Published online Jun 26, 2024. doi: 10.12998/wjcc.v12.i18.3622
Revised: April 23, 2024
Accepted: May 14, 2024
Published online: June 26, 2024
Processing time: 92 Days and 3.6 Hours
Congenital duodenal webs are rare in adults and can lead to various symptoms such as nausea, vomiting, and postprandial fullness. The treatment for this disease is mostly surgical. Endoscopic treatment techniques have been developed and attempted for this disease. Endoscopic radial incision and cutting (RIC) techniques are reportedly very effective in benign anastomotic stricture. This case report highlights the effectiveness and safety of endoscopic RIC as a minimally invasive treatment for adult congenital duodenal webs.
A 23-year-old female patient with indigestion was referred to a tertiary hospital. The patient complained of postprandial fullness in the epigastric region. Previous physical examinations or blood tests indicated no abnormalities. Computed tomography revealed an eccentric broad-based delayed-enhancing mass-like lesion in the second portion of the duodenum. Endoscopy showed an enlarged gastric cavity and a significantly dilated duodenal bulb; a very small hole was observed in the distal part of the second portion, and scope passage was not possible. Gastrografin upper gastrointestinal series was performed, revealing an intraduodenal barium contrast-filled sac with a curvilinear narrow radiolucent rim, a typical "windsock" sign. Endoscopic RIC was performed on the duodenal web. The patient recovered uneventfully. Follow-up endoscopy showed a patent duodenal lumen without any residual stenosis. The patient reported complete resolution of symptoms at the 18-month follow-up.
Endoscopic RIC may be an effective treatment for congenital duodenal webs in adults.
Core Tip: The treatment of duodenal webs has evolved with medical advancements, particularly in endoscopy, shifting from traditional surgical management to minimally invasive endoscopic approaches. Recent advances in endoscopic instruments and techniques have rendered endoscopic treatment a viable alternative. Generally, endoscopic balloon dilatation requires multiple sessions rather than a single treatment. Endoscopic membranectomy or incisional therapy may ultimately necessitate surgical intervention for restenosis owing to scarring. By contrast, radial incision and cutting is a safe, rapid, and effective treatment method that allows complete circumferential excision of the web. Unlike surgery, it does not require a prolonged hospital stay and presents a very low risk of surgical complications, making it an effective alternative treatment.
- Citation: Shin HD. Endoscopic radial incision and cutting method for adult congenital duodenal webs: A case report. World J Clin Cases 2024; 12(18): 3622-3628
- URL: https://www.wjgnet.com/2307-8960/full/v12/i18/3622.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i18.3622
Congenital duodenal web is a type of duodenal atresia in which the duodenal membrane partially or completely obstructs the duodenal lumen, leading to various gastrointestinal symptoms. The incidence of congenital duodenal anomalies is approximately 1 in 20000 to 40000 births, with partial obstructive lesions, including duodenal webs, accounting for only 2% of these defects[1]. Diagnosis is challenging, and curative treatment is commonly delayed. Congenital duodenal web is commonly diagnosed during the neonatal period because patients with duodenal webs develop obstructive symptoms shortly after birth. In some cases, it is diagnosed in infancy or early childhood. Although commonly diagnosed in infancy, rare cases have been reported in adults. The delayed presentation of the duodenal web in adults is difficult to explain, likely because pretreatment diagnoses are rare owing to nonspecific symptoms and a general lack of awareness of this uncommon clinical entity[2]. The degree of obstruction, age at presentation, and imaging findings depend on the web aperture[3]. Adult cases can present with symptoms ranging from mild to severe, depending on the size and location of the web. Traditionally, the duodenal web is completely removed surgically. Recently, with the development of endoscopic accessories and techniques, endoscopic treatment has been performed effectively in some cases. The duodenal web is a membrane-like structure composed of the mucosa and submucosa, lacking a muscularis layer[4]. These anatomical features provide the rationale for using endoscopic radial incision and cutting (RIC) to treat duodenal webs. This endoscopic RIC method is a minimally invasive approach, potentially avoiding the need for extensive surgical intervention.
A 23-year-old female patient presented at our hospital with indigestion. The patient's symptoms were mainly bloating and fullness after eating, and the patient stated that she easily felt bloated.
The patient had visited the hospital frequently since childhood because of indigestion. Every time she visited, she was told that it was a functional gastrointestinal disorder; however, she was not diagnosed with any specific disease. Postprandial bloating and fullness persisted into adulthood. Recently, she reported a 4 kg weight loss because of decreased food consumption, which was accompanied with epigastric pain and heartburn.
