Published online Jun 26, 2024. doi: 10.12998/wjcc.v12.i18.3575
Revised: April 21, 2024
Accepted: April 24, 2024
Published online: June 26, 2024
Processing time: 117 Days and 21 Hours
Intrabony defects beneath non-keratinized mucosa are frequently observed at the distal site of terminal molars. Consequently, the application of regenerative treatment using the modified wedge-flap technique is considered impractical for these specific dental conditions.
This article proposes a modified surgical procedure aimed at exposing the distal intrabony defect by making a vertical incision in the keratinized buccal gingiva. The primary objective is to maintain gingival flap stability, thereby facilitating periodontal regeneration. The described technique was successfully employed in a case involving the left mandibular second molar, which presented with an intrabony defect without keratinized gingiva at the distal site. In this case, an incision was made on the disto-buccal gingival tissue, creating a tunnel-like separation of the distal non-keratinized soft tissue to expose the intrabony defect. Subsequently, bone grafting and guided tissue regeneration surgeries were performed, resulting in satisfactory bone fill at 9 mo postoperatively.
This technique offers a regenerative opportunity for the intrabony defects beneath non-keratinized mucosa and is recommended for further research.
Core Tip: Intrabony defects beneath non-keratinized mucosa frequently occur at the distal of terminal molars, thereby rendering standard regenerative therapy considered impractical. Consequently, we devised a surgical strategy tailored to this specific scenario. By making a vertical incision in the keratinized buccal gingiva, we were able to separate distal non-keratinized soft tissue in a tunnel-like manner, exposing the defect. Regenerative therapy was effectively administered, offering a promising avenue for teeth with non-keratinized mucosa above intrabony defects.
- Citation: Liu JR, Huang Y, Ouyang XY, Liu WY, Xie Y. Modified approach of regenerative treatment for distal intrabony defect beneath non-keratinized mucosa at terminal molar: A case report. World J Clin Cases 2024; 12(18): 3575-3581
- URL: https://www.wjgnet.com/2307-8960/full/v12/i18/3575.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i18.3575
The regeneration of periodontal supporting tissue is an vital objective in periodontal therapy. For addressing the remaining intrabony defect after non-surgical treatment, regenerative treatment is often advocated[1,2]. While the modified wedge flap technique remains a common choice for unveiling intrabony defects in the distal region of the terminal molars during regenerative surgery[3], its efficacy relies on the presence of sufficient keratinized gingiva in the distal area. Unfortunately, a substantial number of Chinese patients exhibit an absence of keratinized tissue in the distal region of the second mandibular molar, which poses a significant challenge in performing regenerative surgery.
This study aims to introduce a novel surgical approach for regenerative therapy targeting the distal intrabony defect of the terminal molar, specifically addressing the non-keratinized mucosa above the defect. This approach involves making an incision in the buccal gingival tissue and creating a tunnel-like separation of the distal non-keratinized soft tissue.
Gingival bleeding when brushing teeth for at last 5 years.
In the last 5 years, a 56-year-old woman frequently experienced bleeding while brushing her teeth, particularly around the left mandibular terminal tooth. The gum surrounding the affected tooth occasionally presented with a reddish hue, although the tooth itself was devoid of any pain. The patient had a horizontally impacted wisdom tooth in the left mandibular region extracted 2 years earlier. Her oral hygiene routine consisted of employing the vertical brushing technique, spending 2 min on each session, twice daily. She was a nonsmoker and occasionally used tooth floss for interdental cleaning.
The patient had controlled type 2 diabetes mellitus with a hemoglobin A1c level of 7.0%. Additionally, she had undergone heart stent placement 2 years ago and was currently on low-dose anticoagulant medication.
Her family history was unremarkable.
