Published online Jun 26, 2024. doi: 10.12998/wjcc.v12.i18.3438
Revised: April 28, 2024
Accepted: May 14, 2024
Published online: June 26, 2024
Processing time: 99 Days and 20.9 Hours
Ultrasound-guided prostate biopsy is a reliable diagnostic procedure for prostate cancer diagnosis with minimal procedure-related trauma. However, complications, such as massive rectal bleeding may occur after the puncture. We hypothesized that using a transrectal resectoscope could help treat massive rectal bleeding after transrectal prostate punctures.
To identify a simple and effective treatment for massive rectal bleeding after transrectal prostate punctures.
Patients requiring treatment for massive rectal bleeding after transrectal prostate punctures were included. A SIMAI resectoscope was inserted through the anus. Direct electrocoagulation was performed for superficial bleeding points. Part of the rectal mucosa or surface muscle layer was removed to expose deep bleeding points, followed by electrocoagulation. An electric cutting ring was used to compress and stop the bleeding for jet-like points before electrocoagulation. The fluid color in the drainage tube was monitored postoperatively for continuous bleeding.
Eight patients were included from 2012 to 2022. None of the patients with massive rectal bleeding after the transrectal prostate punctures improved with conventional conservative and blood transfusion treatments. Two patients had an inferior artery embolism, and digital subtraction angiography was ineffective. All patients received emergency transanal prostate resection, which immediately stopped the bleeding. Four days after the procedure, the patients had recovered and were discharged.
Using a transanal prostate resection instrument is a simple, safe, and effective method for treating massive rectal bleeding after transrectal prostate punctures.
Core Tip: This report describes the treatment of eight patients with massive rectal bleeding after a transrectal prostate puncture using a prostate resectoscope. After massive rectal bleeding, in addition to systemic treatment, the commonly used local treatment methods are often ineffective or traumatic, risking further aggravation. Herein, we describe our experience using a prostate resectoscope to successfully treat superficial, deep, and jet-like bleeding points in patients with massive rectal bleeding after a transrectal prostate puncture, presenting a novel and minimally invasive treatment approach with several advantages over other surgical treatment methods.
- Citation: Li HM, Yang FY, Tu S, Yan P, Qian J, Yao JX. Application of prostate resectoscope in the treatment of massive rectal bleeding after transrectal prostate puncture. World J Clin Cases 2024; 12(18): 3438-3443
- URL: https://www.wjgnet.com/2307-8960/full/v12/i18/3438.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i18.3438
Prostate biopsy is the most reliable diagnostic procedure for prostate cancer diagnosis[1]. Ultrasound-guided transrectal prostate biopsy is a commonly used diagnostic method in urology[2]. In general, procedure-related trauma is minimal; however, other complications may occur, including massive rectal bleeding and systemic infection after the puncture. The rectal bleeding rate ranges from 11.5% to 40%, and, in severe cases, patients may die of hemorrhagic shock[3]. In recent years, our institution has achieved satisfactory results in the treatment of massive rectal bleeding after transrectal prostate punctures using a transrectal resectoscope.
From August 2016 to August 2022, eight patients had obvious hematochezia within 24 h after transrectal prostate biopsy; the amount of blood loss ranged from 600 to 1500 mL. Two patients experienced hemorrhagic shock, and conservative treatment and blood transfusions were ineffective. Two patient had an artery embolism, and treatment with digital subtraction angiography was ineffective. All patients were treated using transanal prostate resection instruments during the emergency period, which immediately stopped the bleeding. The patients recovered and were discharged four days after the procedure.
