Published online Jun 26, 2024. doi: 10.12998/wjcc.v12.i18.3417
Revised: April 25, 2024
Accepted: May 10, 2024
Published online: June 26, 2024
Processing time: 100 Days and 22.2 Hours
The emergency department (ED) plays a critical role in establishing artificial airways and implementing mechanical ventilation. Managing airbags in the ED presents a prime opportunity to mitigate the risk of ventilator-associated pneu
To investigate the current status of ED nurses' knowledge, beliefs, and practical behaviors in airway airbag management and their influencing factors.
A survey was conducted from July 10th to August 10th, 2023, using convenience sampling on 520 ED nurses from 15 tertiary hospitals and 5 sary hospitals in Shanghai. Pathway analysis was utilized to analyze the influencing factors.
The scores for ED nurses' airway airbag management knowledge were 60.26 ± 23.00, belief was 88.65 ± 13.36, and behavior was 75.10 ± 19.84. The main influencing factors of airbag management knowledge included participation in specialized nurse or mechanical ventilation training, department, and work experience in the department. Influencing factors of airbag management belief comprised knowledge, department, and participation in specialized nurse or mechanical ventilation training. Primary influencing factors of airbag management behavior included knowledge, belief, department, participation in specialized nurse or mechanical ventilation training, and professional title. The belief in airbag management among ED nurses acted as a partial mediator between knowledge and behavior, with a total effect value of 0.513, and an indirect effect of 0.085, constituting 16.6% of the total effect.
ED nurses exhibit a positive attitude toward airbag management with relatively standardized practices, yet there remains room for improvement in their knowledge levels. Nursing managers should implement interventions tailored to the characteristics of ED nurses' airbag management knowledge, beliefs, and practices to enhance their airbag management proficiency.
Core Tip: The emergency department (ED) serves as a critical setting for establishing artificial airways and implementing mechanical ventilation. Managing airbags in the ED presents a prime opportunity to mitigate the risk of ventilator-associated pneumonia. Research findings reveal that ED nurses generally harbor a positive attitude toward airbag management, and their practical behaviors are moderately standardized. Nevertheless, there remains a need for enhancing their knowledge levels. This study offers theoretical underpinning for delivering pertinent training and fostering the development of specialized nursing programs tailored to ED settings. Furthermore, it underscores the necessity for implementing targeted improvement strategies.
- Citation: Wei XH, Zhou LJ, Li R, Li XY, Zhang Y, Zhang HY, Wang SM, Zhang J. Current state and influencing factors in airbag management among emergency department nurses: A multicenter study. World J Clin Cases 2024; 12(18): 3417-3427
- URL: https://www.wjgnet.com/2307-8960/full/v12/i18/3417.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i18.3417
As medical technology advances, establishing an artificial airway for mechanical ventilation has become a crucial intervention for critically ill patients. Ventilator-associated pneumonia (VAP), as one of the common complications of mechanical ventilation, stands as a significant contributor to patient mortality. Statistics reveal that approximately 28% of mechanically ventilated patients experience VAP, with mortality rates ranging between 25% and 50%[1,2]. Furthermore, the occurrence of VAP prolongs hospital stays and escalates medical expenses[3]. Within mechanical ventilation, the role of the airbag is paramount. Situated on the outer wall at the end of the tracheal tube or tracheostomy tube, the airbag ensures effective positive pressure ventilation and prevents aspiration of oral and gastric contents when appropriately pressurized[4]. Insufficient airbag pressure could lead to a gap between the airway and airbag, compromising ventilation efficacy and allowing upper respiratory pathogens to enter the lower airways[5]. Conversely, overinflation of the airbag may result in ischemic mucosal damage or even necrosis of the airway[6]. Recent studies both domestically and internationally have confirmed that maintaining airbag pressure within an optimal range significantly reduces the incidence of VAP in patients[7-9]. The probability of patients developing VAP reaches 34.6% without standardized airbag monitoring and management[10]. Therefore, implementing effective airbag management for critically ill patients holds paramount importance in reducing the incidence of VAP, shortening hospital stays, and expediting patient recovery.
Emergency department (ED) is critical in treating severely ill patients, where mechanical ventilation is an essential intervention. Research indicates[11] that the utilization rate of mechanical ventilation in ED has increased to 27%. Consequently, implementing airbag management strategies in ED offers a significant opportunity to reduce the risk of VAP infections[12]. Previous studies have predominantly concentrated on intensive care unit (ICU) nurses' under
A total of 520 ED nurses from 15 tertiary hospitals and 5 sary hospitals in Shanghai were recruited for the study con
General questionnaire: The researchers designed the questionnaire for this section after reviewing previous studies and consulting with experts. It encompassed various demographic and professional aspects, including gender, grade of working hospital, education status, professional title, department: Emergency resuscitation room or EICU, work experience in the department, and participation in specialized nurse or mechanical ventilation training.
