Published online Jun 26, 2024. doi: 10.12998/wjcc.v12.i18.3629
Revised: April 21, 2024
Accepted: May 11, 2024
Published online: June 26, 2024
Processing time: 87 Days and 23.9 Hours
The midpoint transverse process to pleura (MTP) block, a novel technique for thoracic paravertebral block (TPVB), was first employed in laparoscopic renal cyst decortication.
Thoracic paravertebral nerve block is frequently employed for perioperative analgesia during laparoscopic cyst decortication. To address safety concerns associated with TPVBs, we administered MTP blocks in two patients prior to administering general anesthesia for laparoscopic cyst decortication. The MTP block was performed at the T9 level under ultrasound guidance, with 20 mL of 0.5% ropivacaine injected. Reduced sensation to cold and pinprick was observed from the T8 to T11 dermatome levels. Immediately postoperative Numeric Pain Rating Scale scores were 0/10 at rest and on movement, with none exceeding a mean 24 h numeric rating scale > 3.
MTP block was effective technique for providing postoperative analgesia for patients undergoing laparoscopic renal cyst decortication.
Core Tip: In this study, we successfully implemented midpoint transverse process to pleura (MTP) block for postoperative analgesia in two patients undergoing laparoscopic renal cyst decortication. The MTP block was performed at the T9 level under ultrasound guidance, with 20 mL of 0.5% ropivacaine injected. Reduced sensation to cold and pinprick was observed from the T8 to T11 dermatome levels. Immediately postoperative Numeric Pain Rating Scale scores were 0/10 at rest and on movement, with none exceeding a mean 24 h numeric rating scale > 3. In summary, MTP block was effective technique for providing postoperative analgesia for patients undergoing laparoscopic renal cyst decortication.
- Citation: He WJ, Xu WX, Zhang XD, Chen Y, He SY, Wei XQ, Huang XL. Midpoint transverse process to pleura block for postoperative analgesia following laparoscopic renal cyst decortication: Two case reports. World J Clin Cases 2024; 12(18): 3629-3635
- URL: https://www.wjgnet.com/2307-8960/full/v12/i18/3629.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i18.3629
Laparoscopic renal cyst decortication is a minimally invasive procedure that is used to treat symptomatic kidney cysts[1]. While this surgical technique has several advantages, such as smaller incisions and faster recovery time, compared to traditional open surgeries, patients may still experience postoperative pain[2]. Therefore, it is imperative to implement appropriate pain management strategies to effectively alleviate patients' postoperative pain and optimize their overall recovery experience.
In 2017, Costache et al[3] introduced the midpoint transverse process to pleura (MTP) block as a novel thoracic paravertebral block (TPVB) technique. The MTP block involves injecting at the midpoint between the transverse process and the pleura, eliminating the need to identify superior costo-transverse ligament (SCTL), while ensuring a greater distance from the pleura compared to traditional thoracic paravertebral blockade. The MTP block was initially employed in breast surgery[3,4]. MTP block is effective in reducing chest and back pain, making it a suitable option for managing rib fractures and providing thoracoscopic analgesia[5,6]. By utilizing MTP block, anaesthesiologists can effectively target and block specific nerve pathways involved in transmitting pain signals from the surgical site. Abdelbaser et al[7] imp
Case 1: A 74-year-old Chinese man presented to the clinic with episode of gross hematuria for 3 years and recurred symptoms for 1 d.
Case 2: A 44-year-old male patient of Chinese man was diagnosed with a right renal cyst that had been present for two months.
Case 1: The patient had episode of gross hematuria for 3 years, the symptoms of which had recurred in the 1 d prior to admission. The symptoms were characterized by pale red urine with dark red blood clots, while pyuria, dysuria, frequency, and urgency were notably absent.
Case 2: The patient reported that a right kidney cyst was found by ultrasound (US) examination in another hospital 2 months ago. Occasionally, there was intermittent swelling in the right flank region, while lumbago, hematuria, frequency, and urgency were notably absent.