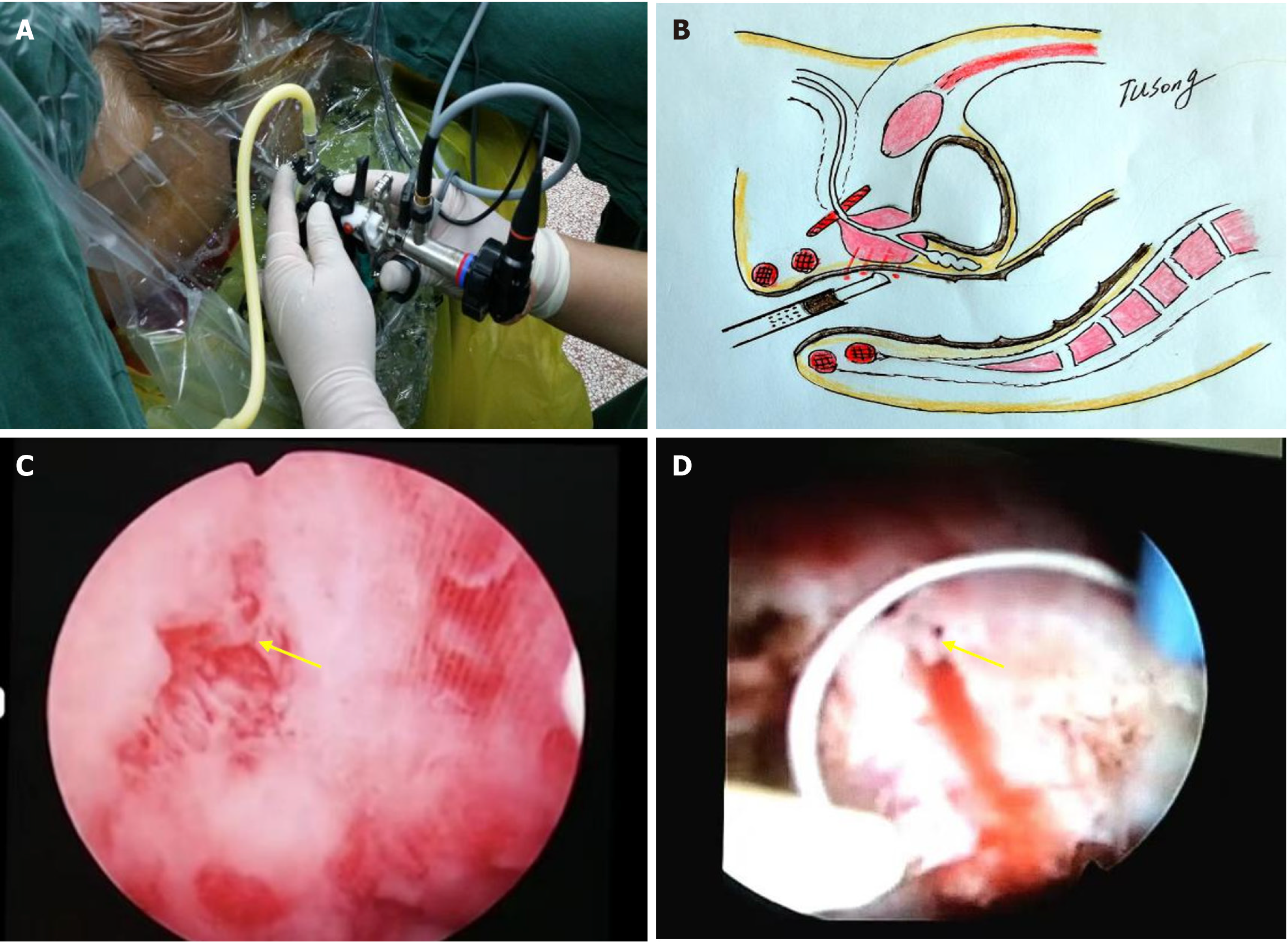
In the lithotomy position, the head was 30° higher than the feet to reduce upward perfusion of the rectal flushing fluid. No anesthesia was required, and pain-relieving and sedative drugs were administered when necessary. The left lower abdomen was properly pressurized with cotton pads to prevent the washing liquid from ascending to the descending colon and to reduce the absorption of the washing liquid and thus retain it after the operation. Prostate resection instrumentation was used; the effective length was 20 cm, and the diameter was 8.3 mm (26 Fr) (Figure 1A and B). The flushing fluid was a 0.9% sodium chloride solution, and the pressure was maintained with a 40 cm water column. The electric cutting power was 280 W, and the electric coagulation power was 180 W.