No unusual surgical history or specific diseases were noted.
No history of malignancy or underlying specific disease in the family was reported.
The patient’s vital signs were as follows: blood pressure, 124/76 mmHg; respiratory rate, 16 breaths/min; heart rate, 76 beats/min; and body temperature, 36.7 °C. No abdominal or rebound tenderness, epigastric distension, gastric splash, organomegaly, or palpable abdominal masses were observed. Normal bowel sounds were identified. The patient was 158 cm tall, weighed 41 kg, and had a body mass index of 16.42 kg/m2.
The results of routine laboratory tests, including routine blood tests, blood biochemistry, routine urine examinations, fecal occult blood, and tumor markers, were all within normal limits.
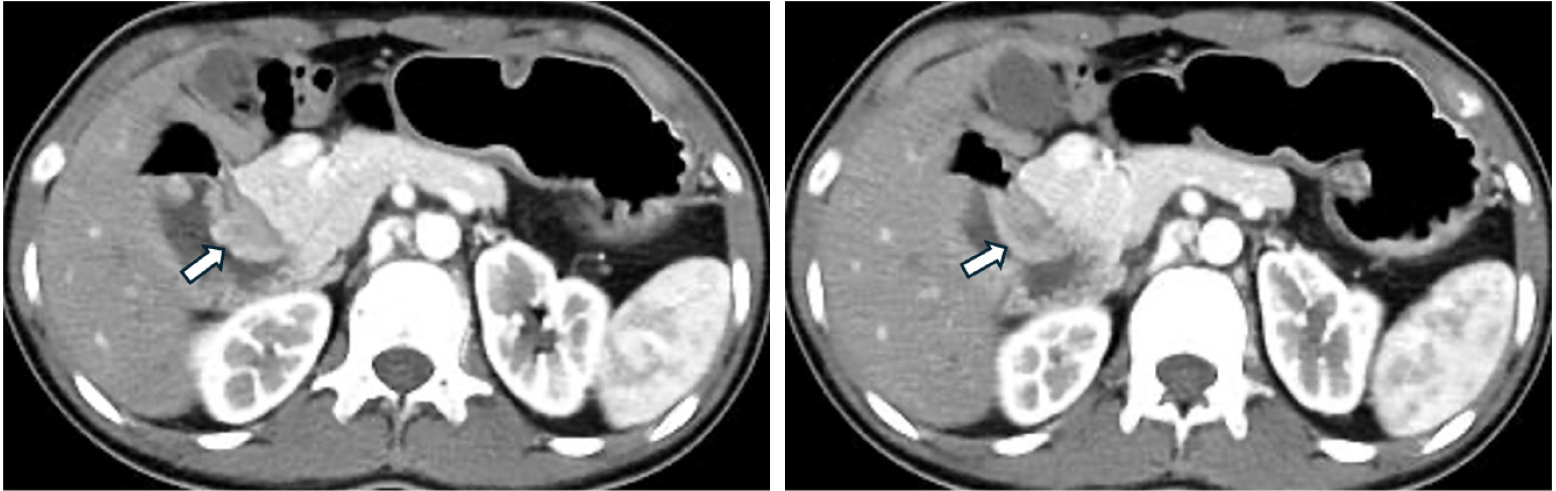
Abdominopelvic computed tomography revealed an eccentric broad-based delayed-enhancing mass-like lesion in the medial wall of the second duodenum (1.8 cm) (Figure 1). These findings suggested a duodenal subepithelial tumor.