The ICU healthcare workers' artificial airway airbag management KAP questionnaire: The questionnaire was originally designed in 2020[15], comprising three dimensions: Knowledge, attitude/belief, and behavior, totaling 42 multiple-choice questions. In this investigation, the Cronbach's alpha coefficients for the questionnaire were calculated as 0.983, 0.926, and 0.956, corresponding to the dimensions of knowledge, attitude/belief, and behavior, respectively. Specifically, the questionnaire addressed knowledge inquiry, encompassing 19 items graded on a scale from 1 (no understanding) to 5 (complete mastery), with a total score ranging from 19 to 95. A higher score reflects a superior comprehension of airbag management and its associated knowledge. The attitude inquiry comprised 8 items graded from 1 (disagree) to 3 (completely agree), with a total score ranging from 8 to 24. A higher score indicates a more favorable attitude and belief toward airbag management. The behavior inquiry involved 15 items rated from 1 (never) to 5 (always), with a total score ranging from 15 to 75. A higher score indicates a higher level of execution of airbag management in clinical practice. The total score of the questionnaire was 194 points, categorized into three levels based on different total scores: Total score < 116 points categorized as poor, 116 ≤ total score < 155 points categorized as fair, and total score ≥ 155 points categorized as good. For ease of comparison of knowledge, belief, and behavior scores, standardized scores were calculated for each dimension and the total score using the formula: Standardized score = (actual score on the questionnaire/total score on questionnaire) X 100[16].
The study utilized the questionnaire star platform for conducting online surveys. Initially, researchers sought consent from nurse supervisors in each hospital's ED to participate in the study. Subsequently, nurse supervisors distributed the questionnaire link to WeChat groups of various ED units, enabling ED nurses to independently and anonymously complete the survey. The open online survey period lasted from July 10 to August 10, 2023, allowing each account to complete the questionnaire only once. Following data collection, a two-person check was conducted to ensure comp
This study utilized SPSS 26.0 to perform statistical analyses. Quantitative data adhering to a normal distribution were described using the mean ± SD, and evaluated through univariate analyses employing independent sample t-tests and analysis of variance. Qualitative data were summarized by frequencies (percentages). Additionally, Pearson correlation analysis was conducted to examine relationships between variables. For a more in-depth analysis, variables that showed statistical significance in the univariate analysis were selected as independent variables for path analysis using Mplus 8.3. P < 0.05 was considered to indicate statistical significance.
In this survey, a total of 520 questionnaires were distributed, out of which 487 were considered valid, leading to an effective response rate of 93.7%. Table 1 provides comprehensive details on the general information about the survey participants.
| Characteristics variables | Frequency | Characteristics variables | Frequency |
| Sex | Professional title | ||
| Male | 53 (10.9) | Nurse | 99 (20.3) |
| Female | 434 (89.1) | Nurse practitioner | 271 (55.6) |
| Grade of a working hospital | Chief nurse practitioner | 112 (23.0) | |
| Grade 3, Class A | 256 (52.6) | Deputy chief nurse practitioner | 5 (1.0) |
| Grade 3, Class B | 134 (27.5) | Work experience in the department | |
| Grade 2, Class A | 97 (19.9) | 1 yr-3 yr | 107 (22.0) |
| Educational status | 4 yr-6 yr | 88 (18.1) | |
| Specialized secondary school | 5 (1.0) | 7 yr-10 yr | 91 (18.7) |
| Junior college | 124 (25.5) | 11 yr-15 yr | 111 (22.8) |
| Bachelor's degree | 354 (72.7) | 16 yr-20 yr | 59 (12.1) |
| Master's degree and above | 4 (0.8) | More than 21 yr | 31 (6.4) |
| Department (of work) | Participation in specialized nurse or mechanical ventilation training | ||
| Emergency resuscitation room | 256 (52.6) | ||
| Emergency intensive care unit | 231 (47.4) | Yes | 300 (61.6) |
| No | 187 (38.4) |
The study revealed that ED nurses exhibited varied levels of competence in airbag management. Their knowledge score was 57.24 ± 21.85 points, indicating a wide range of proficiency. Approximately 47.4% of the participants demonstrated good to fair levels of knowledge in this domain. Regarding their beliefs, the score was 21.28 ± 3.21 points. Impressively, 99.4% of the nurses held beliefs falling within the good to fair range. In terms of behavior, the score stood at 56.33 ± 14.88 points, suggesting moderate consistency. Notably, 80.4% of the nurses displayed good to fair behavior in managing airbags. Table 2 provides detailed distributions of standardized scores and levels across dimensions.