With direct visualization, we inserted the endoscope through the anus, thoroughly checked the rectum and prostate puncture site (anterior wall of the rectum), carefully looked for bleeding points, and observed each puncture point as clearly as possible (generally 12 puncture points) (Figure 1C). In presence of obvious blood accumulation or blood clots in the rectum, the site was first flushed with normal saline to ensure a clear visual field for the operation. Direct electrocoagulation was performed for superficial rectal bleeding. For deep bleeding points, part of the rectal mucosa or muscle layer on the surface was removed, and electrocoagulation was used to stop bleeding after clearly exposing the bleeding point. For jet-like bleeding points, an electric cutting ring was used to compress and stop the bleeding before electrocoagulation (Figure 1D; Video). Preventive electrocoagulation was also used at the suspected bleeding sites to prevent later bleeding. After hemostasis, the flushing solution was stopped, and the patient was carefully observed to ensure that no venous bleeding occurred when the rectum was not under pressure. Accumulated blood and intestinal contents in the rectum were thoroughly flushed and removed, and a rectal drainage tube was retained through the anus to drain the rectal residual flushing fluid and decompress the rectum.
Postoperative bleeding through the drainage tube was monitored, and the drainage tube was removed 24 h later if no bleeding or only a small amount of bleeding occurred. After the operation, the patients’ diet was changed from a liquid to a regular diet, and the patients were discharged.
We conducted electrosurgical examination in eight patients with rectal bleeding after puncture. Each patient experienced rectal bleeding and received conventional treatment with unsatisfactory results. Two patients underwent a blood transfusion and digital subtraction angiography hemostasis due to considerable uncontrolled bleeding. All patients underwent an electrosurgical examination; six had mild bleeding, one had several bleeding puncture points, and one had arterial bleeding. The bleeding was successfully stopped for all patients using a transurethral prostate resection instrument, resulting in immediate hemostasis and good therapeutic effects. The patients remained stable and were discharged after surgery. Imaging and pathological examination results showed that all eight patients had advanced-stage prostate cancer, and continued to receive treatment for metastatic prostate cancer. Furthermore, two patients had oligometastasis, both of whom requested surgical treatment. One patient requested transurethral prostatic resection treatment to resolve their urinary obstruction. All patients were subsequently treated with androgen deprivation therapy combined with abiraterone-acetate or enzalutamide (Table 1). To date, all the patients are undergoing follow-up, and their tumor control outcomes are satisfactory.
| Case No. | Age (yr) | PSA (ng/mL) | Histopathology | TNM | Gleason | Post puncture treatment | Subsequent treatment |
| 1 | 54 | 40.24 | Adenocarcinoma | T3N1M1b | 4 + 3 | CT + TUPRI | ADT + AA |
| 2 | 66 | 140.21 | Adenocarcinoma | T3N1M1b | 4 + 5 | CT + TUPRI | ADT + AA |
| 3 | 76 | 112.67 | Adenocarcinoma | T3N1M1b | 4 + 3 | CT + Transfusion + DSA + TUPRI | ADT + Enzalutamide |
| 4 | 56 | 99.46 | Adenocarcinoma | T3N1M1b | 4 + 4 | CT + TUPRI | RARP + ADT + AA |
| 5 | 71 | 122.35 | Adenocarcinoma | T3N1M1a | 4 + 3 | CT + TUPRI | TUVP + ADT |
| 6 | 66 | 65.61 | Adenocarcinoma | T3N1M1a | 4 + 4 | CT + Transfusion + DSA + TUPRI | LRP + ADT + AA |
| 7 | 82 | 652.64 | Adenocarcinoma | T3N1M1b | 5 + 4 | CT + TUPRI | ADT + Enzalutamide |
| 8 | 76 | 126.13 | Adenocarcinoma | T3N1M1a | 5 + 3 | CT + TUPRI | ADT + Enzalutamide |
Transrectal prostate biopsy is a commonly used diagnostic procedure in urology[4]. However, the puncture itself causes needle track trauma to the rectal wall and prostate; therefore, puncture injury-related complications, such as rectal bleeding, bladder or urinary tract bleeding, and infection, may occur, some of which can be severe, such as massive rectal bleeding and sepsis[5]. Severe massive bleeding can cause hemorrhagic shock, endangering the patient’s life[6].