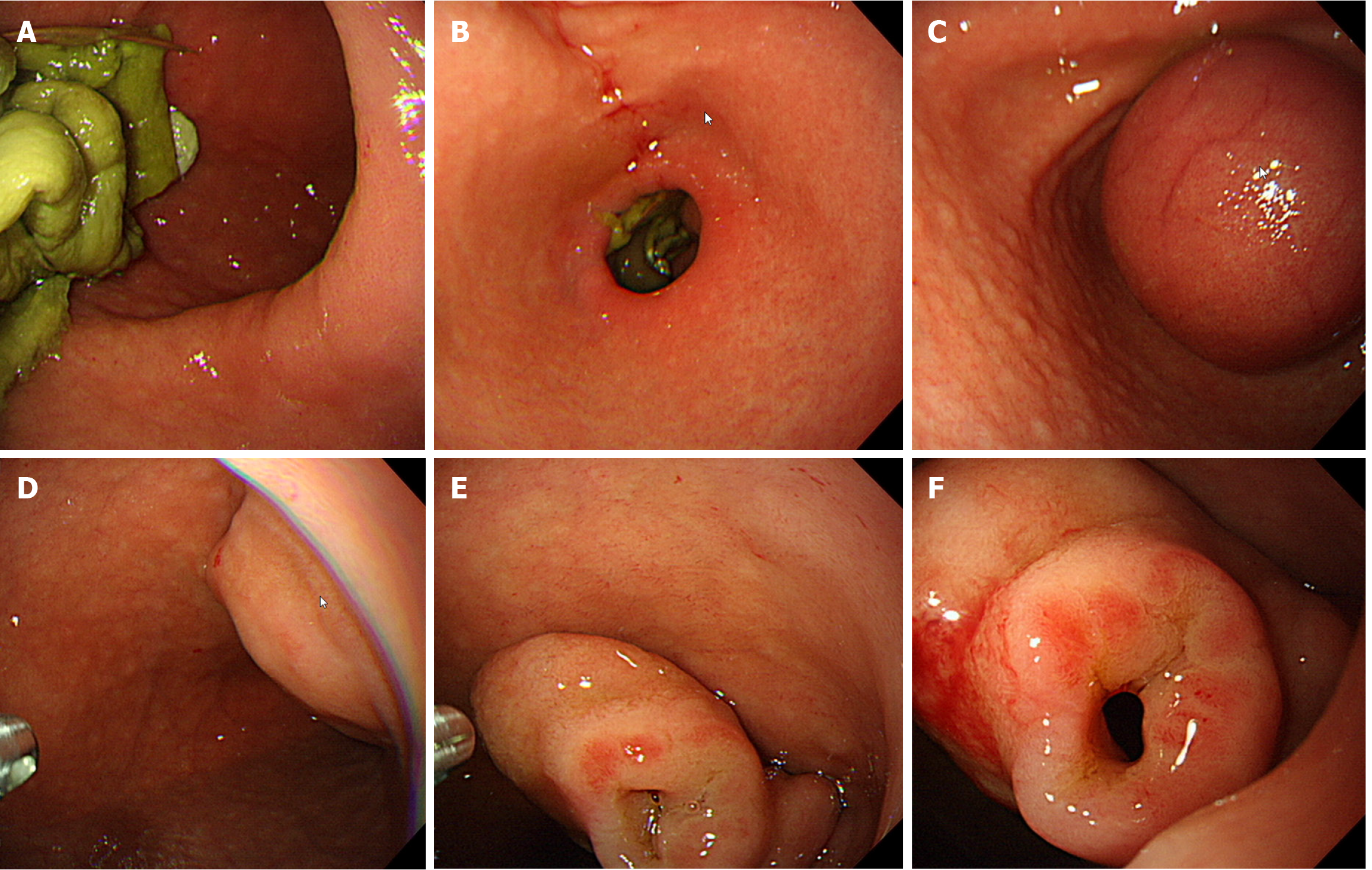
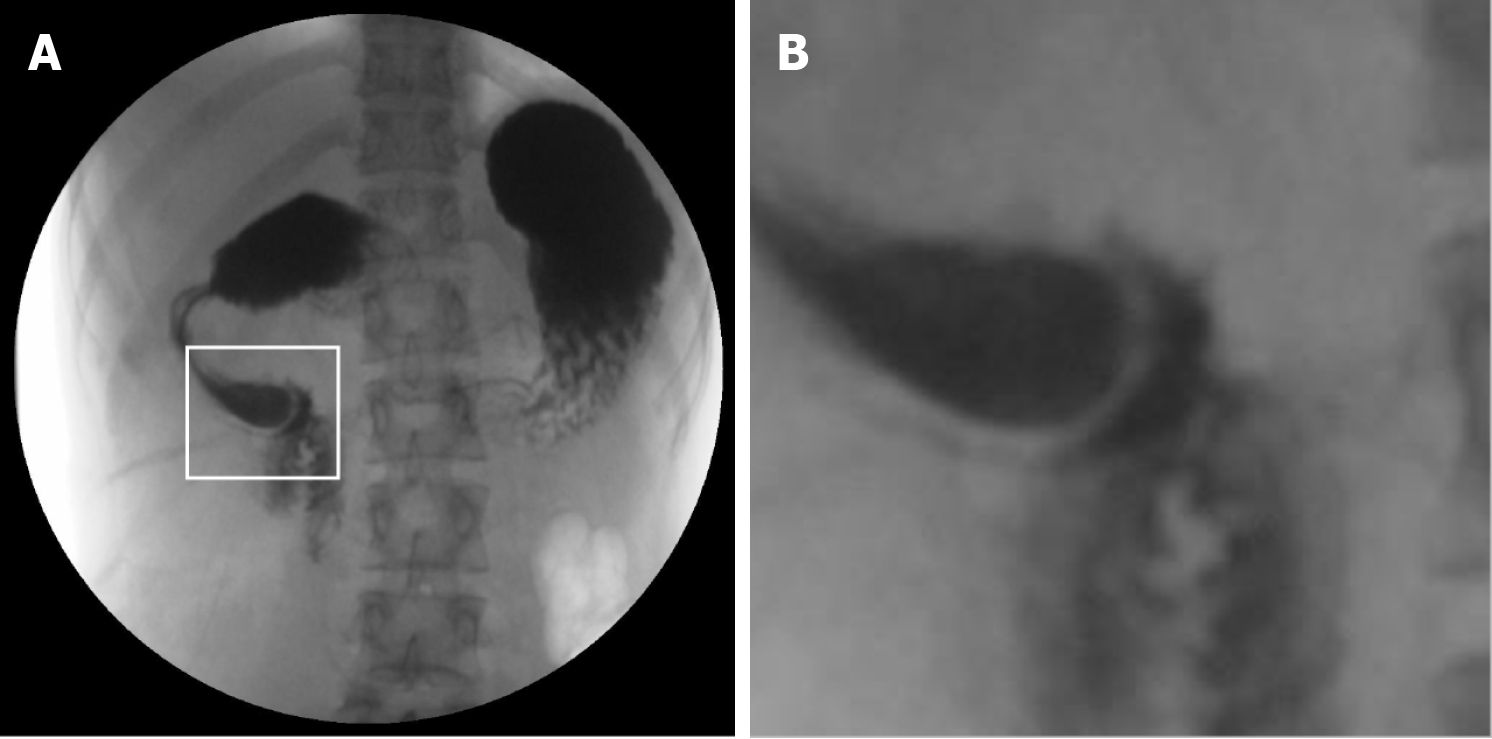
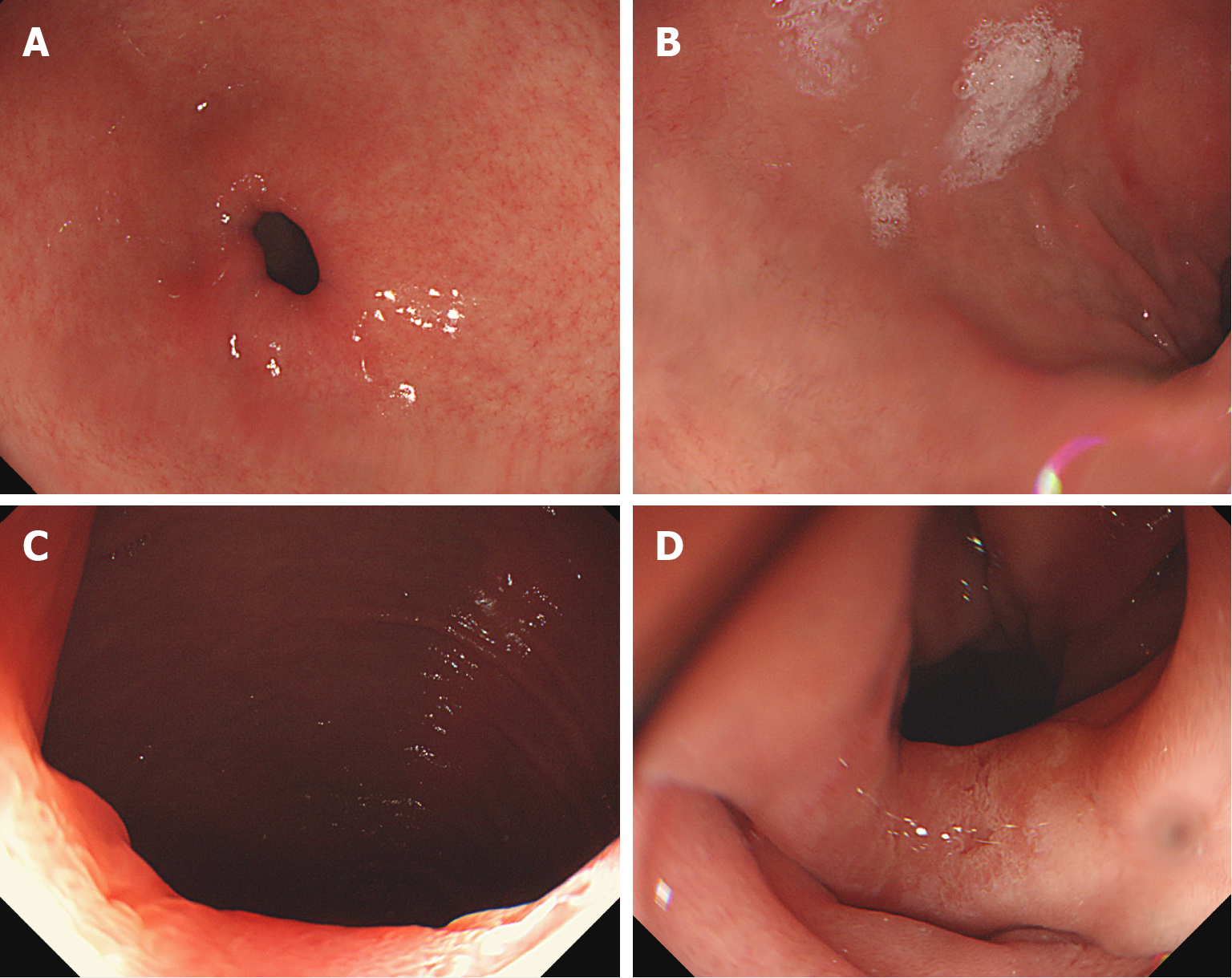
The initial investigations did not yield a definitive diagnosis. Considering the chronic nature and recent exacerbation of her symptoms, a more detailed diagnostic workup was performed. Gastroduodenoscopy revealed an overextended gastric cavity and food residue filling the duodenal bulb. Upon the removal of food from the gastric cavity, the bulb was significantly distended. Inserting the scope further revealed a small hole at the end of the second portion of the duodenum, through which the scope could not pass through. The aperture size was approximately < 5 mm because a nasal scope with a diameter of 5.4 mm could not pass through. The lesion invaginated proximally and appeared mass-like (Figure 2). Subsequently, an upper gastrointestinal (UGI) series was