Case 1: The patient has been diagnosed with hypertension for more than 10 years. Oral nifedipine is used to control the symptoms. The patient has been diagnosed with bilateral cataracts for more than 1 year.
Case 2: The patient has a history of being a carrier of the hepatitis B virus, although specific details remain undisclosed.
The two patients did not have any pertinent familial history of cancer or chronic illness.
Physical examination in two patients revealed no tenderness in the bilateral rib angles and ureter regions, and no tenderness on percussion in the bilateral renal regions. In addition, there were no bladder fullness, deep tenderness, or rebound pain.
Case 1: The blood routine analysis showed a white blood cell count of 7.00 × 109/L and hemoglobin concentration of 147 g/L. The routine urine analysis indicated leucocyte presence at level -, and urine latent blood presence at level 1+. The urine culture result confirmed the presence of no bacterial growth in the sample.
Case 2: The laboratory analysis of the patient yielded no discernible abnormalities.
Case 1: Ultrasonography revealed a slightly enlarged right kidney with aberrant morphology, and multiple cystic masses measuring up to 84 mm × 56 mm × 42 mm were identified within the renal parenchyma with Cystic mass with thin smooth wall, clear boundary, good internal sound permeability, enhanced posterior echo, no obvious blood flow signal inside.
Case 2: Ultrasound revealed that the right kidney exhibits normal dimensions and morphology, and a cyst in the central parenchyma of the right kidney. The cyst was approximately 69 mm × 62 mm × 37 mm in size with Cystic mass with thin smooth wall, clear boundary, good internal sound permeability, enhanced posterior echo, no obvious blood flow signal inside.