The more the puncture points, the greater the possibility of bleeding[7]. The total incidence of rectal bleeding after transrectal prostate biopsy ranges from 11.5% to 40%[3]. Most rectal bleeding will naturally stop after the puncture, requiring no intervention. However, a few patients, especially those with a history of oral aspirin and coagulation dysfunction, develop massive bleeding. We propose that massive rectal bleeding should be indicated based on the following scenarios: (1) More than 600 mL of bleeding through the anus 24 h after the puncture; (2) decrease in hemo
In addition to systemic treatment, the commonly used local treatment methods for massive rectal bleeding include transrectal compression of the prostate, rectal tamponade hemostasis, local injection of hemostatic drugs through the rectal endoscope, suture hemostasis, and compression hemostasis in the anal canal with Vaseline gauze wrapped around the drainage tube[8-11]. However, these measures are often somewhat ineffective or traumatic, risking further aggravation, or are difficult to perform or not feasible. The puncture site is in the wide ampulla of the rectum; therefore, the compression position and pressure of the rectal tampon cannot be accurately controlled, even with a small amount of venous bleeding. Consequently, the pressure required to stop the bleeding cannot be achieved, nor can a reliable hemostasis effect, which allows the bleeding to continue. During treatment with colonoscopy or anoscopy, massive blood accumulation or arterial jet bleeding in the rectum blurs the field of view. Furthermore, electrocoagulation and drug injection under colonoscopy are not easy to perform, and sewing and clamping the bleeding point is challenging because the anus is narrow. Moreover, if the patient has already entered hemorrhagic shock, they may not be able to tolerate anesthesia, major trauma, or surgical treatment; forcing these may cause a greater operational risk. Therefore, a more minimally invasive or non-invasive, rapid, and effective treatment scheme is urgently needed.
Massive rectal bleeding after transrectal prostate puncture is a severe complication, and the key to recovery is its timely diagnosis and treatment. The incidence of rectal bleeding should be 100% because each needle path is a bleeding point; however, the amount of bleeding differs. We observed 30 patients with prostate electrotomy through the anus at the end of transrectal prostate puncture and confirmed that all had bleeding to varying degrees. A large amount of bleeding in a short period, which can lead to unstable blood pressure circulation, or bleeding that exceeds 20% of the circulating blood volume, can easily cause shock or life-threatening situations and must be handled quickly and effectively. From 2017 to 2022, we used the SIMAI transanal prostate resection instrument for rectal examinations and treatment, which imitates the prostate resection and bladder tumor resection technology, to treat patients with massive bleeding with good results.
Our technique has significant technical advantages compared to other surgical treatment methods, such as traditional colonoscopy injection or electrocoagulation hemostasis. First, it is a simple operation similar to that for the transurethral resection of bladder tumors; the only difference is that it is transanal. Therefore, it should be quick and easy for doctors to master. Second, the field of view is clear. The electric resectoscope has a high definition and good directivity, and the arteries can be clearly seen in cases of jet hemorrhage. If blood and blood clots accumulate, they can be quickly removed by suction or flushing to ensure a clear field of view. Third, achieving hemostasis is reliable since the prostate electrocoagulation electrode can coagulate and close 23 mm diameter blood vessels, which immediately controls the bleeding. Fourth, the operation time is short, taking approximately 10 min. Furthermore, medications can be injected through the lens sheath, and the internal rectal drainage tube can be accurately retained. Fifth, the technique is safe owing to its minimally invasive nature, and most patients, especially those who are critically ill, do not require anesthesia. Even if it is unsuccessful, the patient will not be harmed, and open surgery can be performed at any time. Sixth, urologists are familiar with electrosurgical equipment. Therefore, neither do the patients need to be transferred to the endoscopy center, nor do the urologists require assistance from other doctors to stop the bleeding. Hemostasis can be achieved in the urological department. Finally, the technology and equipment specialized for urology can be used flexibly. For instance, prostate electrotomy equipment can be used for prostate and rectal bleeding, allowing for multi-disciplinary treatments.
Moreover, our team has explored the safety of this surgical technique since 2003, finding no serious complications. However, in our experience, the following should be avoided during the operation: (1) Intestinal perforation: Cutting too deep can lead to rectal perforation, especially when the peritoneum is above the reflex level, potentially leading to diffuse peritonitis; (2) water poisoning: If the pressure of the flushing liquid is too high and the operation time is too long, excessive amount of liquid is absorbed, and the patient can experience water poisoning; and (3) serious infection: The space around the rectum is loose. If the flushing pressure is too high and the operation time is too long, cellulitis, perirectal abscess, or systemic infection may occur. Therefore, it is necessary to retain an anal tube after the operation to fully drain the flushing fluid and accumulated blood to assist in rectal decompression.