performed using gastrografin, which showed an intraduodenal barium contrast-filled sac with a curvilinear narrow radiolucent rim, displaying the typical "windsock" sign (Figure 3). Endoscopic and UGI studies revealed a congenital duodenal web partially obstructing the duodenal lumen, which was identified as the cause of the patient’s symptoms.
The patient was diagnosed with a pre-ampullary type congenital duodenal web at the distal end of the second portion of the duodenum.
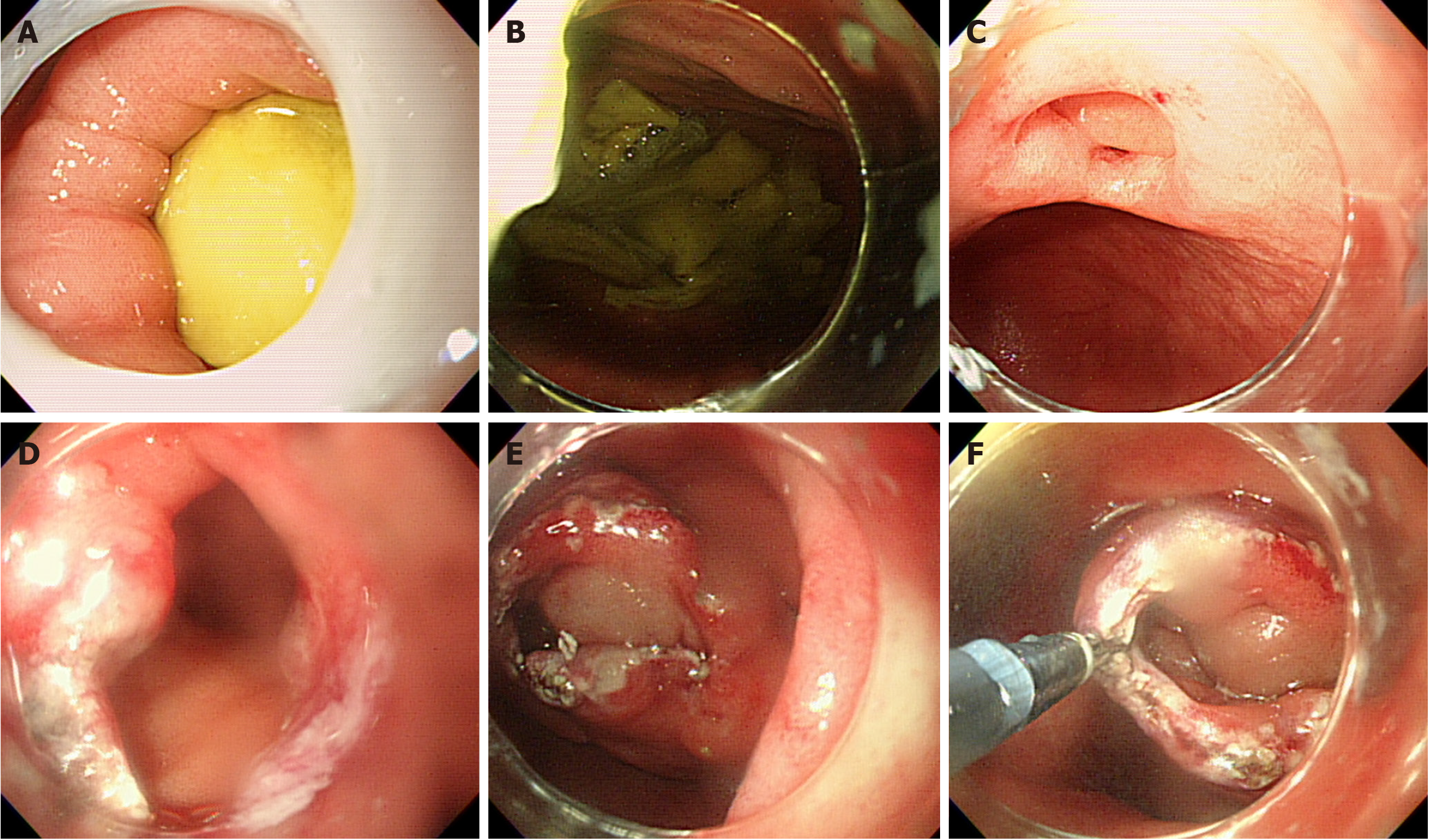
The patient discussed the treatment plan with an experienced pediatric surgeon for this type of surgery. Initially, surgery was considered; however, because of the high risk of laparotomy and various complications, the patient and her mother preferred a less invasive treatment. Considering the patient’s desire for minimally invasive treatment and the potential