore, TCM–WM under the MDT model can significantly promote the recovery of various aspects of ROM in patients with RCIs. Zhao et al[26] reported that warm-needle therapy and acupuncture relieved pain in patients with post-stroke hemiplegic shoulder pain and helped improve ROM, which is in agreement with our results.
This study has some limitations. First, the small sample and single-centered study design may have introduced selection bias, which would affect the accuracy and universality of the results. Second, the factors affecting the postoperative recovery effect of patients with RCIs who underwent arthroscopic rotator cuff repair were not analyzed. The current findings need to be confirmed by further studies with larger datasets to ensure the robustness of the RCI management model. Third, the long-term impact of the two treatment methods on the recovery of patients was not examined. Future studies should validate the outcomes, especially those for TCM–WM under the MDT model. Future studies should address these aspects to confirm the reliability of the current findings.
This study demonstrated that TCM–WM under the MDT model significantly contributes to the recovery of shoulder joint function, postoperative and shoulder joint pain relief, mitigation of dysfunction, and enhancement of muscular strength and ROM. TCM–WM exhibits potential as an effective therapeutic clinical application for RCI.
| 1. | Aguirre K, Mudreac A, Kiel J. Anatomy, Shoulder and Upper Limb, Subscapularis Muscle. 2023 Aug 28. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. [PubMed] |
| 2. | Sangwan S, Green RA, Taylor NF. Stabilizing characteristics of rotator cuff muscles: a systematic review. Disabil Rehabil. 2015;37:1033-1043. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 31] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 3. | Stogicza AR, Peng P. Cryoanalgesia for shoulder pain: a motor-sparing approach to rotator cuff disease. Reg Anesth Pain Med. 2022;47:576-580. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 7] [Reference Citation Analysis (0)] |
| 4. | Monica J, Vredenburgh Z, Korsh J, Gatt C. Acute Shoulder Injuries in Adults. Am Fam Physician. 2016;94:119-127. [PubMed] |
| 5. | Keener JD, Patterson BM, Orvets N, Chamberlain AM. Degenerative Rotator Cuff Tears: Refining Surgical Indications Based on Natural History Data. J Am Acad Orthop Surg. 2019;27:156-165. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 79] [Article Influence: 13.2] [Reference Citation Analysis (0)] |
| 6. | Codding JL, Keener JD. Natural History of Degenerative Rotator Cuff Tears. Curr Rev Musculoskelet Med. 2018;11:77-85. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 47] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 7. | Ranebo MC, Björnsson Hallgren HC, Holmgren T, Adolfsson LE. Surgery and physiotherapy were both successful in the treatment of small, acute, traumatic rotator cuff tears: a prospective randomized trial. J Shoulder Elbow Surg. 2020;29:459-470. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 46] [Article Influence: 9.2] [Reference Citation Analysis (0)] |
| 8. | Thigpen CA, Shaffer MA, Gaunt BW, Leggin BG, Williams GR, Wilcox RB 3rd. The American Society of Shoulder and Elbow Therapists' consensus statement on rehabilitation following arthroscopic rotator cuff repair. J Shoulder Elbow Surg. 2016;25:521-535. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 113] [Cited by in RCA: 129] [Article Influence: 14.3] [Reference Citation Analysis (0)] |
| 9. | Di Benedetto P, Mancuso F, Tosolini L, Buttironi MM, Beltrame A, Causero A. Treatment options for massive rotator cuff tears: a narrative review. Acta Biomed. 2021;92:e2021026. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 9] [Reference Citation Analysis (0)] |
| 10. | Guity MR, Sobhani Eraghi A, Hosseini-Baharanchi FS. Early postoperative pain as a risk factor of shoulder stiffness after arthroscopic rotator cuff repair. J Orthop Traumatol. 2021;22:25. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 13] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 11. | Zhang X, Zhou G, Gu Z, Luo M, Liang G. Research Progress of TCM Therapy for Rotator Cuff Injury. Comb Chem High Throughput Screen. 2024;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Reference Citation Analysis (0)] |