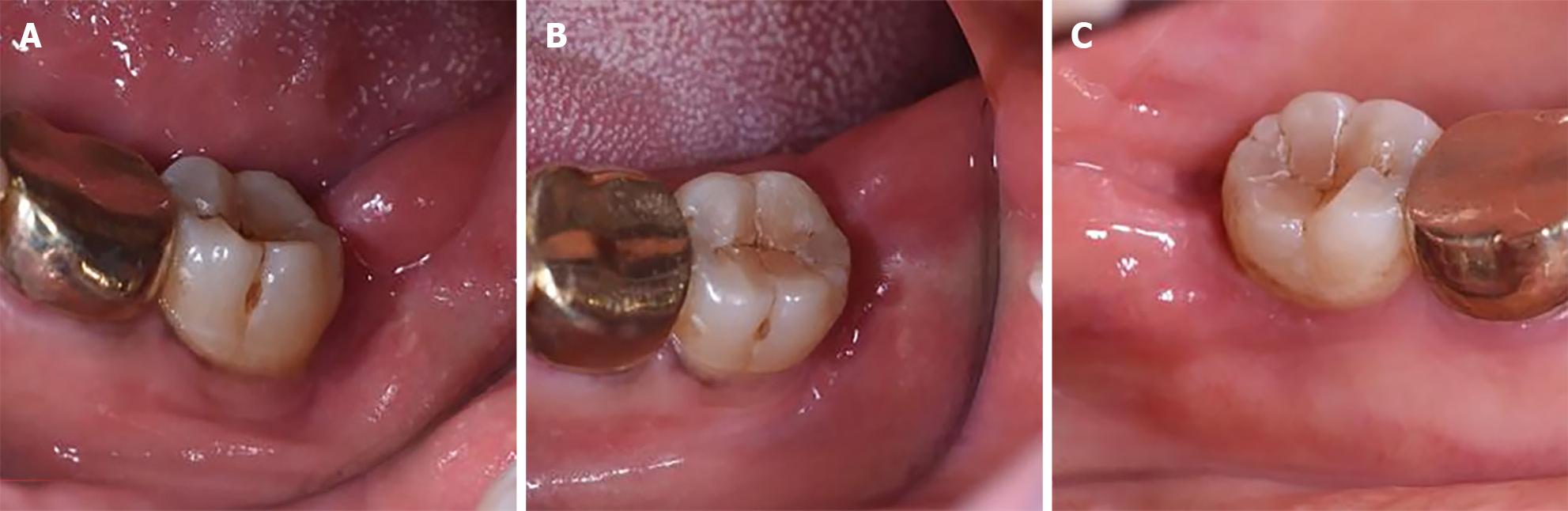
A persistent probing pocket depth (PPD) of 8 mm and clinical attachment loss (CAL) of 7 mm were noted at the distal end of tooth 37, which also lacked keratinized gingiva at the distal site (Figure 1). In addition, the PPD at the distal site of the tooth 36 was 5mm.
The patient's preoperative coagulation tests showed a prothrombinogen activity of 157.6% (normal range 70%-130%), and the rest of the blood profile revealed no abnormalities.
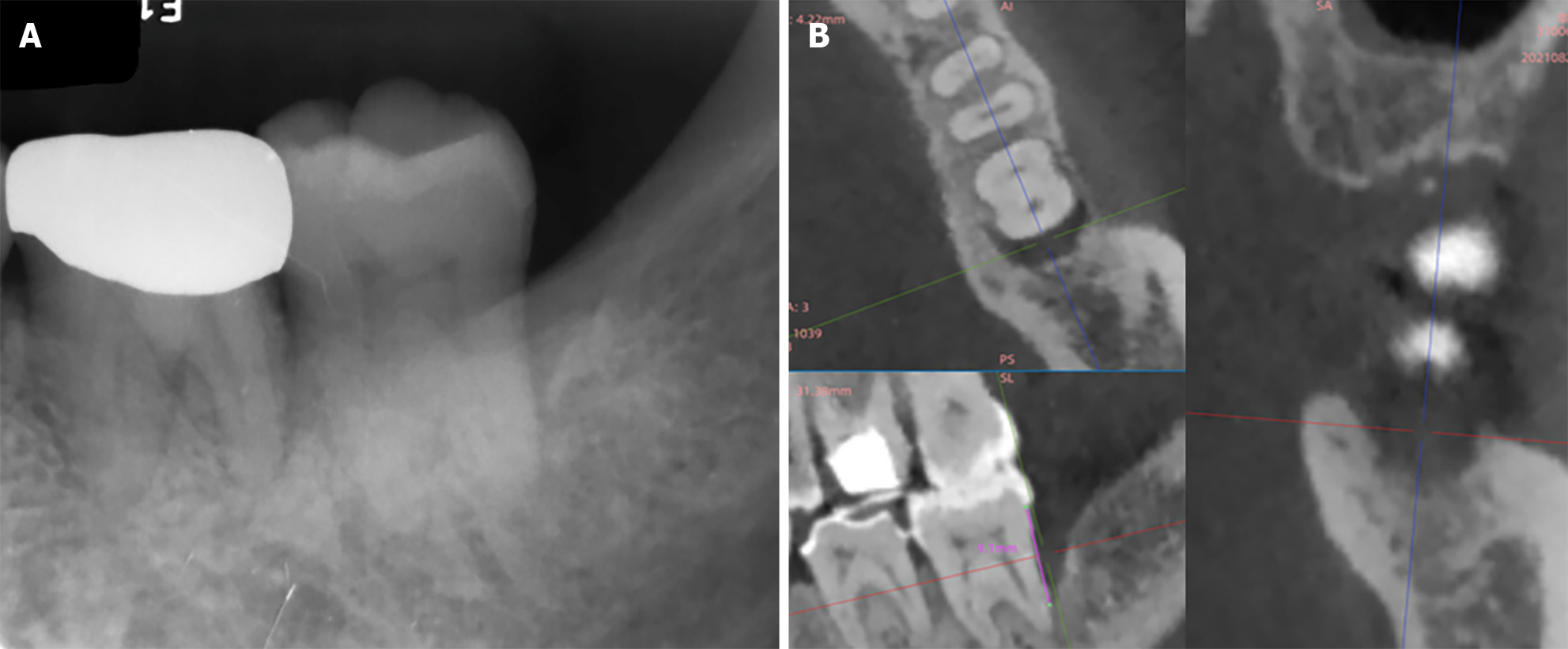
The periapical radiographic images of tooth 37 showed an angular bone defect on the distal aspect of the second molar (Figure 2A). A 3-wall intrabony defect was identified at this site based on a cone-beam computed tomography image (Figure 2B).
Based on the clinical and imaging examination, the patient was diagnosed with periodontitis (stage III, grade C).
Initial periodontal therapy was administered to reduce periodontal tissue inflammation, with reevaluation occurring after three months. Following the non-surgical treatment, there was a marked improvement in her periodontal health. However, due to tooth 37’s probing depth of 8 mm, periodontal regenerative surgery was scheduled.
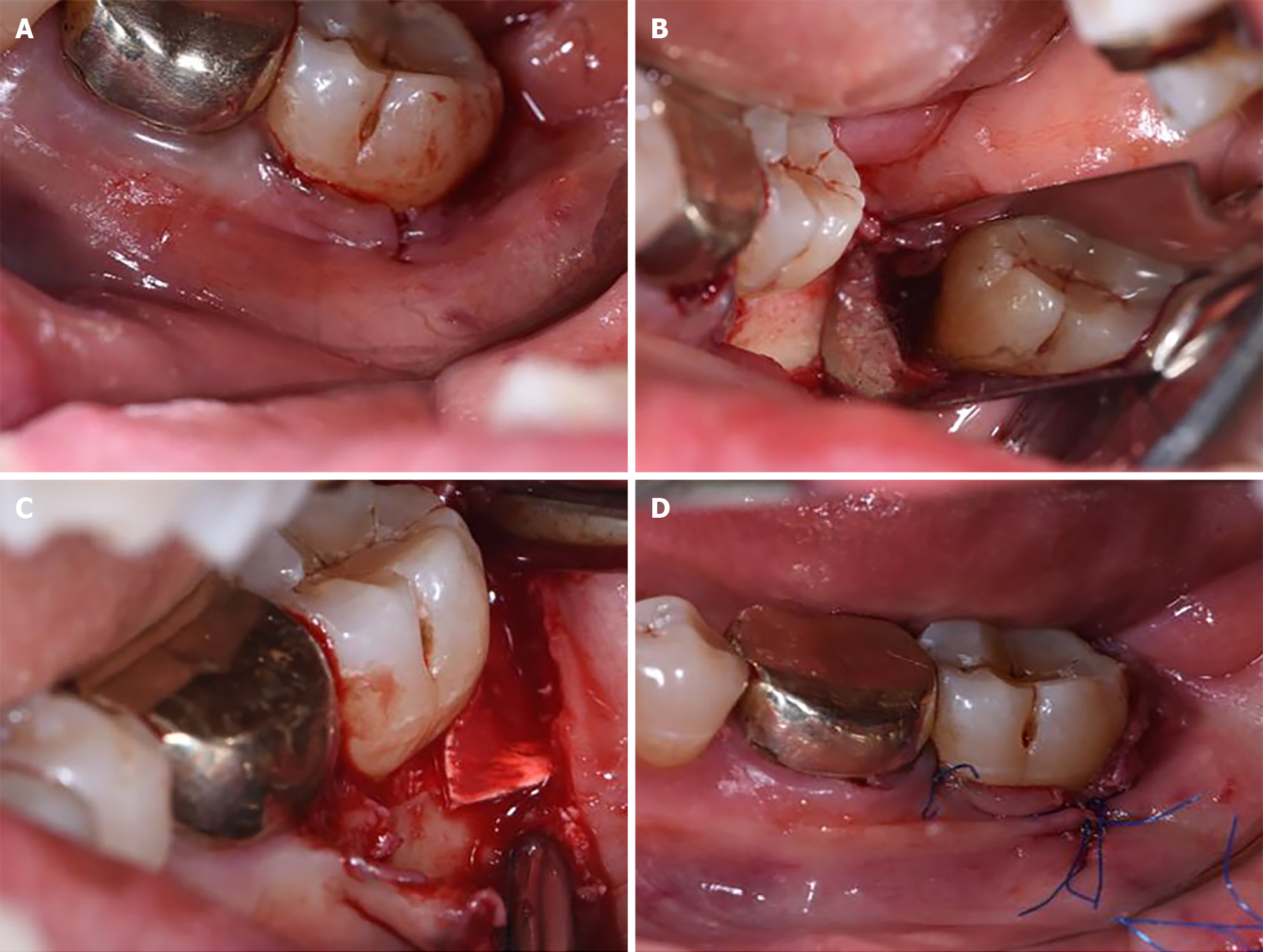
After local anesthesia, using 4% articaine hydrochloride with 1:100000 adrenaline, a sulcular incision was made from the distal site of tooth 37 to the distal site of tooth 36 using a No. 15C blade. Owing to the absence of a keratinized gingiva at the distal end of this terminal tooth, no further leaner incisions were made in the distal tissue. Instead, a vertical incision was made over the mucogingival junction on the distobuccal gingiva of tooth 37 where the width of keratinized tissue was 3 mm (Figure 3A). The full-thickness flap was flipped along the incision, and the sharp separation of the distal soft tissue from the bone crest was achieved using a No. 15C blade. This approach ensured that the soft tissue could be accurately detached from the pocket lining within the bone defect. Then the entire distal soft tissue was then gently tunneled and separated from the bone crest using an elevator. It was elevated up to the lingual bone crest to expose the intrabony defect. Thorough debridement with ultrasound and manual curettage revealed a 3-wall intrabony defect in the distal region adjacent to the terminal molar. The distance from cemeto-enamel junction to the base of the intrabony defect was 8 mm, and the depth of this defect was 6 mm with a maximum mesiodistal width of 3 mm and a maximum buccolingual width of 8 mm (Figure 3B). This intrabony defect was filled with deproteinized bovine bone mineral (Geistlich Bio-Oss, Geistlich Pharma, Wolhusen, Switzerland) and covered with a collagen membrane (Geistlich Bio-Guide) (Figure 3C). The mesial papillae were closed using interrupted sutures, and an anchored suture was placed on the vertical incision (Figure 3D).
Ibuprofen was administrated once daily for the first 3 d following the surgery, and systemic amoxicillin medicine (500 mg, tid) was administered continuously for 1 wk. Any mechanical plaque control measures in the surgical area was prohibited for 2 wk after surgery. Instead, a 0.12% compound chlorhexidine rinse was used twice daily to chemically control plaques. The sutures were removed 2 wk after surgery, and periodontal maintenance was performed every 3 months.
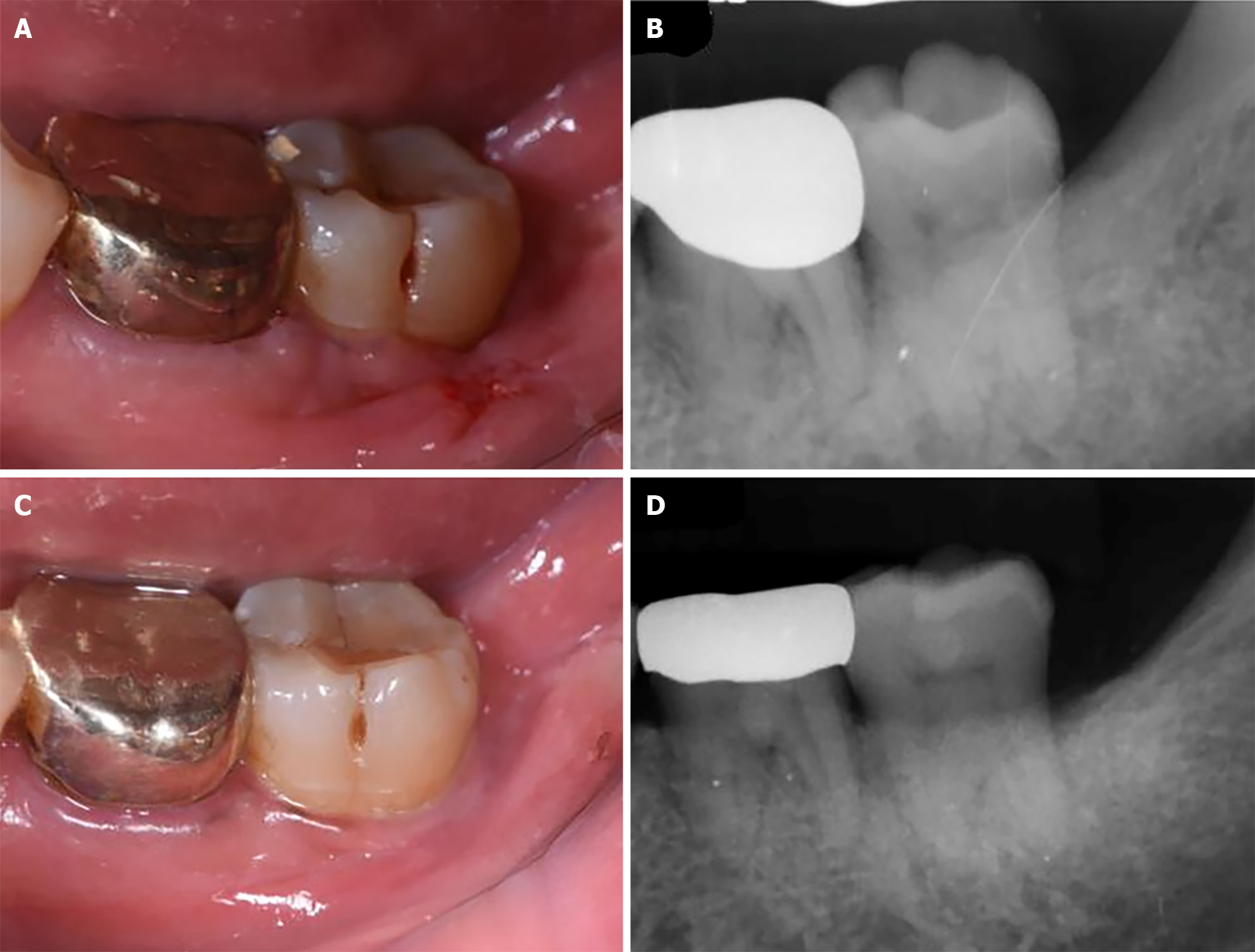
During the first 2 wk of the early healing phase, primary wound healing of the vertical releasing incision and good integrity of the distal non-keratinized soft tissue were observed (Figure 4A). The parallel periapical film showed 100% bone fill in the distal intrabony defect (Figure 4B). Throughout this period, the patient had reported awareness of slight edema at the surgical site, however the pain was minimal.
At 9 months postoperatively, no gingival recession appeared (Figure 4C), and the clinical examination revealed a PPD reduction at the distal site of the mandibular left second molar to 4 mm, with a gain of CAL up to 5 mm. At this point, the radiographic bone gain remained satisfactory at this site according to the parallel film (Figure 4D). No adverse events were observed during the treatment period.
In this case, the distal intrabony defect was exposed using a novel surgical approach in which a buccal vertical incision was made, and the distal soft tissue was elevated in a tunnel-like manner. This modified technique could not only ensures the stability of the gingival flap, but also effectively expose the underlying distal intrabony defect that facilitate thorough debridement and regenerative surgery. In other word, this novel procedure offers an opportunity for the regenerative treatment of terminal molars previously deemed ineligible for such interventions, significantly improving the prognosis of the affected tooth.
The CAL gain in the distal intrabony defect of tooth 37 reached 5 mm with satisfactory bone fill observed at 9 months postoperatively, indicating a successful regeneration of the site. The clinical outcomes of periodontal regenerative therapy are significantly influenced by various factors, including defect morphology, choice of regenerative biomaterials, incision design, and surgical flap management[4-8]. In addition, cumulative evidence has demonstrated the critical role of blood clot stability during the early wound healing phase of surgery[9,10]. It is essential for the blood clots to adhere firmly to the root surface to achieve proper functional orientation and maturation[10]. Excessive mobility of the surgical flap can lead to the detachment of the blood clot from the root surface, resulting in apical epithelial migration and limited or no periodontal regeneration. In this case, a novel technique was employed to avoid creating incisions in the distal non-keratinized soft tissues, ensuring the stability of the surgical flap and promoting retention of the blood clot within the intrabony defect. This approach facilitates good primary healing, and supports the process of periodontal regeneration. Additionally, our approach, similar to the Entire Papilla Preservation technique described by Aslan et al[11], maintained the integrity and continuity of the distal tissue over the bone crest. This provides an uninterrupted blood supply to the area filled with biomaterial, thereby significantly reducing the risk of biomaterial exposure during the early stages of healing. Consequently, satisfactory outcomes were achieved in terms of periodontal regeneration, although more evidence is required to evaluate the long-term result.
Buccal vertical incision is a commonly employed auxiliary incision in various types of periodontal surgeries. In this modified procedure, the precise location of the vertical incision must consider several critical factors, such as the width of the keratinized gingiva, gingival thickness, and the morphology of the bone defect. When the vertical incision is placed near the intrabony defect, anchoring the suture to the vertical incision alone effectively tightens the distal soft tissue to the root surface, resulting in secure closure of the biomaterial-filled area. Conversely, when a vertical incision is made at the mesiobuccal site of the terminal molar or an adjacent tooth where there is sufficient keratinized tissue, the gingival flap can be easily relaxed. However, relying solely on stitching of the vertical incision often fails to achieve adequate closure of the distal regenerative area. In such situations, a sling suture should be added to the distal tissue to ensure it is close to the root. It is worth noting that some individuals may experience postoperative scarring[12,13]. However, such scarring is typically minimal and inconspicuous, especially in posterior areas.
The modified procedure, involving a distal linear incision shifted to the buccal site of the gingiva and a tunnel-like elevation of the distal tissue, provided a novel approach to accessing the intrabony defect at the distal end of the terminal second molar. Therefore, this procedure offered regenerative opportunities for teeth with non-keratinized mucosa above the intrabony defect.
We extend our sincere gratitude to Nurse Feng Yin for her invaluable assistance in taking the clinical photographs of the patient. Her dedication and expertise contributed greatly to the completeness of our research.
| 1. | Cortellini P, Tonetti MS. Clinical concepts for regenerative therapy in intrabony defects. Periodontol 2000. 2015;68:282-307. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 109] [Cited by in RCA: 186] [Article Influence: 18.6] [Reference Citation Analysis (0)] |
| 2. | Stavropoulos A, Bertl K, Spineli LM, Sculean A, Cortellini P, Tonetti M. Medium- and long-term clinical benefits of periodontal regenerative/reconstructive procedures in intrabony defects: Systematic review and network meta-analysis of randomized controlled clinical studies. J Clin Periodontol. 2021;48:410-430. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 69] [Article Influence: 17.3] [Reference Citation Analysis (0)] |
| 3. | Lang NLJ. Clinical Periodontology and Implant Dentistry: Additional Therapy. 2015; 780. |
| 4. | Nibali L, Sultan D, Arena C, Pelekos G, Lin GH, Tonetti M. Periodontal infrabony defects: Systematic review of healing by defect morphology following regenerative surgery. J Clin Periodontol. 2021;48:100-113. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 91] [Cited by in RCA: 73] [Article Influence: 18.3] [Reference Citation Analysis (0)] |
| 5. | Windisch P, Iorio-Siciliano V, Palkovics D, Ramaglia L, Blasi A, Sculean A. The role of surgical flap design (minimally invasive flap vs. extended flap with papilla preservation) on the healing of intrabony defects treated with an enamel matrix derivative: a 12-month two-center randomized controlled clinical trial. Clin Oral Investig. 2022;26:1811-1821. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 11] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 6. | Sculean A, Nikolidakis D, Nikou G, Ivanovic A, Chapple IL, Stavropoulos A. Biomaterials for promoting periodontal regeneration in human intrabony defects: a systematic review. Periodontol 2000. 2015;68:182-216. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 139] [Cited by in RCA: 192] [Article Influence: 19.2] [Reference Citation Analysis (0)] |
| 7. | Cortellini P, Tonetti MS. Focus on intrabony defects: guided tissue regeneration. Periodontol 2000. 2000;22:104-132. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 205] [Cited by in RCA: 196] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 8. | Matarasso M, Iorio-Siciliano V, Blasi A, Ramaglia L, Salvi GE, Sculean A. Enamel matrix derivative and bone grafts for periodontal regeneration of intrabony defects. A systematic review and meta-analysis. Clin Oral Investig. 2015;19:1581-1593. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 71] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 9. | Susin C, Fiorini T, Lee J, De Stefano JA, Dickinson DP, Wikesjö UM. Wound healing following surgical and regenerative periodontal therapy. Periodontol 2000. 2015;68:83-98. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 69] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 10. | Shaikh MS, Zafar MS, Pisani F, Lone MA, Malik YR. Critical features of periodontal flaps with regard to blood clot stability: A review. J Oral Biosci. 2021;63:111-119. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 11. | Aslan S, Buduneli N, Cortellini P. Entire Papilla Preservation Technique: A Novel Surgical Approach for Regenerative Treatment of Deep and Wide Intrabony Defects. Int J Periodontics Restorative Dent. 2017;37:227-233. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 24] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 12. | Bruno JF. Connective tissue graft technique assuring wide root coverage. Int J Periodontics Restorative Dent. 1994;14:126-137. [PubMed] |
| 13. | Joly JC, Carvalho AM, da Silva RC, Ciotti DL, Cury PR. Root coverage in isolated gingival recessions using autograft versus allograft: a pilot study. J Periodontol. 2007;78:1017-1022. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 51] [Article Influence: 2.8] [Reference Citation Analysis (0)] |