Postoperative pathology in two patients confirmed that the final diagnosis were simple renal cysts.
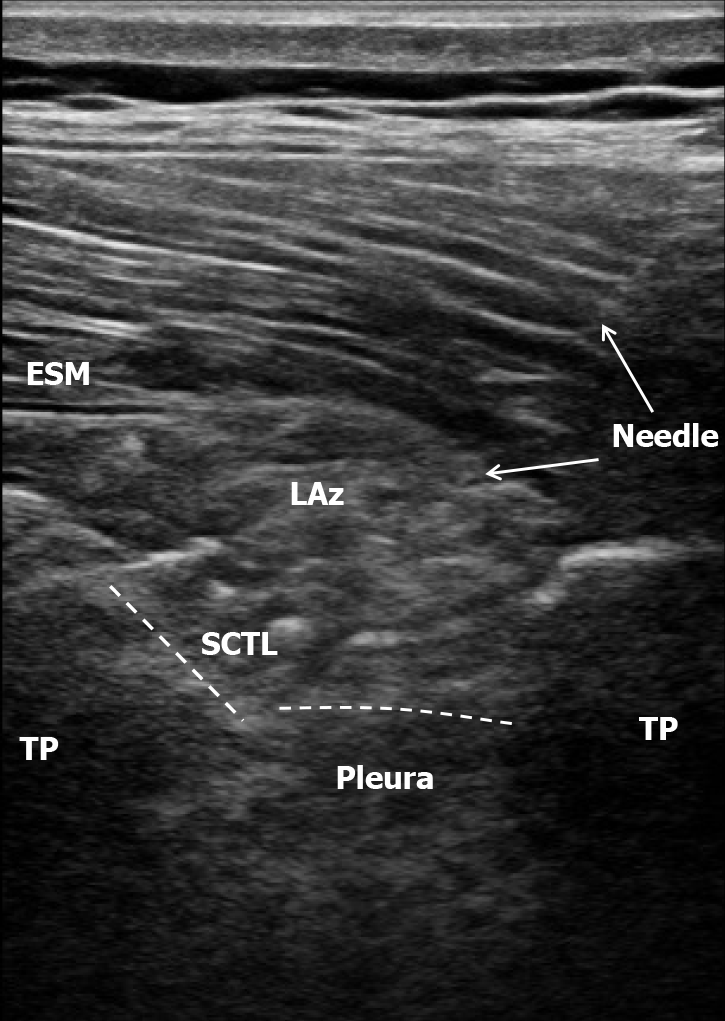
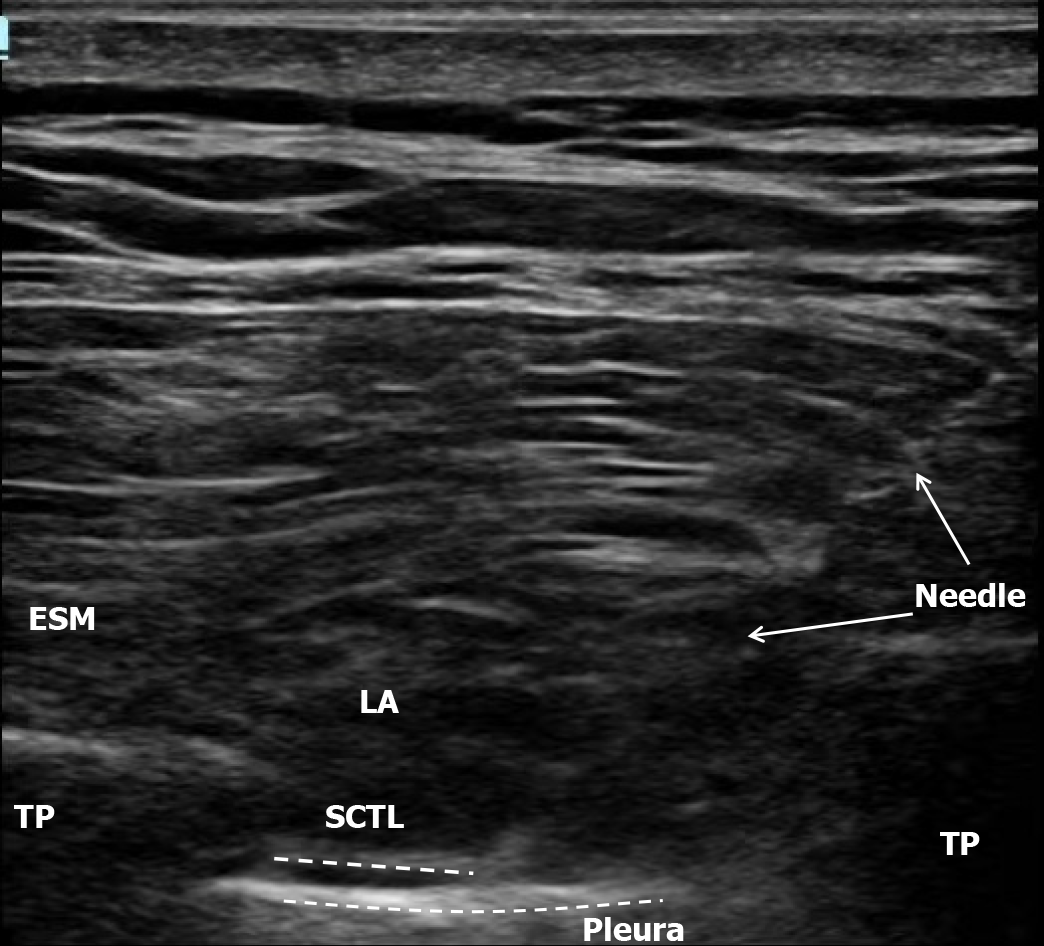
Case 1: The patient underwent standard monitoring upon arrival in the operating room. After establishing venous access, sedation was achieved using 1 mg of midazolam and 5 μg of intravenous sufentanil. The patient was instructed to maintain the right lateral decubitus position throughout the procedure. The thoracic spinous processes from T1 to T9 were carefully palpated and subsequently marked. MTP block was initiated between the right T9-10 segments under the guidance of a 6 to 13 MHz linear US probe (Mindray, Te7, Guangdong, China). The needle (80 mm 20-gauge block needle KDL, Wenzhou, Zhejiang Province, China) tip was accurately positioned at the midpoint between the transverse process and pleura, and a precise injection of 20 mL of 0.5% ropivacaine was administered at T9-10. Local anaesthetic spread was observed using US during the injection. We observed consistent downwards displacement of the pleura, without detected increase in the erector spinae plane (ESP) at the T9-10 level (Figure 1). Sensory evaluation was conducted at 5-min intervals using a chilled swab and a blunt 22 G needle tip along the posterior scapular line, the mid-axillary line, and the mid-clavicular line. A decrease in the sensation of the T8-T11 dermatomes was observed 20 min after the initiation of MTP block. Anaesthesia was subsequently induced using 160 mg of propofol, 40 μg of sufentanil, and 80 mg of rocuronium. The combination of propofol and remifentanil was administered to achieve sedation and analgesia during intubation under general anaesthesia (GA).