| 12. | Ye C, Zhang W, Wang S, Jiang S, Yu Y, Chen E, Xue D, Chen J, He R. Icariin Promotes Tendon-Bone Healing during Repair of Rotator Cuff Tears: A Biomechanical and Histological Study. Int J Mol Sci. 2016;17. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 20] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 13. | Kang L, Liu P, Peng A, Sun B, He Y, Huang Z, Wang M, Hu Y, He B. Application of traditional Chinese therapy in sports medicine. Sports Med Health Sci. 2021;3:11-20. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 6] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 14. | Tang H, Luo F, Fan H, Huang L, Liao S, Yu W, Chen Y, Qin X, Chen J. Acupuncture and manual therapy for rotator cuff tears: A protocol for systematic review and meta analysis. Medicine (Baltimore). 2020;99:e20377. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 15. | Wang IL, Chen YM, Hu R, Wang J, Li ZB. Effect of Acupuncture on Muscle Endurance in the Female Shoulder Joint: A Pilot Study. Evid Based Complement Alternat Med. 2020;2020:9786367. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 16. | Liu S, Liu JT, Chen L, Fan TY, Cui XJ, Cheng SD, Chen YJ, Shi Q, Xue CC, Li XF. Efficacy of five-step shoulder manipulation for rotator cuff-related shoulder pain: protocol for a multicenter randomized controlled trial. Trials. 2023;24:498. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 17. | Tashjian RZ. Epidemiology, natural history, and indications for treatment of rotator cuff tears. Clin Sports Med. 2012;31:589-604. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 328] [Cited by in RCA: 447] [Article Influence: 34.4] [Reference Citation Analysis (0)] |
| 18. | Xu J, Zhang Z, Zhou K, Li Y, Wan J, Mao T, Ji X, Liu J, Lin Q. Integration of network pharmacology and molecular docking technology reveals the mechanism of the herbal pairing of Codonopsis Pilosula (Franch.) Nannf and Astragalus Membranaceus (Fisch.) Bge on chronic heart failure. Ann Palliat Med. 2021;10:7942-7959. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 19. | Liu L, Li H, Tan G, Ma Z. Traditional Chinese herbal medicine in treating amenorrhea caused by antipsychotic drugs: Meta-analysis and systematic review. J Ethnopharmacol. 2022;289:115044. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 8] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 20. | Feng L, Liu WK, Deng L, Tian JX, Tong XL. Clinical efficacy of aconitum-containing traditional Chinese medicine for diabetic peripheral neuropathic pain. Am J Chin Med. 2014;42:109-117. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 35] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 21. | Jia N, Li Y, Wu Y, Xi M, Hur G, Zhang X, Cui J, Sun W, Wen A. Comparison of the anti-inflammatory and analgesic effects of Gentiana macrophylla Pall. and Gentiana straminea Maxim., and identification of their active constituents. J Ethnopharmacol. 2012;144:638-645. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 56] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 22. | Hu G, Li Z, Li H, Guan H. Clinical Observation on the Treatment of Rotator Cuff Injury with Modified Buyang Huanwu Decoction and Rotator Cuff Repair. J Healthc Eng. 2021;2021:3088160. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |
| 23. | Walker J 3rd, Dreher FL. Acupuncture: Evidence-Based Treatment in the Rehabilitation Setting. Phys Med Rehabil Clin N Am. 2020;31:699-717. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 24. | Yang L, Tan JY, Ma H, Zhao H, Lai J, Chen JX, Suen LKP. Warm-needle moxibustion for spasticity after stroke: A systematic review of randomized controlled trials. Int J Nurs Stud. 2018;82:129-138. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 29] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 25. | Desjardins-Charbonneau A, Roy JS, Dionne CE, Frémont P, MacDermid JC, Desmeules F. The efficacy of manual therapy for rotator cuff tendinopathy: a systematic review and meta-analysis. J Orthop Sports Phys Ther. 2015;45:330-350. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 89] [Article Influence: 8.9] [Reference Citation Analysis (0)] |
| 26. | Zhao H, Nie W, Sun Y, Li S, Yang S, Meng F, Zhang L, Wang F, Huang S. Warm Needling Therapy and Acupuncture at Meridian-Sinew Sites Based on the Meridian-Sinew Theory: Hemiplegic Shoulder Pain. Evid Based Complement Alternat Med. 2015;2015:694973. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 14] [Article Influence: 1.4] [Reference Citation Analysis (0)] |