Treating massive rectal bleeding after transrectal prostate puncture with a transanal prostate resection instrument is simple, safe, and effective. The operation technology is similar to that of a transurethral bladder tumor resection, except that the transurethral technology is used transanally. The equipment and technical conditions are available in grassroots hospitals in developing countries, such as those in areas of China. Therefore, we encourage the popularization and application of this technique as the preferred method at such hospitals.
We thank the patients for their contribution to this report.
| 1. | Goldberg H, Ahmad AE, Chandrasekar T, Klotz L, Emberton M, Haider MA, Taneja SS, Arora K, Fleshner N, Finelli A, Perlis N, Tyson MD, Klaassen Z, Wallis CJD. Comparison of Magnetic Resonance Imaging and Transrectal Ultrasound Informed Prostate Biopsy for Prostate Cancer Diagnosis in Biopsy Naïve Men: A Systematic Review and Meta-Analysis. J Urol. 2020;203:1085-1093. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 46] [Article Influence: 9.2] [Reference Citation Analysis (0)] |
| 2. | Lu CH, Lin TP, Shen SH, Huang YH, Chung HJ, Kuo JY, Huang WJS, Wu HHH, Chang YH, Lin ATL, Chen KK. Clinical efficacy of transrectal ultrasound-guided prostate biopsy in men younger than 50 years old with an elevated prostate-specific antigen concentration (>4.0 ng/mL). J Chin Med Assoc. 2017;80:413-418. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 3. | Loeb S, Vellekoop A, Ahmed HU, Catto J, Emberton M, Nam R, Rosario DJ, Scattoni V, Lotan Y. Systematic review of complications of prostate biopsy. Eur Urol. 2013;64:876-892. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 594] [Cited by in RCA: 732] [Article Influence: 61.0] [Reference Citation Analysis (0)] |
| 4. | Omer A, Lamb AD. Optimizing prostate biopsy techniques. Curr Opin Urol. 2019;29:578-586. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 22] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 5. | Borghesi M, Ahmed H, Nam R, Schaeffer E, Schiavina R, Taneja S, Weidner W, Loeb S. Complications After Systematic, Random, and Image-guided Prostate Biopsy. Eur Urol. 2017;71:353-365. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 241] [Cited by in RCA: 339] [Article Influence: 37.7] [Reference Citation Analysis (0)] |
| 6. | Malik A, Ishtiaq R, Goraya MHN, Inayat F, Gaduputi VV. Endoscopic Therapy in the Management of Patients With Severe Rectal Bleeding Following Transrectal Ultrasound-Guided Prostate Biopsy: A Case-Based Systematic Review. J Investig Med High Impact Case Rep. 2021;9:23247096211013206. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 7. | Ghani KR, Dundas D, Patel U. Bleeding after transrectal ultrasonography-guided prostate biopsy: a study of 7-day morbidity after a six-, eight- and 12-core biopsy protocol. BJU Int. 2004;94:1014-1020. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 87] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 8. | Braun KP, May M, Helke C, Hoschke B, Ernst H. Endoscopic therapy of a massive rectal bleeding after prostate biopsy. Int Urol Nephrol. 2007;39:1125-1129. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 13] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 9. | de Arriba Alonso M, Vaquero Ayala L, Alonso Prieto MÁ, Linares Torres P. [Complications of the biopsy of prostate transrectal ecoguide: about a case]. Gastroenterol Hepatol. 2013;36:607-608. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 10. | Gonen M, Resim S. Simplified treatment of massive rectal bleeding following prostate needle biopsy. Int J Urol. 2004;11:570-572. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 14] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 11. | Katsinelos P, Kountouras J, Dimitriadis G, Chatzimavroudis G, Zavos C, Pilpilidis I, Paroutoglou G, Germanidis G, Mimidis K. Endoclipping treatment of life-threatening rectal bleeding after prostate biopsy. World J Gastroenterol. 2009;15:1130-1133. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 18] [Cited by in RCA: 16] [Article Influence: 1.0] [Reference Citation Analysis (0)] |