Patients underwent traditional three-port laparoscopic renal cyst decortication treatment. After endotracheal intubation under general anesthesia, the patient was positioned in a 90° left lateral decubitus position on the left side. The 10-mm camera port incision, measuring 2 cm in length, was positioned 2 cm above the iliac crest along the midaxillary line. The pneumoperitoneum was obtained using the open technique and, two standard 5-mm operating ports were created 2 cm below the rib margin along the posterior axillary line and 2 cm below the anterior axillary line at rib level twelve respectively. Under laparoscopic guidance, the renal perirenal fascia and adipose capsule were dissected using an ultrasonic knife until adequate excision of the cyst walls was achieved. Following confirmation of no active bleeding, intraperitoneal drainage tube placement was performed through retroperitoneum via trocars. The trocar incisions were then disinfected with alcohol swabs and closed in layers using sutures.
The surgical procedure lasted for a duration of 123 min, during which general anesthesia was administered for a period of 158 min. Propofol was utilized at a dosage of 970 mg, in conjunction with remifentanil at a dose of 2.1 mg throughout the operation. As preemptive analgesia, sufentanil was administered 5 min prior to the conclusion of the surgery at a dose of 5 µg. Following completion of the surgical intervention, patients were transferred to the postanesthesia care unit (PACU) for postoperative recovery.
Case 2: The patients underwent preoperative MTP block prior to undergoing traditional three-hole laparoscopic renal cyst decortication treatment. The planned multimodal analgesia regimen included a 9-level MTP block and GA. MTP block was performed under US guidance, and the distance between the location of the block and the posterior margin of the transverse process was determined to be 0.5 cm. Following the injection of 20 mL of 0.5% ropivacaine, pleural displacement was observed and subtle elevation of the ESP (Figure 2). 20 min after initiating MTP block, the sensorial block was evaluated using the cold and pinprick test. The sensory level decreased from T8 to T11.
The surgical procedure had a duration of 80 min, during which GA was consistently administered for 120 min. Propofol was employed at an exact dosage amounting to 766 mg, concurrently with remifentanil dosed at 1.4 mg throughout the entire operative process. As part of preemptive analgesia protocol, sufentanil administration took place 5 min before concluding the surgery using an exact dose measurement equivalent to 5 μg. The patient regained consciousness promptly, and 6 min following the successful completion of the surgical procedure, tracheal extubation was performed in the operating room, after which the patient was subsequently transferred to the PACU.
Case 1: After the patient regained consciousness, we removed the endotracheal tube. After tracheal extubation, we refrained from examining the anesthetic area due to the patient's persistent lack of complete consciousness. The numerical rating scale (NRS) score was 0 out of 10 1 h after awakening and 6 h after the operation. 12 h after surgery, the NRS score was recorded as 1/10. However, the patient reported a pain score of 2 during periods of inactivity and 3 during periods of activity on the day following surgery. Notably, no additional analgesic intervention was required during the postoperative period. On the second day after surgery, the patient resumed normal activities, the drainage tube was removed on the third day and was discharged on the fourth day.
Case 2: The NRS score was 0 out of 10 at 1 h post-awakening and 6 h post-operation. The patient was pain free and generally comfortable during the postoperative period. Subsequently, the drainage tube was removed on the third day, and the patient resumed a normal oral diet. Consequently, the patient was discharged from the hospital on the fifth day.
Renal cysts are prevalent benign renal lesions. Small cysts typically present no symptoms, while larger cysts can compress the renal parenchyma and cause low back pain or compress the collecting system and lead to hydronephrosis, necessitating surgical intervention[1]. Renal cysts can be treated through various methods, including open surgery, puncture therapy, and laparoscopic surgery. With the widespread adoption of laparoscopic technology, laparoscopic decortication has emerged as the preferred choice for treating renal cysts. Laparoscopic surgery requires a minimum of three incisions measuring 1-2 cm, and the placement of the incisions and drainage tubes elicits pain in patients during and after surgery.
MTP block is a new alternative to paravertebral block[3]. MTP block has been found to provide perioperative analgesia in breast[4,8-11], thoracoscopic[6,12-14], rib[5,15], and spinal surgery patients[16]. Due to the adjacency of the MTP block site with the beginning of nerve branches, the paravertebral spaces in each segment remain open, allowing drugs injected into this space to effectively block the corresponding level's paravertebral nerve and diffuse into adjacent thoracic paravertebral nerves and epidural space when a large volume is administered. Considering that the lower pleural boundary is located at the 12th thoracic vertebra[17], it suggests that MTP block application could also be considered for epigastric and lumbar surgery[18].
In the present study, the two operating ports, positioned 2 cm below the inferior border of the 12th rib, correspond to the T10 blocked areas. The camera port incision, positioned 2 cm above the iliac crest along the midaxillary line, corresponds to the T11 blocked areas. We observed that using 20 mL of 5% ropivacaine for segmental MTP block anesthesia at the T9 level effectively blocks sensation from the T8-T11 nerve segments and alleviates pain at the laparoscopic incision.
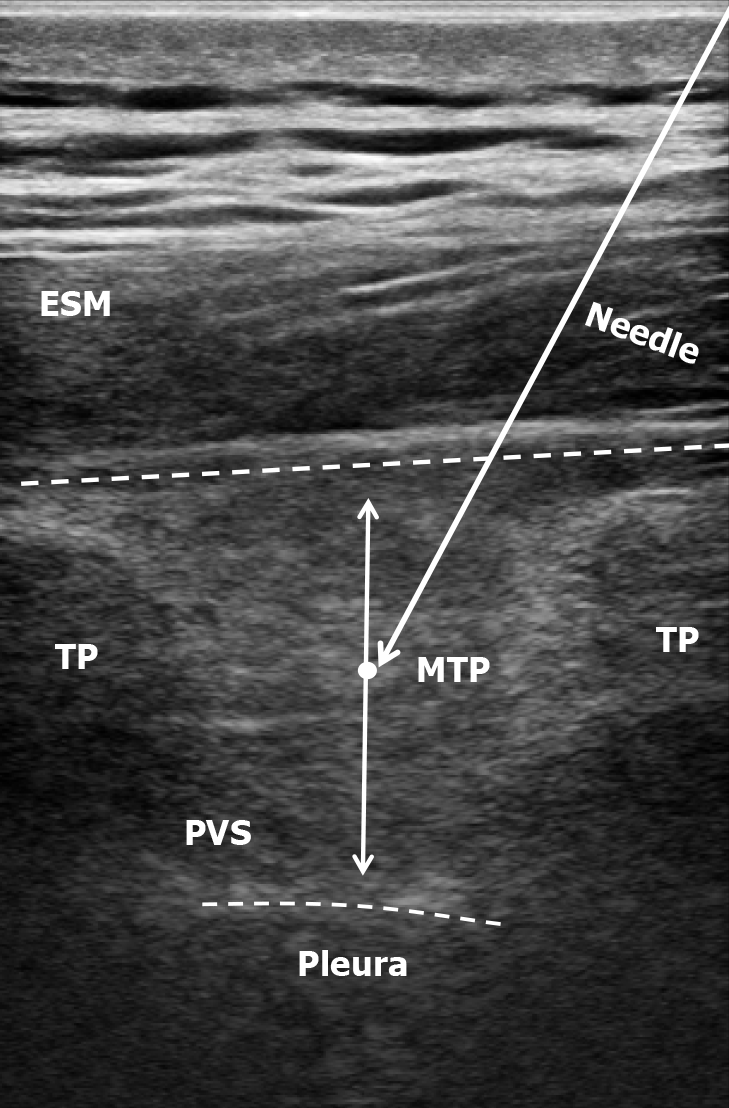
Moreover, MTP block reduces the incidence of accidental injury. For US-guided MTP block, the site selected for puncture is between the two transverse processes and the pleura[3], ensuring that it remains lateral to the SCTL to prevent inadvertent puncture into the pleural or paraspinal space (Figure 3). Conversely, for US-guided TPVB, the aim is to accurately penetrate the SCTL and inject the drug within the paravertebral space. Potentially associated complications include inadvertent vascular puncture, pleural puncture, pneumothorax, and unintentional epidural or intrathecal spread.
The use of MTP block for postoperative analgesia has shown promising results in clinical studies. Patients who have undergone laparoscopic renal cyst decortication report a decrease in pain intensity and an improvement in postoperative recovery when this technique is utilized.