complications associated with surgical intervention, we adopted the endoscopic RIC method. The patient was placed under general anesthesia. The RIC technique involved using an insulation-tipped electrosurgical knife (IT2-knife, KD-611L; Olympus, Tokyo, Japan) to cut the duodenal web. The Erbe VIO 300D electrosurgical system (Erbe Elektromedizin GmbH, Tubingen, Germany) was set to Endo Cut Q mode using Effect setting 2 (30 W) to create incisions and remove the web. Unfortunately, despite the patient fasting for a long time, similar to the first diagnostic endoscopy, a large amount of fibrous food residue was discovered in the gastric cavity and duodenal bulb. All the contents were removed from the gastric cavity before the procedure. The RIC procedure was started by carefully making a small incision under direct visualization, with a transparent cap applied to the tip of the endoscope to enhance the view of the distal duodenum. The endoscope was advanced further to ascertain the location of the ampulla of Vater (AoV). In this patient, the duodenal web was pre-ampullary. Subsequently, the incision was expanded until it approached the duodenal wall. Similar to endoscopic submucosal dissection (ESD), under direct endoscopic visualization, an incision was carefully made circumferentially along the duodenal wall and into the space between the web and wall. The incision was made opposite the AoV to avoid damaging it. An incision was made halfway through the lumen, and complete resection was not attempted, as in the first procedure (Figure 4). The procedure was completed without complications, and the patient was monitored for any immediate postoperative complications. The procedure lasted approximately 20 min. Subsequently, lumen width was sufficiently secured.
