Published online Jun 26, 2024. doi: 10.12998/wjcc.v12.i18.3561
Revised: April 9, 2024
Accepted: May 6, 2024
Published online: June 26, 2024
Processing time: 141 Days and 8.4 Hours
It is well-described that the coronavirus disease 2019 (COVID-19) infection is associated with an increased risk of thrombotic complications. While there have been many cases of pulmonary emboli and deep vein thrombosis in these patients, reports of COVID-19 associated portal vein thrombosis (PVT) have been uncommon. We present a unique case of concomitant PVT and splenic artery thrombosis in a COVID-19 patient.
A 77-year-old-male with no history of liver disease presented with three days of left-sided abdominal pain. One week earlier, the patient was diagnosed with mildly symptomatic COVID-19 and was treated with nirmatrelvir/ritonavir. Physical exam revealed mild right and left lower quadrant tenderness, but was otherwise unremarkable. Significant laboratory findings included white blood cell count 12.5 K/μL, total bilirubin 1.6 mg/dL, aminoaspartate transferase 40 U/L, and alanine aminotransferase 61 U/L. Computed tomography of the abdomen and pelvis revealed acute PVT with thrombus extending from the distal portion of the main portal vein into the right and left branches. Also noted was a thrombus within the distal portion of the splenic artery with resulting splenic infarct. Hypercoagulable workup including prothrombin gene analysis, factor V Leiden, cardiolipin antibody, and JAK2 mutation were all negative. Anticoagulation with enoxaparin was initiated, and the patient’s pain improved. He was discharged on apixaban.
It is quite uncommon for PVT to present simultaneously with an arterial thrombotic occlusion, as in the case of our patient. Unusual thrombotic manifestations are classically linked to hypercoagulable states including malignancy and hereditary and autoimmune disorders. Viral infections such as Epstein-Barr virus, cytomegalovirus, viral hepatitis, and COVID-19 have all been found to increase the risk of splanchnic venous occlusions, including PVT. In our patient, prompt abdominal imaging led to early detection of thrombus, early treatment, and an excellent outcome. This case is unique in that it is the second known case within the literature of simultaneous PVT and splenic artery thrombosis in a COVID-19 patient.
Core Tip: Thromboembolism is a severe but clinically common complication of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection. Thrombotic events classically occur in infected patients who are critically ill, and typically present as deep vein thrombosis or pulmonary embolism. We report a rare case of a patient with SARS-CoV-2 infection complicated by simultaneous portal vein thrombosis and splenic artery thrombosis. A presentation of moderate to severe abdominal pain in SARS-CoV-2 patients should trigger prompt abdominal imaging, as early diagnosis and treatment of splanchnic thrombosis with anticoagulation leads to favorable outcomes.
- Citation: Abramowitz BR, Coles M, Aytaman A, Chander-Roland B, DiLeo DA. Simultaneous portal vein thrombosis and splenic vein thrombosis in a COVID-19 patient: A case report and review of literature. World J Clin Cases 2024; 12(18): 3561-3566
- URL: https://www.wjgnet.com/2307-8960/full/v12/i18/3561.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i18.3561
The coronavirus disease 2019 (COVID-19) infection is associated with a hypercoagulable state and increased risk of thrombotic complications[1]. Although thrombosis in COVID-19 patients can affect any blood vessel, the incidence of venous thromboembolism within these patients is far greater than that of arterial thromboembolism[2,3]. Up to 30% of critically ill COVID-19 patients have been reported to experience either deep vein thrombosis (DVT) or pulmonary embolism (PE)[4]. In contrast, ischemic strokes, acute coronary syndrome, acute limb ischemia, and mesenteric ischemia have only been reported in up to 3.7% of patients[5].
Splanchnic vein thrombosis is an uncommon thrombotic complication of COVID-19[6]. As thrombosis within the portal system can rapidly expand, the clot may progress into the mesenteric venous system, leading to intestinal ischemia[7]. Although splanchnic venous thrombosis is rare, it has been reported in patients with mild COVID-19 infection, including patients without respiratory symptoms[8,9]. We present an exceptionally unique case of simultaneous portal vein thrombosis (PVT) and splenic artery thrombosis in a COVID-19 patient with mild upper respiratory symptoms.
A 77-year-old Caucasian male presented to the emergency room with three days of left-sided abdominal pain.
The patient described his pain as continuous and crampy in character, most severe in the left lower quadrant, and associated with constipation. He denied flank pain, melena, hematochezia, nausea, or vomiting.
The patient had no history of liver disease. One week earlier he tested positive for COVID-19 after experiencing a mild cough and sore throat. He was treated with nirmatrelvir/ritonavir. His upper respiratory symptoms resolved three days after nirmatrelvir/ritonavir initiation.
On presentation, the patient was hemodynamically stable. Physical exam revealed mild right and left lower quadrant tenderness, and was otherwise unremarkable.
Laboratory findings showed a white blood cell count of 12.5 K/μL, hemoglobin of 16.8 g/dL, total bilirubin of 1.6 mg/dL, aspartate aminotransferase of 40 U/L, alanine aminotransferase of 61 U/L, and alkaline phosphatase of 80 U/L. Partial thromboplastin time and international normalized ratio were within normal limits.
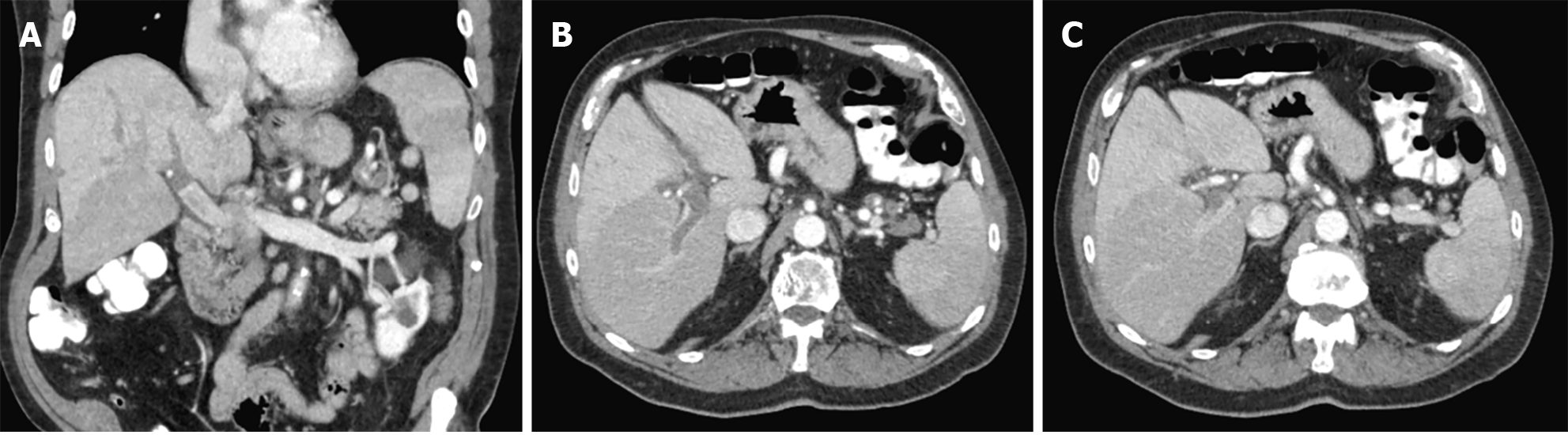
Computed tomography of the abdomen and pelvis (CTAP) revealed acute PVT with the thrombus extending from the distal portion of the main portal vein into the right and left portal branches. Thrombus was also present within the distal portion of the splenic artery with resultant developing splenic infarct. Finally, ill-defined soft tissue was noted in the region of the splenic hilum measuring approximately 2.5 cm, likely reflecting inflammatory changes, though an exophytic pancreatic lesion could not be ruled out (Figure 1).
Hypercoagulable workup including prothrombin gene analysis, factor V Leiden, cardiolipin antibody, and JAK2 mutation were obtained and later all resulted negative.
Based on the imaging findings, the patient was diagnosed with both PVT and splenic artery thrombosis.
Anticoagulation was initiated promptly with full dose enoxaparin. After three days, the patient reported complete resolution of his abdominal pain. He was discharged on a 6-month course of apixaban.
The patient returned for magnetic resonance imaging (MRI) of his abdomen eight weeks after discharge. He denied any recurrence of abdominal pain since his hospitalization. MRI revealed reperfusion of the portal vein and the previously visualized soft tissue density noted in the CTAP was no longer seen, ruling out an exophytic pancreatic lesion.
Thrombosis is a serious complication of COVID-19, which has significantly contributed to its morbidity and mortality throughout the pandemic[10]. Several retrospective studies have shown the incidence of thromboembolism in patients admitted to intensive care units to be quite high, with one study revealing an incidence rate of 69%[11]. DVT and PE comprise the main bulk of cases of thromboembolism in COVID-19 patients, but the virus does increase the general risk of thromboembolism within all vasculature, including the splanchnic circulation, as in the case of our patient.
Delineating the pathophysiology behind thrombosis in COVID-19 infection is key to understanding the increased thrombotic risk in these patients. The SARS-CoV-2 virus primarily infects and enters endothelial cells through membrane-bound angiotensin converting enzyme-2 (ACE2) receptors[12,13]. Once inside the cell, the virus is able to hijack its host cell machinery in order to replicate viral RNA, perform particle assembly, and release an even greater viral load back into the extracellular environment. The infected endothelial cells accrue damage that leads to cell dysfunction, pyroptosis, and apoptosis, which leads to increased vascular permeability[14,15]. Recognition of viral RNA by the innate immune system results in the production of pro-inflammatory cytokines[16]. Massive cytokine build-up allows for the pouring of both innate and adaptive immune cells into the vasculature in the setting of acutely increased permeability, which is subsequently followed by widespread platelet activation[17]. Additionally, damaged endothelial cells lose their physio
Although the risk of splanchnic vein thrombosis is higher in COVID-19 patients than the average population, its incidence within the infected population has been reported to be as low as 0.6%, far below that of DVT or PE[19]. The most common subtype of splanchnic vein thrombosis in COVID-19 patients is PVT, followed by mesenteric vein thrombosis, splenic vein thrombosis, and Budd-Chiari syndrome[20]. Although thrombotic risk is elevated with increased severity of COVID-19 infection, thrombosis can still be diagnosed in mild and even asymptomatic COVID-19 infections[21]. In our case, the patient only experienced mild upper respiratory symptoms that had already resolved before he began to develop thrombotic-related clinical symptoms. Therefore, thrombotic risk still exists in COVID-19 patients whose symptoms may have already resolved.
The incidence of arterial thromboembolism in COVID-19 is significantly lower than that of venous thromboembolism, with the most common subtypes being acute coronary syndrome followed by ischemic stroke, and acute limb ischemia[22]. Splanchnic arterial thromboembolism in COVID-19, such as the splenic artery thrombosis that occurred in our patient, is even rarer. There is only one additional known case within the literature of simultaneous PVT and splenic artery thrombosis in a COVID-19 patient[23].
As PVT in COVID-19 patients has been found to have mortality rates up to 16%, early diagnosis and treatment is imperative[24]. Presenting clinical symptoms typically involve abdominal pain and are otherwise non-specific. Thus, imaging with CT scan, ultrasound, or MRI will facilitate the diagnosis[25,26]. Once the diagnosis is made, treatment with anticoagulation must be prioritized, as early anticoagulation has been associated with positive outcomes[27,28]. Low molecular weight heparin (LMWH) is often utilized as the primary anticoagulant of choice in COVID-19 patients rather than direct oral anticoagulants, as LMWH is less likely to have negative drug interactions with antiviral therapies[29,30].
As dozens of cases of COVID-associated PVT have been reported ever since the start of the pandemic with relatively high mortality rates, it is important for clinicians to have PVT within the differential for COVID-19 patients presenting with abdominal pain. In our patient, prompt abdominal imaging led to early detection of thrombus with early treatment and an excellent outcome. This case is quite unique in that it is only the second known imaging confirmed case within the literature of simultaneous PVT and splenic artery thrombosis in a COVID-19 patient.
Thromboembolism is a severe potential complication of COVID-19 infection. Thrombosis more commonly affects venous circulation within the extremities or the pulmonary vessels, but it can also affect splanchnic vessels. Although it is relatively rare, splanchnic thrombosis should be on the differential in a patient presenting with abdominal pain in the setting of a COVID-19 infection. Our case was quite unique in that the patient presented with both portal vein and splenic artery thrombosis simultaneously. As previous literature has shown, timely imaging and early treatment with anticoagulation resulted in a positive outcome in our patient.
| 1. | Al-Ani F, Chehade S, Lazo-Langner A. Thrombosis risk associated with COVID-19 infection. A scoping review. Thromb Res. 2020;192:152-160. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 304] [Cited by in RCA: 273] [Article Influence: 54.6] [Reference Citation Analysis (0)] |
| 2. | Ten Berg J. Venous and arterial thromboembolic disease in COVID-19. J Thromb Thrombolysis. 2021;52:1007-1009. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 3. | Violi F, Ceccarelli G, Cangemi R, Cipollone F, D'Ardes D, Oliva A, Pirro M, Rocco M, Alessandri F, D'Ettorre G, Lichtner M, Pignatelli P, Ferro D, Ruberto F, Lip GYH, Pugliese F, Mastroianni CM; Intensive Care, Infectious Diseases COVID-19 Study Group of Sapienza University. Arterial and venous thrombosis in coronavirus 2019 disease (Covid-19): relationship with mortality. Intern Emerg Med. 2021;16:1231-1237. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 24] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 4. | Angelini DE, Kaatz S, Rosovsky RP, Zon RL, Pillai S, Robertson WE, Elavalakanar P, Patell R, Khorana A. COVID-19 and venous thromboembolism: A narrative review. Res Pract Thromb Haemost. 2022;6:e12666. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 13] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 5. | Duhailib ZA, Oczkowski S, Polok K, Fronczek J, Szczeklik W, Piticaru J, Mammen MJ, Alshamsi F, Eikelboom J, Belley-Cote E, Alhazzani W. Venous and arterial thrombosis in COVID-19: An updated narrative review. J Infect Public Health. 2022;15:689-702. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 7] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 6. | Sharma N, Shukla R, Kumar K, Arora S, Warrier R, Philip S. Portal Vein Thrombosis-a Rare Complication of SARS-CoV-2 Infection. SN Compr Clin Med. 2021;3:1416-1419. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 7. | Costache RS, Dragomirică AS, Dumitraș EA, Mariana J, Căruntu A, Popescu A, Costache DO. Portal vein thrombosis: A concise review (Review). Exp Ther Med. 2021;22:759. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 13] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 8. | Buso G, Becchetti C, Berzigotti A. Acute splanchnic vein thrombosis in patients with COVID-19: A systematic review. Dig Liver Dis. 2021;53:937-949. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 18] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 9. | Singh B, Kaur P, Maroules M. Splanchnic vein thrombosis in COVID-19: A review of literature. Dig Liver Dis. 2020;52:1407-1409. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 20] [Cited by in RCA: 22] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 10. | Gonzalez-Fajardo JA, Ansuategui M, Romero C, Comanges A, Gómez-Arbeláez D, Ibarra G, Garcia-Gutierrez A. Mortality of COVID-19 patients with vascular thrombotic complications. Med Clin (Engl Ed). 2021;156:112-117. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 19] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 11. | Nahum J, Morichau-Beauchant T, Daviaud F, Echegut P, Fichet J, Maillet JM, Thierry S. Venous Thrombosis Among Critically Ill Patients With Coronavirus Disease 2019 (COVID-19). JAMA Netw Open. 2020;3:e2010478. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 177] [Cited by in RCA: 237] [Article Influence: 47.4] [Reference Citation Analysis (0)] |
| 12. | Gąsecka A, Borovac JA, Guerreiro RA, Giustozzi M, Parker W, Caldeira D, Chiva-Blanch G. Thrombotic Complications in Patients with COVID-19: Pathophysiological Mechanisms, Diagnosis, and Treatment. Cardiovasc Drugs Ther. 2021;35:215-229. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 90] [Cited by in RCA: 99] [Article Influence: 24.8] [Reference Citation Analysis (0)] |
| 13. | Ali MAM, Spinler SA. COVID-19 and thrombosis: From bench to bedside. Trends Cardiovasc Med. 2021;31:143-160. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 65] [Cited by in RCA: 141] [Article Influence: 28.2] [Reference Citation Analysis (0)] |
| 14. | Bittner ZA, Schrader M, George SE, Amann R. Pyroptosis and Its Role in SARS-CoV-2 Infection. Cells. 2022;11:1717. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19] [Cited by in RCA: 26] [Article Influence: 8.7] [Reference Citation Analysis (0)] |
| 15. | Otifi HM, Adiga BK. Endothelial Dysfunction in Covid-19 Infection. Am J Med Sci. 2022;363:281-287. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 84] [Article Influence: 28.0] [Reference Citation Analysis (0)] |
| 16. | Jing H, Wu X, Xiang M, Liu L, Novakovic VA, Shi J. Pathophysiological mechanisms of thrombosis in acute and long COVID-19. Front Immunol. 2022;13:992384. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 44] [Article Influence: 14.7] [Reference Citation Analysis (0)] |
| 17. | Becker RC, Sexton T, Smyth S; International COVID-19 Thrombosis Biomarkers Colloquium (ICODE) Investigators. COVID-19 and biomarkers of thrombosis: focus on von Willebrand factor and extracellular vesicles. J Thromb Thrombolysis. 2021;52:1010-1019. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 9] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 18. | Birnhuber A, Fließer E, Gorkiewicz G, Zacharias M, Seeliger B, David S, Welte T, Schmidt J, Olschewski H, Wygrecka M, Kwapiszewska G. Between inflammation and thrombosis: endothelial cells in COVID-19. Eur Respir J. 2021;58:2100377. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 20] [Cited by in RCA: 106] [Article Influence: 26.5] [Reference Citation Analysis (0)] |
| 19. | Zheng X, Gao F, Wang L, Meng Y, Ageno W, Qi X. Incidence and outcomes of splanchnic vein thrombosis after diagnosis of COVID-19 or COVID-19 vaccination: a systematic review and meta-analysis. J Thromb Thrombolysis. 2023;55:18-31. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 7] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 20. | Deltenre P, Payancé A, Elkrief L, La Mura V, Artru F, Baiges A, Cervoni JP, China L, Colle I, Lemaitre E, Procopet B, Schiller D, Bureau C, Goria O, Ollivier I, Nuzzo A, Rautou PE, Plessier A; for VALDIG, an EASL consortium. Splanchnic vein thrombosis associated with SARS-CoV-2 infection: A VALDIG case-control study. JHEP Rep. 2023;5:100894. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 21. | Cheng NM, Chan YC, Cheng SW. COVID-19 related thrombosis: A mini-review. Phlebology. 2022;37:326-337. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 21] [Reference Citation Analysis (0)] |
| 22. | Kunutsor SK, Laukkanen JA. Incidence of venous and arterial thromboembolic complications in COVID-19: A systematic review and meta-analysis. Thromb Res. 2020;196:27-30. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 48] [Cited by in RCA: 68] [Article Influence: 13.6] [Reference Citation Analysis (0)] |
| 23. | Rehman A, Thoppil AJ, Wallach SL. Portal Vein Thrombosis and Splenic Infarction in a COVID-19 Patient. Cureus. 2021;13:e16843. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 24. | El-Hady HA, Mahmoud Abd-Elwahab ES, Mostafa-Hedeab G, Shawky Elfarargy M. Portal vein thrombosis in patients with COVID-19: A systematic review. Asian J Surg. 2023;46:3017-3026. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 9] [Reference Citation Analysis (0)] |
| 25. | Jafari SH, Naseri R, Khalili N, Haseli S, Bahmani M. Portal vein thrombosis associated with COVID-19: points to consider. BJR Case Rep. 2020;6:20200089. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 26. | Shrestha PS, Ishak A, Napit AR, Sarwar S, Rai N, Nizami Z, Bheemisetty N, Jayaraj P, Shrestha A, Rodriguez ID. Portal vein thrombosis as a thrombotic complication of COVID-19 mRNA vaccine: A case report and literature review. IDCases. 2022;29:e01582. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 27. | Sinz S, Glaser-Gallion F, Steffen T. Portal vein thrombosis in COVID-19 infection. Surg Case Rep. 2021;7:87. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 9] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 28. | Akella R, Raj R, Kannan L, Jacob A. Coexisting portal vein thrombosis and aortic thrombosis in a patient with COVID-19: A case report and literature review. IDCases. 2022;28:e01509. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 29. | Kreidieh F, Temraz S. Anticoagulation for COVID-19 Patients: A Bird's-Eye View. Clin Appl Thromb Hemost. 2021;27:10760296211039288. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 12] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 30. | Ahuja N, Bhinder J, Nguyen J, Langan T Jr, O'Brien-Irr M, Montross B, Khan S, Sharma AM, Harris LM. Venous thromboembolism in patients with COVID-19 infection: risk factors, prevention, and management. Semin Vasc Surg. 2021;34:101-116. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 9] [Article Influence: 2.3] [Reference Citation Analysis (0)] |