To the best of our knowledge, this is the first case report documenting the effectiveness of MTP block in laparoscopic renal cyst decortication. Future larger randomized studies are required to further demonstrate and validate the efficacy of MTP block in patients undergoing laparoscopic renal cyst decortication.
In this study, we successfully implemented MTP block for postoperative analgesia in two patients undergoing laparoscopic renal cyst decortication. The MTP block was performed at the T9 level under US guidance, with 20 mL of 0.5% ropivacaine injected. Reduced sensation to cold and pinprick was observed from the T8 to T11 dermatome levels. Immediately postoperative Numeric Pain Rating Scale (NRS) scores were 0/10 at rest and on movement, with none exceeding a mean 24 h NRS > 3. In summary, MTP block was effective technique for providing postoperative analgesia for patients undergoing laparoscopic renal cyst decortication.
| 1. | Eissa A, El Sherbiny A, Martorana E, Pirola GM, Puliatti S, Scialpi M, Micali S, Rocco B, Liatsikos E, Breda A, Porpiglia F, Bianchi G; European Section of Uro-Technology (ESUT). Non-conservative management of simple renal cysts in adults: a comprehensive review of literature. Minerva Urol Nefrol. 2018;70:179-192. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 15] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 2. | Han X, Yuan G, Zhu X, Li T, Li Y, Zhang P, Zhang X, Yang B, Yin G. A comparative study of mini- versus standard laparoscopy in the treatment of renal cysts. Minim Invasive Ther Allied Technol. 2021;30:179-186. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 3. | Costache I, de Neumann L, Ramnanan CJ, Goodwin SL, Pawa A, Abdallah FW, McCartney CJL. The mid-point transverse process to pleura (MTP) block: a new end-point for thoracic paravertebral block. Anaesthesia. 2017;72:1230-1236. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 87] [Cited by in RCA: 96] [Article Influence: 12.0] [Reference Citation Analysis (0)] |
| 4. | Costache I. Mid-point transverse process to pleura block for surgical anaesthesia. Anaesth Rep. 2019;7:1-3. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 17] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 5. | Syal R, Kumar R, Kamal M, Bhatia P. Novel block and new indication: Ultrasound-guided continuous "mid-point transverse process to pleura" block in a patient with multiple rib fractures. Saudi J Anaesth. 2019;13:365-367. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 17] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 6. | Pedoto A, Kalchiem-Dekel O, Baselice S, Husta BC, Rosenblatt MA. Ultrasound-Guided Midpoint Transverse Process to Pleura Nerve Block for Medical Thoracoscopy: A Case Report. A A Pract. 2020;14:e01240. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 7. | Abdelbaser I, Abourezk AR, Badran A, Abdelfattah M. Bilateral Ultrasound-Guided Mid-Point Transverse Process to Pleura Block for Perioperative Analgesia in Pediatric Cardiac Surgery: A Randomized Controlled Study. J Cardiothorac Vasc Anesth. 2023;37:1726-1733. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 8. | Bhoi D, Narasimhan P, Nethaji R, Talawar P. Ultrasound-Guided Midpoint Transverse Process to Pleura Block in Breast Cancer Surgery: A Case Report. A A Pract. 2019;12:73-76. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 9] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 9. | Bhoi D, Ranjitha N, Talawar P, Narasimhan P. A novel out plane technique of midpoint transverse process to pleura block in breast surgery: A case report. Saudi J Anaesth. 2018;12:637-639. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 10. | Kumar R, Mohammed S, Paliwal B, Kamal M, Chhabra S, Bhatia P, Syal R. The midpoint transverse process to pleura (MTP) block for postoperative analgesia in patients undergoing modified radical mastectomy: A case series. J Anaesthesiol Clin Pharmacol. 2023;39:648-650. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |
| 11. | Kahramanlar AA, Aksoy M, Ince I, Dostbıl A, Karadenız E. The Comparison of Postoperative Analgesic Efficacy of Ultrasound-Guided Paravertebral Block and Mid-Point Transverse Process Pleura Block in Mastectomy Surgeries: A Randomized Study. J Invest Surg. 2022;35:1694-1699. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 13] [Reference Citation Analysis (0)] |
| 12. | Watton DE, Rose PGD, Abdallah FW, Thompson CP, Maziak DE, Costache I. Midpoint transverse process to pleura catheter placement for postoperative analgesia following video-assisted thoracoscopic surgery. Anaesth Rep. 2019;7:65-68. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 13. | Scimia P, Fusco P, Droghetti A, Harizaj F, Basso Ricci E. The ultrasound-guided mid-point transverse process to pleura block for postoperative analgesia in video-assisted thoracoscopic surgery. Minerva Anestesiol. 2018;84:767-768. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 14. | Chen X, Yang J, Xia M, Wu H, Wang S, Zhang W. Single-Injection Midpoint Transverse Process-to- Pleura Block Versus Thoracic Paravertebral Block for Postoperative Analgesia After Uniportal Video-Assisted Thoracoscopic Surgery: A Randomized Controlled Trial. J Cardiothorac Vasc Anesth. 2022;36:2432-2438. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 12] [Reference Citation Analysis (0)] |
| 15. | Syal R, Soni K, Kumar R, Kamal M. A novel indication of an advanced block: Mid-point transverse process to pleura block for rib cartilage harvesting in pinna reconstruction surgery-A case report. Indian J Anaesth. 2022;66:607-608. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 16. | Kilicaslan A, Kacira BK. Awake thoracic spine surgery under bilateral ultrasound guided multiple midpoint transverse process to pleura (MTP) blocks. J Clin Anesth. 2019;58:132-133. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 17. | Yalcin NG, Choong CK, Eizenberg N. Anatomy and pathophysiology of the pleura and pleural space. Thorac Surg Clin. 2013;23:1-10, v. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 29] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 18. | Eskin MB, Ceylan A, Özhan MÖ, Atik B. Ultrasound-guided erector spinae block versus mid-transverse process to pleura block for postoperative analgesia in lumbar spinal surgery. Anaesthesist. 2020;69:742-750. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 34] [Article Influence: 6.8] [Reference Citation Analysis (0)] |