The patient’s recovery was remarkably smooth, with a significant improvement in symptoms immediately after the procedure. Diet was resumed on the second post-procedure day, and the patient reported no postprandial discomfort, a marked change from that before the procedure. One month after discharge, the patient reported having gained approximately 5 kg and expressed great enjoyment in eating, noting significant happiness. A follow-up endoscopy conducted 12 months later confirmed the absence of residual stenosis (Figure 5). The patient remained symptom-free for 18 months since the procedure. This outcome not only illustrates the effectiveness of the endoscopic RIC method for treating congenital duodenal webs in adults, but also highlights its benefits as a minimally invasive alternative to traditional surgical approaches.
Because the incidence of duodenal webs is extremely low and most cases are diagnosed during the neonatal period, its occurrence and detection in adults are very rare. The delayed presentation of duodenal webs in adults is difficult to explain. Fewer than 100 cases have been reported in the literature in the last 100 years[1]. The most important factor in the manifestation of symptoms is the size of the web aperture as this determines the degree of obstruction, age at presentation, and radiologic findings[3]. Gradual fibrosis of the web aperture is presumed to occur owing to various stimuli progresses, followed by the progressive loss of compensatory peristaltic action of the stomach and duodenal bulb. This results in a marked expansion of the stomach and duodenal bulb, eventually leading to symptoms[1]. When symptoms of intestinal obstruction occur acutely, they may be attributable to an acute inflammatory event caused by food debris, mucosal edema, and ulceration in the web region that precipitates acute intestinal obstruction[2].
The traditional clinical characteristic of gastric outlet obstruction syndrome is gradual development. Typically, a history of recurrent postprandial discomfort and vomiting is reported. A history of indigestion since childhood, especially in those who struggle with early satiety and postprandial fullness, can serve as a symptomatic diagnostic indication for the presence of a duodenal web. In most cases, physical examination yields no specific findings; however, in some cases, gastric splashes may be heard when accompanied with an acute obstruction.
If the possibility of this rare condition is not considered, an endoscopist may mistake the markedly dilated duodenal bulb for a dilated antrum and web of the pylorus, leading to a misdiagnosis of pyloric obstruction. Endoscopy is useful in ruling out peptic ulcer disease and making a diagnosis. However, endoscopy as the initial examination correctly diagnoses 50% of cases[5]. As in this case, a large amount of food residue remaining in the gastric cavity and duodenal bulb despite long periods of fasting, along with significant dilation of the gastric cavity and duodenal bulb, can serve as diagnostic clues for obstruction by a duodenal web. The diagnosis is most often confirmed by a UGI series, which shows a dilated stomach and bulb, indicative of megaduodenum. The UGI study typically demonstrates a significantly dilated duodenal bulb filled with barium and a thin radiolucent rim-leakage of barium through the small hole in the barium-filled area is considered a typical saccular “windsock” sign[1,2].
Because relatively few cases of duodenal webs have been reported in adults, surgical treatment has varied, and various operations have been suggested. These include duodenoduodenostomy, duodenostomy, duodenostomy with incision or excision of the web, duodenojejunostomy, and duodenoplasty. Most patients are treated by longitudinal duodenotomy with excision followed by Heineke–Mikulicz strictureplasty[1]. Disadvantages of surgery include greater invasiveness, longer hospital stays, and commonly associated complications.
Recently, with the development of endoscopic accessories and techniques, endoscopic treatment has been effectively performed in some cases[6-10]. However, these treatments have limitations. In general, endoscopic balloon dilatation is an effective and relatively safe procedure; however, its main disadvantage is that it requires several repeated sessions rather than being completed in one session[10]. Endoscopic incision or Nd:YAG laser ablation may lead to delayed scar formation, resulting in restenosis, potentially necessitating subsequent surgery[6,7].
When considering endoscopic treatment of the duodenal web, the anatomical features of the web need to be examined. The duodenal web is a membrane-like structure composed of mucosa and submucosa that lack a muscularis layer[4]. This absence allows selective resection of the web without damaging the thin underlying duodenal muscle layer using advanced techniques such as ESD. The effectiveness of the endoscopic RIC method has already been demonstrated in the treatment of benign anastomotic strictures in the gastrointestinal tract[11-14]. Because the duodenal web is a benign stricture, the RIC method is applicable. However, care must be taken with most duodenal webs because of their juxta-ampullary location, and to minimize damage to the biliary and pancreatic ducts during the procedure. The RIC method allows for complete circumferential excision of the duodenal web, similar to other surgical methods, and the procedure time is significantly shorter than that of traditional surgery. In this case, securing the width of the lumen was expected, even with an incision made up to half the lumen in the initial procedure. An incision must be made under direct vision through a transparent cap applied to the tip of the endoscope to avoid damaging the muscle layer of the thin duodenal wall.
