Published online Jun 26, 2024. doi: 10.12998/wjcc.v12.i18.3534
Revised: February 20, 2024
Accepted: April 25, 2024
Published online: June 26, 2024
Processing time: 158 Days and 5.5 Hours
Conjoined twins are a rare twin malformation commonly presenting as single am
A woman of childbearing age conceived naturally, and at 8 wk of gestation, transvaginal ultrasonography showed an embryo and cardiac tube pulsation in both amniotic sacs. On dynamic observation, the two embryos were connected in the lower abdomen, with restricted movement. A repeat transvaginal ultrasound at 11 wk showed that the intestinal tubes of both fetuses were connected in the lower abdomen. The pregnancy was terminated and labor was induced.
Transvaginal ultrasound may detect conjoined twin malformations in an early stage. Our case provides diagnostic insights for ultrasonographers and can help develop early therapeutic interventions.
Core Tip: We recently diagnosed a case of bi-amniotic sac conjoined twin fetuses at 8 wk of gestation, reports of such cases are rare nationally and globally. We provide insights into the early diagnosis and treatment of conjoined twin fetuses for colleagues.
- Citation: Liang ZQ, Ding WQ. Twin fetuses associated with double amniotic sacs diagnosed using transvaginal ultrasonography: A case report. World J Clin Cases 2024; 12(18): 3534-3538
- URL: https://www.wjgnet.com/2307-8960/full/v12/i18/3534.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i18.3534
Conjoined twins are a twin malformation caused by abnormal embryo development, commonly presenting as single amniotic sac twinning, with an incidence of 1.5/100000 and associated with a high stillbirth rate[1,2]. Congenital anomalies, which are consistently present in the case of joined twins, may affect the survival of one or both fetuses even if they are surgically separated after birth[3]. According to the site of fusion, conjoined twins can be classified as cephalic, thoracic, umbilical, sciatic, parasitic, cranial, spinal, or breech union[4]. Early screening for conjoined twins using ultrasonography (color Doppler, fetal echocardiography, or 3D ultrasonography) is currently available[5,6], and this abnormality can generally be evaluated around 12 wk of gestation[7].
We recently diagnosed a case of bi-amniotic sac conjoined twin fetuses at 8 wk of gestation, presenting with one chorionic villus sac, one yolk sac, two amniotic sacs, intestinal connection via a defect in the abdominal wall and cloacal abnormality, and umbilical cord abnormality. Reports of such cases are rare, both nationally and globally. By sharing the diagnosis and treatment of this case and reviewing the relevant literature, in this case report we aim to provide insights into the early diagnosis and treatment of conjoined twin fetuses for colleagues.
A woman of childbearing age, with two pregnancies and one birth, conceived naturally and underwent the first early pregnancy ultrasound examination in our department at 8 wk of pregnancy.
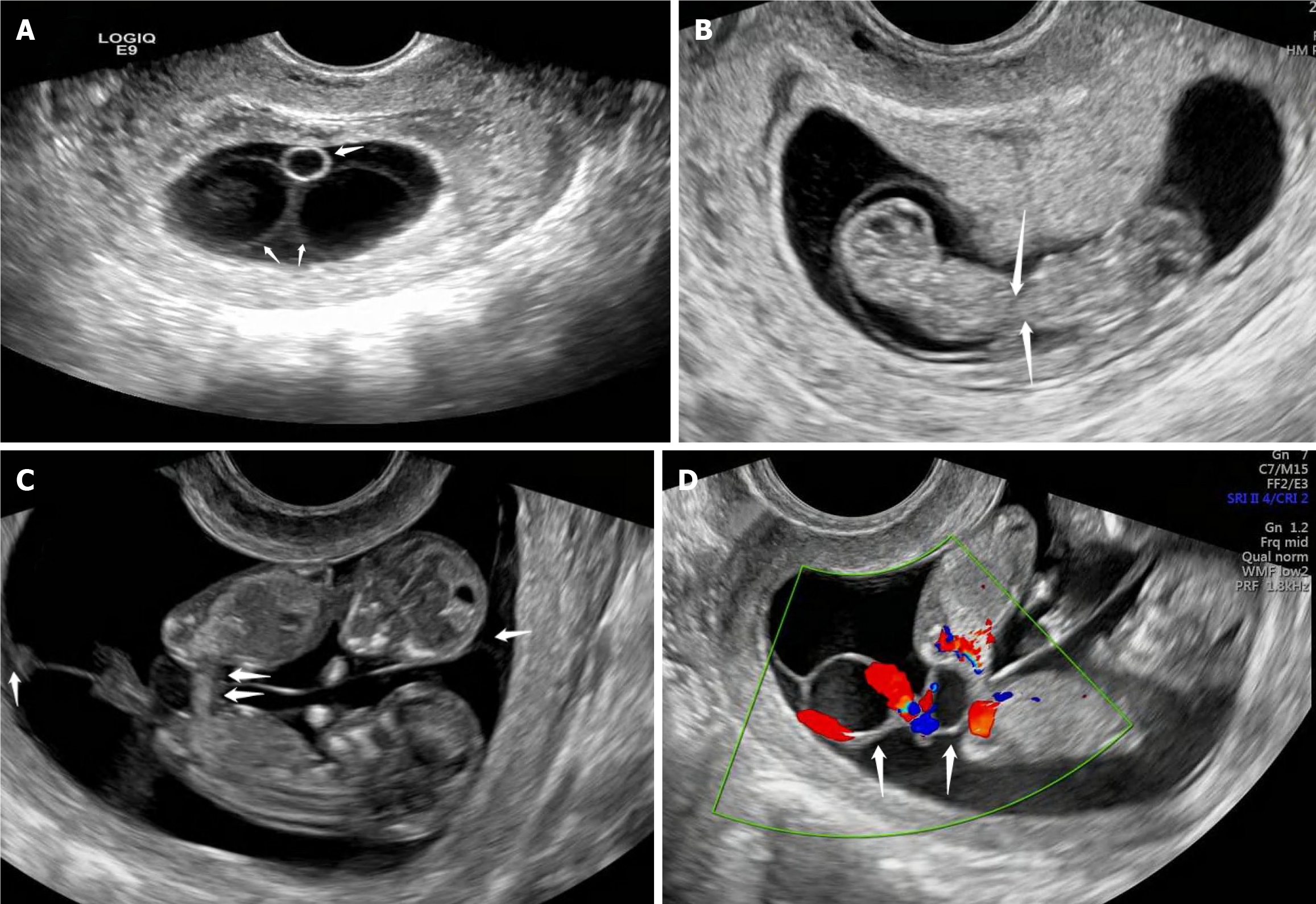
Transvaginal ultrasonography showed a gestational sac in the uterine cavity, with an amniotic membrane separating the sacs, and a yolk sac was visible at one end of the sac (Figure 1A). A single embryo and cardiac tubular pulsation were observed in both amniotic sacs, and the embryos were linked in the lower abdomen, with limited mobility, by dynamic observation (Figure 1B). Repeat transvaginal ultrasonography at 11 wk of gestation showed a connection of the intestinal tubes in the lower abdomen of both fetuses (Figure 1C). Doppler ultrasonography showed that there was no free-floating umbilical cord, and the umbilical vessels were intertwined, forming a common umbilical cord in the area of the twin fetuses' connection, and two anechoic cysts were observed in the amniotic septum (Figure 1D). Multiple umbilical vessels were coiled around the anechoic cysts and inserted along the amniotic septum in front of the placental inlet in a forked manner.
The patient had no previous heart, lung, liver, or kidney disorders, no chronic diseases—such as hypertension or diabetes mellitus—no bleeding tendency, history of allergies, or epidemiologic history.
There was a critical risk of early Down’s syndrome in the first pregnancy, risk of trisomy 211:452, normal NT, and risk of noninvasive DNA, although the patient experienced a normal delivery and her child is currently alive. A family history of genetic disease was denied. There was no family history of twin births.
Vital signs were normal, including well-proportioned, well-nourished, normal face, and normal heart, lungs, and abdomen.
Doppler ultrasonography showed that there was no free-floating umbilical cord, and the umbilical vessels were intertwined, forming a common umbilical cord in the area of the twin fetuses' connection, and two anechoic cysts were observed in the amniotic septum (Figure 1D).
Double amniotic sacs.
Given that the intestinal contents of the twin fetuses were clearly connected, a final diagnosis of monochorionic bi-amniotic twin fetuses was made. The patient chose to terminate her pregnancy at 11 wk.
After labor induction, the excretory tissue confirmed the presence of only one placenta, one yolk sac, an umbilical cord containing six blood vessels, split amniotic septa attached to the center of the placenta, and ventral cleft deformities in both fetuses (Figure 2). Chromosomal analyses of the excretory tissues revealed no abnormalities.
The etiology and pathogenesis of conjoined twins remain unclear. In addition to genetic factors, external factors are crucial causal factors. Exposure of the mother to adverse environmental conditions during preconception and early pregnancy may lead to abnormal embryo division[8]. The developmental mechanism of monochorionic bi-amniotic twin embryos can be explained by the fission and fusion theories. Kapur et al[9] were the first to propose the hypothesis of incomplete secondary fission of embryonic development, where a single amniotic cavity starts with a single embryonic disk. Two protostrips form in one disk because of defects in protoganglionic embryo formation, and as the protostrips develop towards the ends to form two new embryonic disks: the amniotic sacs become smaller where the two disks fold. Eventually, the amniotic membrane forms two amniotic sacs by attaching to the embryo only in the umbilical cord region. However, this hypothesis failed to explain the ventral cleft deformity and intestinal abnormalities reported in the literature.
The fusion hypothesis, later proposed by Spencer[10], is more acceptable. It states that the two embryonic discs are formed in two different amniotic cavities, and since there is only one yolk sac and the two discs fuse at the umbilicus during development, the subumbilical abdominal wall is formed in the region of the urothelium and caudal to the yolk sac. The fusion of this region interferes with the formation of the subumbilical abdominal wall, resulting in the joining of the adjacent intestinal tubes, leading to the development of a double amniotic sac. Spencer's fusion hypothesis seems to be more applicable to the present case of bi-amniotic sac conjoined twin fetuses, and fusion in the lower abdomen is most likely; there are no reports of double amniotic twin fetuses outside of the abdominal junction site.
It is generally accepted that the number of yolk sacs is equal to the number of amniotic sacs, but the possibility of two amniotic sacs existing in one yolk sac was demonstrated by the current case. In line herewith, Shen et al[11] concluded that the number of yolk sacs does not predict the number of amniotic sacs within a single chorioallantoic sac, and that yolk sac formation occurs before amniotic differentiation and after chorioallantoic differentiation. It has been hypothesized that a single yolk sac represents a single urothelium because the urothelium is a small diverticulum in the tail of the yolk sac[12]. According to Spencer's fusion theory, the single yolk sac and its urothelium induce the formation of a common somite, suggesting potential herniation of the umbilical vessels and intestines into the extraembryonic somite. In addition, there is an increased risk of possible congenital defects in single yolk sacs in conjoined twins[13]. Another important feature of monochorionic conjoined twins is the common umbilical cord or urachus[13]. In the present case, using Doppler ultrasonography, it was possible to observe separate umbilical vessels in the twin fetuses. After exiting the umbilical orifice, these vessels intertwined with each other in a common umbilical cord and inserted in a bifurcated manner along the amniotic septum in front of the entrance to the placenta.
Conjoined twins have a higher risk of stillbirth and poorer prognosis, even after delivery. Surgical separation is difficult and expensive, posing a great burden on the family and society[14]. Moreover, the ethical issues involved in the separation of conjoined twins are controversial[15]. Therefore, early diagnosis and pregnancy termination or necessary interventions are essential[16]. Prenatal ultrasound diagnosis of conjoined twins is based on a number of features: fetus lying in a fixed position, head and body parts constantly at the same level, inseparable body and skin contours, and sharing of organs by fetuses facing each other. Further, some conjoined twins may have fewer limbs than normal twins, a single placenta, and no amniotic fluid separation. However, in the current case, there was amniotic separation; therefore, observing amniotic fluid separation cannot rule out the possibility of conjoined twins. Transvaginal ultrasonography in this case aided in the visualization of the embryos and appendages, including chorionicity, amniotic cysticity, number of yolk sacs, site of twin attachment, and umbilical vessel alignment. Given the early stage of pregnancy in the present case, the observation of the fetal structures was limited, and the fetal bladder, cloacal cavity, and number of umbilical blood vessels could not be clearly observed. If necessary, magnetic resonance or computed tomographic examination can be performed[17].
Although the embryological basis of co-twinning remains unclear, our case suggests the possibility of co-twinning in monochorionic bi-amniotic sac twins, and transvaginal ultrasonography facilitates the diagnosis of co-twinning in early pregnancy and the visualization of fetal and appendage structures, which can help in the early decision of further pregnancy management.
The incidence of conjoined twins is low; however, this malformation is accompanied by congenital anomalies. In such twins, most vital organs are connected. Only a few twin malformations can be separated surgically. Early diagnosis and treatment are necessary, and transvaginal ultrasound may allow for early detection. Our case provides guidance for ultrasonographers in the diagnostic process and can help formulate therapeutic measures to intervene in an early stage.
| 1. | Liu H, Deng C, Hu Q, Liao H, Wang X, Yu H. Conjoined twins in dichorionic diamniotic triplet pregnancy: a report of three cases and literature review. BMC Pregnancy Childbirth. 2021;21:687. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 2. | Mutchinick OM, Luna-Muñoz L, Amar E, Bakker MK, Clementi M, Cocchi G, da Graça Dutra M, Feldkamp ML, Landau D, Leoncini E, Li Z, Lowry B, Marengo LK, Martínez-Frías ML, Mastroiacovo P, Métneki J, Morgan M, Pierini A, Rissman A, Ritvanen A, Scarano G, Siffel C, Szabova E, Arteaga-Vázquez J. Conjoined twins: a worldwide collaborative epidemiological study of the International Clearinghouse for Birth Defects Surveillance and Research. Am J Med Genet C Semin Med Genet. 2011;157C:274-287. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 101] [Cited by in RCA: 123] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 3. | Spitz L. Conjoined twins. Prenat Diagn. 2005;25:814-819. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 86] [Cited by in RCA: 91] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 4. | Spencer R. Anatomic description of conjoined twins: a plea for standardized terminology. J Pediatr Surg. 1996;31:941-944. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 132] [Cited by in RCA: 114] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 5. | Mian A, Gabra NI, Sharma T, Topale N, Gielecki J, Tubbs RS, Loukas M. Conjoined twins: From conception to separation, a review. Clin Anat. 2017;30:385-396. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 42] [Article Influence: 5.3] [Reference Citation Analysis (1)] |
| 6. | Mathew RP, Francis S, Basti RS, Suresh HB, Rajarathnam A, Cunha PD, Rao SV. Conjoined twins - role of imaging and recent advances. J Ultrason. 2017;17:259-266. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 32] [Cited by in RCA: 31] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 7. | Johnston I. Conjoined twins. Lancet. 2001;357:149. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 8. | Spitz L, Kiely EM. Conjoined twins. JAMA. 2003;289:1307-1310. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 101] [Cited by in RCA: 82] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 9. | Kapur RP, Jack RM, Siebert JR. Diamniotic placentation associated with omphalopagus conjoined twins: implications for a contemporary model of conjoined twinning. Am J Med Genet. 1994;52:188-195. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 25] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 10. | Spencer R. Minimally united ischiopagus twins: infraumbilical union with cloacal anomalies. J Pediatr Surg. 1996;31:1538-1545. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 16] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 11. | Shen O, Samueloff A, Beller U, Rabinowitz R. Number of yolk sacs does not predict amnionicity in early first-trimester monochorionic multiple gestations. Ultrasound Obstet Gynecol. 2006;27:53-55. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 27] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 12. | Xiang G, Wen Y, Zhang L, Tong X, Li L. Three-dimensional ultrasonographic features of diamniotic conjoined twins with body stalk anomaly. BMC Pregnancy Childbirth. 2020;20:221. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 5] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 13. | Poláková M, Zetová L, Vlk R, S V. [Monochorionic biamniotic twins with a common yolk sac in the first trimester ultrasound scan - is there a higher risk of a congenital defect?]. Ceska Gynekol. 2012;77:521-523. [PubMed] |
| 14. | Spitz L. Ethics in the management of conjoined twins. Semin Pediatr Surg. 2015;24:263-264. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 16] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 15. | Lee M, Gosain AK, Becker D. The bioethics of separating conjoined twins in plastic surgery. Plast Reconstr Surg. 2011;128:328e-334e. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 17] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 16. | Wheeler R. Conjoined twins: Surgically and legally exceptional. Arch Dis Child. 2021;106:1158-1159. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 17. | Kattel P. Conjoined Twins. JNMA J Nepal Med Assoc. 2018;56:708-710. [PubMed] |