| Project | Score (points, mean ± SD) | Standardized score (points, mean ± SD ) | Grade (frequency): Poor, Fair, Good | ||
| Knowledge | 57.24 ± 21.85 | 60.26 ± 23.00 | 256 (52.6) | 100 (20.5) | 131 (26.9) |
| Belief | 21.28 ± 3.21 | 88.65 ± 13.36 | 3 (0.6) | 118 (24.2) | 366 (75.2) |
| Practice | 56.33 ± 14.88 | 75.10 ± 19.84 | 94 (19.3) | 162 (33.3) | 231 (47.4) |
In the domain of ED nurses' competence in airbag management, the three areas scoring the lowest in knowledge include item 5, "Understanding venous pressure on the airway wall" (2.49 ± 1.40); item 4, "Understanding arterial pressure on the airway wall" (2.54 ± 1.41); and item 7, "Understanding factors that increase airbag pressure" (2.83 ± 1.27). Similarly, the lowest scores in beliefs about airbag management are item 8, "Agreement with the regular assessment of airbag pressure monitoring" (2.52 ± 0.56); item 2, "Proactive learning about artificial airway airbag management" (2.58 ± 0.52); and item 3, "Participation in airbag-related training" (2.61 ± 0.50). In practices, the lowest scores are item 8, "Flushing fluid accumulation from the airbag during airway management" (3.08 ± 1.52); item 2, "Measuring airbag pressure before and after oral care and nasogastric feeding" (3.40 ± 1.33); and item 15, "Using an airbag leak test to assess upper airway patency before extubation" (3.44 ± 1.40). Please refer to Table 3 for detailed information.
| Project | Score (points, mean ± SD) |
| The three entries with the lowest knowledge scores | |
| Item 5 "Understanding venous pressure on the airway wall" | 2.49 ± 1.40 |
| Item 4 "Understanding arterial pressure on the airway wall" | 2.54 ± 1.41 |
| Item 7 "Understanding factors that increase airbag pressure" | 2.83 ± 1.27 |
| The three entries with the lowest belief scores | |
| Item 8 "Agreement with the regular assessment of airbag pressure monitoring" | 2.52 ± 0.56 |
| Item 2 "Proactive learning about artificial airway airbags management" | 2.58 ± 0.52 |
| Item 3 "Participation in airbag-related training" | 2.61 ± 0.50 |
| The three items with the lowest practical scores | |
| Item 8 "Flushing fluid accumulation from the airbag during airway management" | 3.08 ± 1.52 |
| Item 2 "Measuring airbag pressure before and after oral care and nasogastric feeding" | 3.40 ± 1.33 |
| Item 15 "Using an airbag leak test to assess upper airway patency before extubation" | 3.44 ± 1.40 |
Statistically significant differences were observed in airbag management knowledge scores among nurses based on their educational level, department of work, work experience in the department, and participation in specialized nurse or mechanical ventilation training (P < 0.05). Variations in belief scores were noted based on the department of work and participation in specialized nurse or mechanical ventilation training (P < 0.05). Similarly, differences in behavior scores were significant concerning educational level, professional title, department of work, and participation in specialized nurse or mechanical ventilation training in the ED (P < 0.05). Please refer to Table 4 for detailed information. Positive correlations were found between ED nurses' knowledge and belief, knowledge and behavior, and belief and behavior regarding airbag management (r = 0.452, 0.582, 0.463 respectively; P < 0.01).
| Project | Knowledge score | Test statistic | P value | Belief score | Test statistic | P value | Practical score | Test statistic | P value |
| Sex | -0.2912 | 0.772 | -1.2982 | 0.195 | 0.4592 | 0.647 | |||
| Male | 56.32 ± 24.75 | 20.74 ± 3.38 | 57.32 ± 16.92 | ||||||
| Female | 57.35 ± 21.50 | 21.34 ± 3.18 | 56.21 ± 14.63 | ||||||
| Grade of a working hospital | 2.7841 | 0.063 | 2.4881 | 0.084 | 1.8201 | 0.163 | |||
| Grade 3, Class A | 55.55 ± 21.79 | 21.00 ± 3.25 | 55.96 ± 15.04 | ||||||
| Grade 3, Class B | 57.25 ± 20.43 | 21.42 ± 3.14 | 55.22 ± 15.03 | ||||||
| Grade 2, Class A | 61.68 ± 23.46 | 21.81 ± 3.13 | 58.82 ± 14.11 | ||||||
| Educational status | 2.6711 | 0.047 | 1.3661 | 0.253 | 3.1881 | 0.024 | |||
| Specialized secondary school | 53.40 ± 24.74 | 22.80 ± 1.79 | 61.40 ± 17.56 | ||||||
| Junior college | 60.80 ± 21.98 | 21.24 ± 3.32 | 59.38 ± 13.71 | ||||||
| Bachelor's degree | 55.84 ± 21.67 | 21.23 ± 3.19 | 55.09 ± 15.14 | ||||||
| Master's degree and above | 76.25 ± 14.38 | 24.00 ± 0.00 | 64.50 ± 9.68 | ||||||
| Professional title | 1.6071 | 0.187 | 2.3001 | 0.077 | 3.4081 | 0.018 | |||
| Nurse | 55.80 ± 21.77 | 21.47 ± 3.22 | 60.14 ± 13.65 | ||||||
| Nurse practitioner | 56.15 ± 21.90 | 20.96 ± 3.25 | 54.68 ± 15.54 | ||||||
| Chief nurse Practitioner | 60.79 ± 21.72 | 21.83 ± 3.03 | 56.99 ± 13.89 | ||||||
| Deputy chief nurse practitioner | 65.60 ± 19.50 | 22.20 ± 3.03 | 55.00 ± 11.34 | ||||||
| Department | -4.4882 | < 0.001 | -4.5182 | < 0.001 | -6.9092 | < 0.001 | |||
| Emergency resuscitation room | 53.10 ± 21.17 | 20.67 ± 3.36 | 52.14 ± 15.56 | ||||||
| Emergency intensive care unit | 61.83 ± 21.73 | 21.95 ± 2.90 | 60.97 ± 12.59 | ||||||
| Work experience in the department | 2.3291 | 0.042 | 1.4751 | 0.196 | 2.0041 | 0.077 | |||
| 1 yr-3 yr | 55.31 ± 23.00 | 21.29 ± 3.32 | 58.48 ± 14.88 | ||||||
| 4 yr-6 yr | 54.73 ± 21.45 | 20.61 ± 3.40 | 55.24 ± 15.09 | ||||||
| 7 yr-10 yr | 54.34 ± 21.81 | 21.22 ± 3.06 | 52.57 ± 16.15 | ||||||
| 11 yr-15 yr | 58.38 ± 21.16 | 21.32 ± 3.09 | 57.05 ± 13.80 | ||||||
| 16 yr-20 yr | 62.95 ± 19.49 | 21.81 ± 3.20 | 58.41 ± 13.01 | ||||||
| More than 21 yr | 64.65 ± 23.35 | 22.06 ± 2.94 | 56.45 ± 13.50 | ||||||
| Participation in specialized nurse or mechanical ventilation training | 9.6352 | < 0.001 | 5.7992 | < 0.001 | 7.9382 | < 0.001 | |||
| Yes | 63.87 ± 21.69 | 21.94 ± 2.95 | 60.31 ± 13.53 | ||||||
| No | 46.61 ± 17.51 | 20.21 ± 3.33 | 49.94 ± 14.76 |
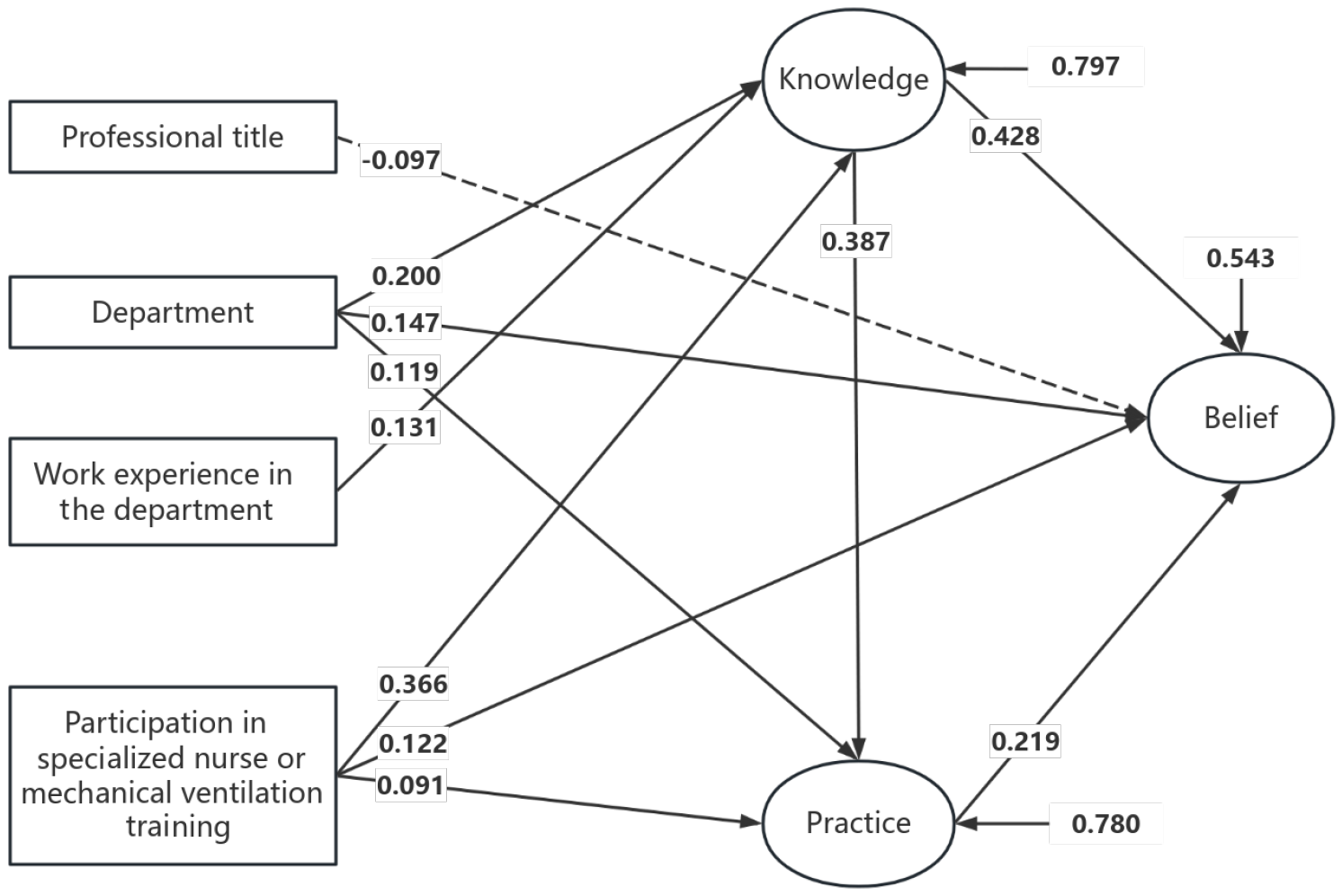
Utilizing the KAP theory, we conducted path analysis, as illustrated in Figure 1, considering variables with statistically significant effects from single-factor analysis as independent variables, and knowledge, attitude, and behavior scores as dependent variables. Table 5 presents the model fit parameters, with values indicating a good fit. In Table 6, we highlight that out of 13 research hypotheses, our study supported 10, did not support 2, and found a negative effect in 1 hypothesis. Specifically, the department of work, work experience, and participation in specialized nurse or mechanical ventilation training directly influenced the knowledge score of ED nurses regarding airbag management. Additionally, knowledge, department of work, participation in specialized nurse or mechanical ventilation training, and professional title directly influenced the belief score. Furthermore, knowledge, belief, department of work, participation in specialized nurse or mechanical ventilation training, and professional title had direct effects on the behavior score of ED nurses. Notably, belief acted as a partial mediator between knowledge and behavior. The total effect was 0.513, with an indirect effect of 0.085, constituting 16.6% of the total effect (refer to Table 7).
| Fit indices | χ2 | DF | χ2/DF | Root mean square error of approximation | Comparative fit index | Tucker-Lewis index | Standardized residual mean root |
| Fitted values | 3291.278 | 1003 | 3.281 | 0.068 | 0.907 | 0.901 | 0.047 |
| Reference value | — | — | 1-5 | < 0.08 | > 0.90 | > 0.90 | < 0.05 |
| Hypothesis | Relationship between variables | Estimate | Standard error | T value | P value | Decision |
| H1 | Knowledge: Belief | 0.387 | 0.044 | 8.764 | < 0.01 | Accepted |
| H2 | Knowledge: Practice | 0.428 | 0.040 | 10.587 | < 0.01 | Accepted |
| H3 | Belief: Practice | 0.219 | 0.041 | 5.338 | < 0.01 | Accepted |
| H4 | Educational status: Knowledge | -0.038 | 0.042 | -0.884 | 0.376 | Rejected |
| H5 | Department: Knowledge | 0.200 | 0.041 | 4.911 | < 0.01 | Accepted |
| H6 | Work experience in the department: Knowledge | 0.131 | 0.042 | 3.104 | < 0.01 | Accepted |
| H7 | Participation in specialized nurse or mechanical ventilation training: Knowledge | 0.366 | 0.039 | 9.472 | < 0.01 | Accepted |
| H8 | Department: Belief | 0.119 | 0.043 | 2.781 | < 0.01 | Accepted |
| H9 | Participation in specialized nurse or mechanical ventilation training: Belief | 0.091 | 0.046 | 1.999 | < 0.05 | Accepted |
| H10 | Educational status: Practice | -0.024 | 0.039 | -0.609 | 0.543 | Rejected |
| H11 | Professional title: Practice | -0.097 | 0.039 | -2.482 | < 0.05 | Significant negative correlation |
| H12 | Department: Practice | 0.147 | 0.037 | 4.015 | < 0.01 | Accepted |
| H13 | Participation in specialized nurse or mechanical ventilation training: Practice | 0.122 | 0.038 | 3.208 | < 0.01 | Accepted |
| Dependent variable | Independent variable | Direct effect | Overall effect ranking |
| Knowledge | Participation in specialized nurse or mechanical ventilation training | 0.366 | 1 |
| Department | 0.200 | 2 | |
| Work experience in the department | 0.131 | 3 | |
| Belief | Knowledge | 0.387 | 1 |
| Department | 0.119 | 2 | |
| Participation in specialized nurse or mechanical ventilation training | 0.091 | 3 | |
| Practice | Knowledge | 0.428 | 1 |
| Belief | 0.219 | 2 | |
| Department | 0.147 | 3 | |
| Participation in specialized nurse or mechanical ventilation training | 0.122 | 4 | |
| Professional title | -0.97 | 5 |
According to the KAP theory, knowledge serves as the foundation for behavioral change. In the realm of airbag management for critically ill patients, mastering this knowledge is crucial. Within the clinical practice of ED nurses, frequent procedures involving endotracheal intubation and mechanical ventilation are imperative. A deficiency in relevant knowledge may result in improper procedures, subsequently escalating the incidence of VAP. This study unveiled that the knowledge level of ED nurses in airbag management mostly ranged from good to fair, with 47.4% of respondents categorized as having fair to good levels, consistent with previous studies[13,17]. However, attention is warranted regarding poorly performing items within the knowledge score, particularly in comprehending factors such as venous pressure, arterial pressure, and increased airbag pressure. This inadequacy might be linked to limited opportunities for ED nurses to partake in relevant training. Hence, structured theoretical courses and practical guidance could assist in enhancing nurses' knowledge of airbag management[18,19]. Furthermore, studies by Higgs et al[20] demonstrated that adherence to evidence-based guidelines in airbag management can significantly mitigate complications. Therefore, future training programs could tailor training based on evidence-based guidelines, targeting the identified weaknesses in ED nurses' knowledge.
Regarding airbag management beliefs, ED nurses showcased relatively positive attitudes, with 99.4% classified in the fair to good range, consistent with prior research[21]. Nevertheless, attention should be directed towards certain belief items with lower scores, including regular assessment of airbag pressure monitoring, active engagement in learning-related knowledge, and participation in relevant training. This might be influenced by the demanding nature of ED nursing work and the pressure of assessments, reducing their willingness to actively engage in learning and training. Hence, administrators could enhance nurses' training enthusiasm by optimizing training formats and improving training management systems.
In terms of airbag management behavior, 80.4% of ED nurses exhibited good to fair levels, contrary to findings in a previous study[22]. This difference might be attributed to the growing emphasis on nursing care practices in airbag management, with departments establishing nursing quality control units for supervision. However, specific attention should be given to certain behaviors with lower scores, such as flushing fluid accumulation from the airbag during airway management, measuring airbag pressure before and after oral care and nasogastric feeding, and using an airbag leak test to assess upper airway patency before extubation. Past research indicates that bedside skills training through plan-do-check-act methodologies can significantly enhance nurses' bedside skills in standardized airbag management, consequently reducing VAP incidence[23]. Therefore, we propose using quality management approaches to improve the standardization of nurses' airbag management. Additionally, considering the adoption of new instruments and technologies, such as dynamic airbag pressure monitoring systems or portable electronic airbag pressure monitoring devices[24-26], could further enhance airbag management practices.
The results of path analysis highlighted the positive direct impact of specialized nurse or mechanical ventilation training on the airbag management knowledge scores of ED nurses, aligning with previous research[27]. Consequently, it is advisable to strengthen education and training concerning airbag management in clinical settings, by establishing quality control groups for artificial airway airbag management. This measure aims to ensure the timely dissemination of research advancements and cutting-edge knowledge in this field[28]. Furthermore, a noticeable discrepancy in airbag management knowledge was observed between nurses in the EICU and those in the emergency resuscitation room, possibly indicating a lack of emphasis on airbag management in the latter. Many hospitals have yet to implement standardized airbag management measures in emergency resuscitation rooms. Therefore, we propose active knowledge exchange between departments to enhance the airbag management knowledge level of all nurses in the hospital. Lastly, our research findings suggest that years of work experience significantly impact nurses' airbag management knowledge scores, consistent with prior studies[13]. Nurses with more experience generally possess richer clinical experience and a higher level of airbag management knowledge. Hence, administrators should prioritize and provide additional training opportunities for nurses with less experience to improve their airbag management knowledge levels.
Path analysis results revealed that the knowledge of airbag management among ED nurses significantly impacts their belief scores, consistent with previous findings[15]. This discovery likely demonstrates how the extensive knowledge of nurses in airbag management positively influences their beliefs in this domain. Additionally, nurses stationed in emergency resuscitation units and those lacking specialized training in nursing or mechanical ventilation tended to hold relatively pessimistic views regarding airbag management. This tendency could arise from a deficiency in emphasis on airway management within emergency resuscitation units and a lack of specialized training, potentially resulting in a lower level of proficiency in airbag management knowledge. Therefore, it is recommended to prioritize interventions targeting nurses with lower levels of airbag management knowledge, particularly those deployed in emergency resuscitation units and those lacking specialized training. The goal is to augment their awareness and commitment to actively participate in airbag management practices.
The path analysis results underscored the significant and direct impact of airbag management knowledge on behavior. Moreover, both airbag management knowledge and beliefs directly shaped airbag management behavior, with airbag management beliefs serving as a mediator between knowledge and behavior, aligning with previous research[15]. This suggests that enhanced knowledge and positive beliefs regarding airbag management can promote stricter adherence to practices among nurses. Research conducted by Hu et al[29] further validates the efficacy of educational interventions in cultivating positive beliefs among nurses, offering a viable approach to enhancing airbag management behavior. However, nurses working in emergency resuscitation units and those lacking specialized training in nursing or mechanical ventilation exhibited comparatively inferior airbag management behavior. Previous studies[12,30,31] have also revealed elevated airbag pressures in mechanically ventilated patients within ED and pre-hospital settings, indicating a need for improvement in airbag management practices, particularly in critical care scenarios. This highlights the importance for management to prioritize quality control in ED airbag management to bolster nurses' adherence to proper practices. Additionally, the path analysis revealed a negative correlation between airbag management behavior and nurses holding higher professional titles. This phenomenon may be attributed to fewer airbag management-related tasks being performed by nurses with higher professional titles, often delegated to lower-ranking colleagues. Consequently, management must enhance training and assessment protocols for nurses in emergency resuscitation units, those lacking specialized training, and those with higher professional titles, thereby providing adequate support and fostering improvement in airbag management behavior.
The study highlights a positive attitude and relatively standardized practices among ED nurses regarding airbag management. However, there is room for improvement in their knowledge levels. To enhance nurses' knowledge of airbag management for mechanically ventilated patients and reduce the incidence of VAP, managers can develop scientifically feasible training strategies based on the knowledge, beliefs, and practice characteristics of ED nurses and influencing factors. Improvements to specialized training systems can be implemented to enhance nurses' adherence to airbag management measures.
There are some advantages of our study. Firstly, the innovative approach of shifting the research focus from the ICU to the ED for airbag management studies presents a novel perspective. Secondly, conducting a multicenter, large-sample survey in Shanghai, China, ensures a comprehensive and diverse dataset, yielding insightful observations. Thirdly, the inclusion of in-depth analyses, such as pathway analysis and effect decomposition, enhances the overall understanding of the subject.
We also acknowledged some limitations of this study. First, The cross-sectional design of the study poses challenges in establishing causal relationships between variables. Additionally, the exclusive reliance on data from ED nurses in Shanghai, China, may constrain the generalizability of the findings. To enhance the universal applicability of research outcomes, future endeavors should consider broadening the study scope to include samples from diverse regions and healthcare institutions. Despite these limitations, the study provides a robust foundation for future research aiming to refine and broaden the understanding of airbag management practices among ED nurses.
| 1. | Chastre J, Fagon JY. Ventilator-associated pneumonia. Am J Respir Crit Care Med. 2002;165:867-903. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1831] [Cited by in RCA: 1734] [Article Influence: 75.4] [Reference Citation Analysis (0)] |
| 2. | Oliveira J, Zagalo C, Cavaco-Silva P. Prevention of ventilator-associated pneumonia. Rev Port Pneumol. 2014;20:152-161. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 31] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 3. | Spalding MC, Cripps MW, Minshall CT. Ventilator-Associated Pneumonia: New Definitions. Crit Care Clin. 2017;33:277-292. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 48] [Cited by in RCA: 75] [Article Influence: 9.4] [Reference Citation Analysis (0)] |
| 4. | Wu YS, Su GX, Yin YL, Wei SY, Gao P. Research progress of artificial airway balloon technology and pressure monitoring technology. Chin Nurs Res. 2018;32:18-21. [DOI] [Full Text] |
| 5. | Lizy C, Swinnen W, Labeau S, Poelaert J, Vogelaers D, Vandewoude K, Dulhunty J, Blot S. Cuff pressure of endotracheal tubes after changes in body position in critically ill patients treated with mechanical ventilation. Am J Crit Care. 2014;23:e1-e8. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 68] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 6. | Efrati S, Deutsch I, Gurman GM, Noff M, Conti G. Tracheal pressure and endotracheal tube obstruction can be detected by continuous cuff pressure monitoring: in vitro pilot study. Intensive Care Med. 2010;36:984-990. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 7. | Lau AC, So HM, Tang SL, Yeung A, Lam SM, Yan WW; Hong Kong East Cluster Task Force on Prevention of Ventilator-associated Pneumonia in Critical Care Areas. Prevention of ventilator-associated pneumonia. Hong Kong Med J. 2015;21:61-68. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 9] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 8. | Lorente L, Blot S, Rello J. New issues and controversies in the prevention of ventilator-associated pneumonia. Am J Respir Crit Care Med. 2010;182:870-876. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 86] [Cited by in RCA: 71] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 9. | Yao Y, Liu YC, Yu MM, Zhu PY, Chen Q. Effect of continuous artificial airway balloon pressure control on the incidence of ventilator-associated pneumonia. Chin J of Mod Nurs. 2017;23:1734-1738. [DOI] [Full Text] |
| 10. | Zhang RY. Evaluation of the application effect of artificial airway balloon manometry in patients with mechanical ventilation. China Practical Med. 2015;10:270-271. [DOI] [Full Text] |
| 11. | Li YL, Jia RX, Li Y, Song T. Analysis of Clinical Risks and Maintenance Strategies for Ventilator Use. Hospital Administration Forum. 2023;40:90-92. [DOI] [Full Text] |
| 12. | Grap MJ, Munro CL, Unoki T, Hamilton VA, Ward KR. Ventilator-associated pneumonia: the potential critical role of emergency medicine in prevention. J Emerg Med. 2012;42:353-362. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 20] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 13. | Zhang C, Zhang Y, Li SY, Wang CH, Liu JY, Zhang YH. A multi-center investigation on ICU nurses' cognition, attitude and behavior towards airbag management. International J of Nurs Science. 2020;39:1189-1193. [DOI] [Full Text] |
| 14. | Yang Y, Yang J, Li HJ, Liu HY, Li LJ, Cai MM, Yun RR, Guo SH, Gong QL. Preparation and evaluation of a questionnaire on the knowledge, credit and practice of artificial airway airbag management in intensive care ward. Journal of Lanzhou University (Med Edition). 2019;45:91-96. [DOI] [Full Text] |
| 15. | Zhang C. Development and application of knowledge, attitude and behavior questionnaire on artificial airway balloon management for ICU medical staff. Chengde Med College. 2020;. [DOI] [Full Text] |
| 16. | Cui PR, Zhou YX, Zhang MX, Zhao F, Yuan L, Xiao LF, Xing QL, Wang Q, Mo YZ. Investigation and research of the gap between clinical practice and guidelines of nurse knowledge, attitude and practice on insulin injection. Chin J of Nurs. 2023;58:1178-1185. [DOI] [Full Text] |
| 17. | Xiang YJ, Sai DH. Investigation and analysis of nurses' knowledge of tracheal intubation balloon management. Chin J of Mod Nurs. 2010;16:2512-2515. [DOI] [Full Text] |
| 18. | Mpasa F, van Rooyen DRM, Venter D, Jordan P, Ten Ham-Baloyi W. Improving nurses' knowledge of managing endotracheal tube cuff pressure in intensive care units: A quasi-experimental study. Health SA. 2020;25:1479. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 19. | Murugiah UR, Ramoo V, Jamaluddin MFH, Yahya A, Baharudin AA, Abu H, Thinagaran RRR. Knowledge acquisition and retention among nurses after an educational intervention on endotracheal cuff pressure. Nurs Crit Care. 2021;26:363-371. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 6] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 20. | Higgs A, McGrath BA, Goddard C, Rangasami J, Suntharalingam G, Gale R, Cook TM; Difficult Airway Society; Intensive Care Society; Faculty of Intensive Care Medicine; Royal College of Anaesthetists. Guidelines for the management of tracheal intubation in critically ill adults. Br J Anaesth. 2018;120:323-352. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 392] [Cited by in RCA: 509] [Article Influence: 63.6] [Reference Citation Analysis (0)] |
| 21. | Wei Z, Wu JM, Ye WC, Guo YF, Guo AM. Investigation on the status quo of airway management and evidence-based practice attitude of ICU nurses. Chin Nurs Manag. 2015;15:563-566. [DOI] [Full Text] |
| 22. | Zhang RL. Analysis of ICU nurses' knowledge, belief, and behavior about patients' early activities and their influencing factors. China J of Practical Nurs. 2019;35:897-900. [DOI] [Full Text] |
| 23. | Zhang S, Nie Q, Zheng J, Lv SS, Cheng YY. Using PDCA to improve the monitoring and management level of artificial airway balloon pressure in ICU nurses. Med and Health. 2022;57-60. |
| 24. | Li JF, Wang ZM, Zhao LL, Yin J. Application of self-made dynamic balloon pressure monitoring system combined with continuous low negative pressure suction in artificial airway management of mechanically ventilated patients. Chin J of Mod Nurs. 2012;1714-1716. [DOI] [Full Text] |
| 25. | Wang S, Li W, Li W, Song D, Chen D, Duan J, Li C, Li G. [A design and study of a novel electronic device for cuff-pressure monitoring]. Zhonghua Wei Zhong Bing Ji Jiu Yi Xue. 2017;29:551-555. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 26. | Lu YC, Jiang DH, Su CY, Zhang Y. Development and application of continuous monitoring controller for artificial airway balloon pressure in intensive care unit. Chin J of Mod Nurs. 2012;4069-4071. [DOI] [Full Text] |
| 27. | Min FF, Zeng XL. Status quo of RlCU nurses' cognition and behavior on artificial airway airbag management and analysis of related factors. Nurs Pract and Res. 2020;17:38-40. [DOI] [Full Text] |
| 28. | Shu Y, Bi MM, Zhang C, Gong YY, Li ZX, Zhou TT, Li XR, Liu XY, Xie WG. Summary of the best evidence of artificial airway balloon management in ICU patients. Chin J of Nurs. 2022;57:3038-3045. [DOI] [Full Text] |
| 29. | Hu WC, Liu G, Yuan QD, Quan JQ. Effect of video playback of trauma weekly meeting on knowledge, attitude, and practice of emergency nurses in trauma care. Nurs Pract and Res. 2022;19:150-153. [DOI] [Full Text] |
| 30. | Galinski M, Tréoux V, Garrigue B, Lapostolle F, Borron SW, Adnet F. Intracuff pressures of endotracheal tubes in the management of airway emergencies: the need for pressure monitoring. Ann Emerg Med. 2006;47:545-547. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 59] [Article Influence: 3.0] [Reference Citation Analysis (1)] |
| 31. | Svenson JE, Lindsay MB, O'Connor JE. Endotracheal intracuff pressures in the ED and prehospital setting: is there a problem? Am J Emerg Med. 2007;25:53-56. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 41] [Article Influence: 2.3] [Reference Citation Analysis (0)] |