The management of congenital duodenal webs in adults poses a significant clinical challenge owing to the rarity of the condition and variability of symptoms. Traditional treatments often involve surgical intervention, which is associated with a higher risk of morbidity and longer recovery time. As demonstrated in our case, the endoscopic RIC method offers a viable alternative with several advantages, including reduced procedural risk, shorter hospital stay, and faster recovery.
Endoscopic treatments for duodenal webs have evolved over time, using various techniques described in the literature. However, the endoscopic RIC method stands out for its simplicity and effectiveness. By making radial incisions and then cutting through the web, we ensured complete resolution of the obstruction while minimizing the risk of complications such as perforation or bleeding.
Our case underscores the importance of considering congenital duodenal webs in the differential diagnosis of adults who present with long-term nonspecific gastrointestinal symptoms. Furthermore, it highlights the role of endoscopic RIC as a first-line treatment option, providing a less invasive approach than traditional surgery, with comparable outcomes.
The successful treatment of an adult congenital duodenal web using the endoscopic RIC method in this study supports the safety and effectiveness of this method for treating such rare condition. Moreover, this emphasizes the need for awareness among clinicians regarding the potential presence of congenital duodenal webs in adults and availability of minimally invasive endoscopic treatments.
| 1. | Ladd AP, Madura JA. Congenital duodenal anomalies in the adult. Arch Surg. 2001;136:576-584. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 46] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 2. | Norman CH Jr, Pacis AB. Congenital duodenal web in an adult. J Natl Med Assoc. 1978;70:797-798. [PubMed] |
| 3. | Alghannam R, Yousef YA. Delayed presentation of a duodenal web. J Pediatr Surg Case Rep. 2015;3:530-533. [RCA] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 4. | Morris G, Kennedy A Jr, Cochran W. Small Bowel Congenital Anomalies: a Review and Update. Curr Gastroenterol Rep. 2016;18:16. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 53] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 5. | Marwah S, Gurawalia JP, Sagu R, Marwah N. Congenital duodenal diaphragm in an adult masquerading as superior mesenteric artery syndrome. Clin J Gastroenterol. 2013;6:217-220. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 6. | Gertsch P, Mosimann R. Endoscopic laser treatment of a congenital duodenal diaphragm in an adult. Gastrointest Endosc. 1984;30:253-254. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 17] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 7. | Jex RK, Hughes RW Jr. Endoscopic management of duodenal diaphragm in the adult. Gastrointest Endosc. 1986;32:416-419. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 14] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 8. | Torroni F, De Angelis P, Caldaro T, di Abriola GF, Ponticelli A, Bergami G, Dall'Oglio L. Endoscopic membranectomy of duodenal diaphragm: pediatric experience. Gastrointest Endosc. 2006;63:530-531. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 17] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 9. | Lee SS, Hwang ST, Jang NG, Tchah H, Choi DY, Kim HY, Ryoo E. A case of congenital duodenal web causing duodenal stenosis in a down syndrome child: endoscopic resection with an insulated-tip knife. Gut Liver. 2011;5:105-109. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 23] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 10. | Zimmer V, Bergheim C. Late-Presenting Duodenal Web. Clin Gastroenterol Hepatol. 2020;18:A35. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 11. | Lee TH, Lee SH, Park JY, Lee CK, Chung IK, Kim HS, Park SH, Kim SJ, Hong SJ, Lee MS. Primary incisional therapy with a modified method for patients with benign anastomotic esophageal stricture. Gastrointest Endosc. 2009;69:1029-1033. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 51] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 12. | Muto M, Ezoe Y, Yano T, Aoyama I, Yoda Y, Minashi K, Morita S, Horimatsu T, Miyamoto S, Ohtsu A, Chiba T. Usefulness of endoscopic radial incision and cutting method for refractory esophagogastric anastomotic stricture (with video). Gastrointest Endosc. 2012;75:965-972. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 96] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 13. | Kawaguti FS, Martins BC, Nahas CS, Marques CF, Ribeiro U, Nahas SC, Maluf-Filho F. Endoscopic radial incision and cutting procedure for a colorectal anastomotic stricture. Gastrointest Endosc. 2015;82:408-409. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 15] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 14. | Lee TG, Yoon SM, Lee SJ. Endoscopic radial incision and cutting technique for treatment-naive stricture of colorectal anastomosis: Two case reports. World J Gastrointest Surg. 2020;12:460-467. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |