Published online Jun 26, 2024. doi: 10.12998/wjcc.v12.i18.3410
Revised: April 6, 2024
Accepted: May 10, 2024
Published online: June 26, 2024
Processing time: 134 Days and 16.8 Hours
The coronavirus disease 2019 (COVID-19) pandemic has significantly impacted health, mental well-being, and societal functioning, particularly for individuals with psychiatric conditions and substance use disorders. Recent evidence highlights a concerning increase in alcohol consumption during the pandemic, with a study spanning 2015-2020 indicating heightened usage, especially among young and middle-aged adults, for relaxation and tension relief. Additionally, addressing challenges exacerbated by the pandemic, another study underscored persistent barriers to healthcare access, resulting in increased alcohol and tobacco use rates and limited healthcare options. These findings shed light on the unique vulnerabilities exposed by the pandemic, emphasizing the need to investigate further its impact on alcohol consumption in diverse non-urban American communities.
To investigate the impact of the COVID-19 pandemic on alcohol abuse using socioeconomic and medical parameters in diverse non-urban community in America.
Based on a cross-sectional analysis of 416 participants the United States in 2021, the study utilized The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition criteria to categorize alcohol consumption levels. Participants aged 21 years and above were surveyed through an online platform due to COVID-19 challenges. The survey was conducted from January 14 to January 31, 2022, recruiting participants via social media and ensuring anonymity. Informed consent was secured, emphasizing the voluntary nature of participation, and participants could only take the survey once.
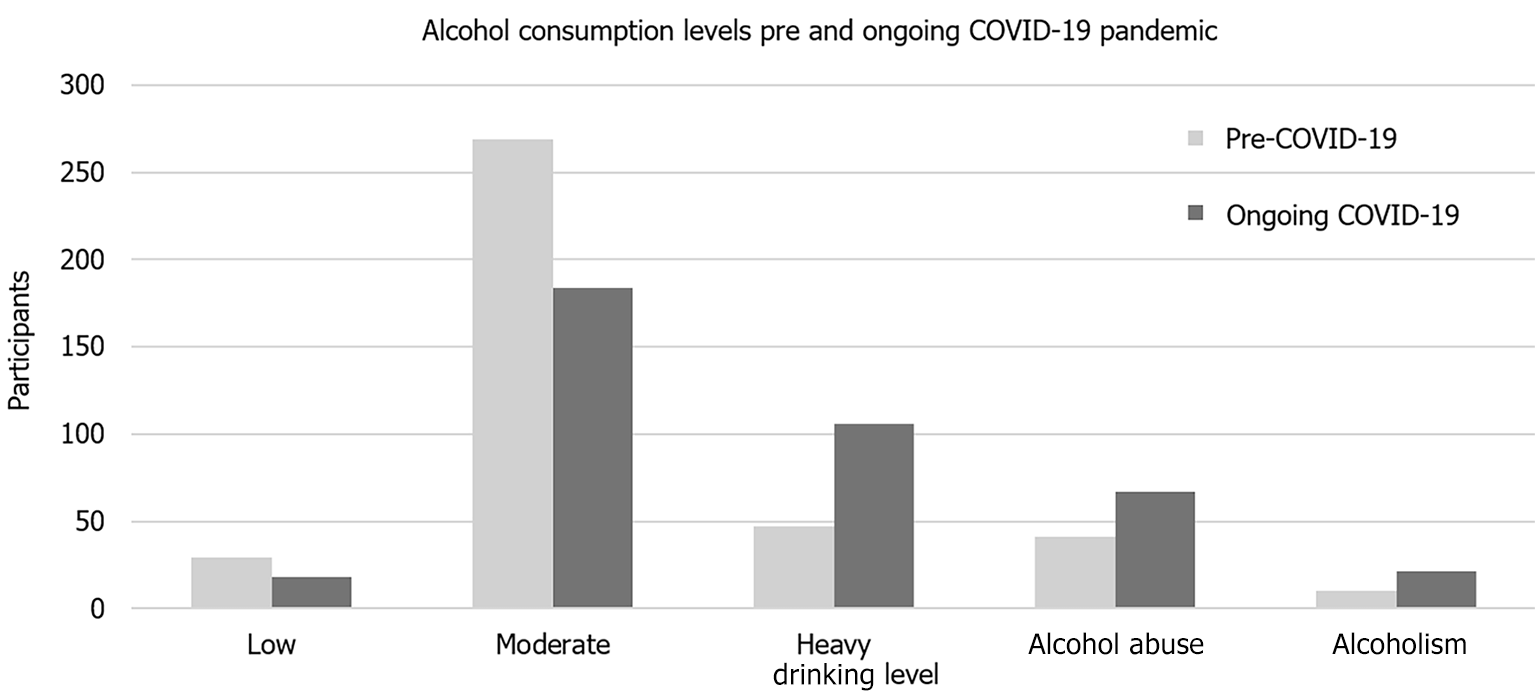
Out of 416 survey respondents, 396 met eligibility criteria, with 62.9% reporting increased alcohol consumption during COVID-19. Males (68.8%) and ages 21-29 years (34.6%) predominated. Low alcohol consumption decreased by 2.8% (P = 0.237), moderate by 21.4% (P < 0.001), and heavy increased by 14.9% (P < 0.001). Alcohol abuse rose by 6.5% (P = 0.0439), with a 7% increase in self-identified alcohol abusers/alcoholics. Seeking treatment during COVID-19 rose by 6.9%. Easier alcohol access (76.0%) was reported, while 80.7% found it harder to access medical care for alcohol-related issues. These findings highlight the pandemic's impact on alcohol consumption and healthcare access, emphasizing the need for targeted interventions during public health crises.
The COVID-19 pandemic exacerbated alcoholism and abuse, with increased heavy consumption (P < 0.001) and abuse (P = 0.0439). Access to medical programs for addressing alcohol abuse declined, highlighting the need for targeted intervention.
Core Tip: The coronavirus disease 2019 (COVID-19) pandemic intensifies alcohol-related challenges in diverse non-urban American communities, impacting health and well-being. A cross-sectional study of 416 participants in 2021 reveals a 62.9% surge in alcohol consumption during the pandemic. Predominantly male (68.8%) and aged 21-29 (34.6%), the cross-section sees decreased low and moderate alcohol consumption but a notable rise in heavy drinking. Alcohol abuse increases by 6.5%, with a 7% surge in those identifying as alcohol abusers/alcoholics. Seeking therapeutic treatment rises by 6.9%. COVID-19 facilitates easier alcohol access (76.0%) but hampers medical care for alcohol-related issues (80.7%). The study underscores the pandemic's profound impact on alcoholism and access to care in non-urban settings.
- Citation: Rathore R, Rangrej SB, Carvalho V. Increased alcohol consumption during the COVID-19 pandemic: A cross-sectional study. World J Clin Cases 2024; 12(18): 3410-3416
- URL: https://www.wjgnet.com/2307-8960/full/v12/i18/3410.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i18.3410
The coronavirus disease 2019 (COVID-19) pandemic is a catastrophic event that impacts individual and collective health, emotional well-being, and social functioning. Pandemics, such as COVID-19, can lead to various medical, psychological like anxiety and depression and sociological problems, and these challenges may be particularly pronounced in individuals with psychiatric conditions and those engaging in excessive substance use[1,2]. Emerging evidence suggests an increase in alcohol consumption during the COVID-19 pandemic.
A comprehensive study examining U.S. drinking trends prior to and during the COVID-19 pandemic in 2020, which included data from 2015 to 2020, encompassing 16987 young adults (ages 19–30 years) and 23584 middle-aged adults (ages 35–55 years), revealed an increased frequency of alcohol use in both groups. Additionally, both young and middle-aged adults reported increased alcohol use for relaxation, tension relief, and boredom[3].
The United States Census Bureau's urban-rural classification distinguishes between densely developed urban areas and non-urban rural regions. Urban areas comprise densely settled cores with residential, commercial, and other urban land uses delineated based on housing units and population density criteria. Rural areas encompass all territory, population, and housing not included within urban boundaries[4].
Despite assumptions of slower COVID-19 spread in non-metropolitan regions due to more space per person, barriers to healthcare access persist, especially in metropolitan areas. These barriers are often linked to lower incomes, limited economic opportunities, and healthcare access. Non-metropolitan areas also face higher rates of alcohol and tobacco use, alongside fewer healthcare options[5].
While the COVID-19 pandemic impacted all communities, non-urban or underserved communities areas faced unique vulnerabilities. Nonuraban residents reported more positive COVID-19 tests, closer friends or family members hospitalized, increased treatment for anxiety or depression, delays in paying rent, mortgages, and bills, greater difficulty affording groceries and other necessities, and an increased reliance on loans from family or friends compared to urban residents[6]. A recent study on COVID-19 and its impact on underserved communities highlighted challenges in these area mentioned factors, such as existing health disparities among underserved communities, lack of resources for people of color, lack of belief in available resources, social isolation, and economic burden, limited access to treatment, regulatory barriers in telehealth, and stress from the on-going COVID-19 pandemic have been identified as some of the key factors behind the acute health effects of people with substance use disorder[7]. Due to the disproportionate inequalities experienced by non-urban residents during the COVID-19 pandemic, this study aims to better understand how the pandemic affected their alcohol consumption.
Analysis of a representative cross-sectional general non-urban United States population in 2021 included 416 participants, measuring socio-demographics, alcohol use history, access to alcohol products, and access to medical care related to alcohol abuse. The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition criteria were employed to categorize the levels of alcohol consumption, and bivariate and multivariate analyses were conducted to examine factors associated with alcohol abuse during the COVID-19 pandemic.
This study utilized a cross-sectional design to survey a convenience sample of United States adults aged 21 years and above residing in non-urban communities, defined according to the United States Census Bureau, 2020. Participants were recruited through a convenience sampling technique, and an online survey was administered via Survey Monkey®. Due to the challenges posed by the COVID-19 pandemic, a community-based national sampling survey was not feasible. Therefore, data collection took place online, aligning with social distancing and lockdown protocols. The survey was conducted from January 14 to January 31, 2022, a period during which the pandemic was still active in the United States. Participants aged 18 years and above, with internet access and the ability to read, were eligible to participate, and their consent was obtained. Survey settings were restricted to ensure each participant could only take the survey once, allowing for free editing of answers until submission. Identifiers were not collected to maintain response anonymity.
Study participants were recruited through crowdsourcing on various social media platforms (Facebook, Twitter, and Instagram), WhatsApp groups, or email. The survey commenced with an introduction to the study team, objectives, and the estimated time required to complete the questionnaire. Informed consent was obtained, assuring participants of response confidentiality and emphasizing the voluntary nature of their participation. Only participants who provided affirmative consent proceeded to the survey.
In this survey involving 416 respondents, 396 were eligible for the study after applying exclusion criteria based on responses. Of these, 249 (62.9%) reported increased alcohol consumption during the COVID-19 pandemic compared to pre-pandemic levels. The sample characteristics, detailed in Table 1, indicate that 286 (68.8%) were male, 115 (27.6%) were female, and 15 (3.6%) identified as other genders. The age distribution revealed 34.6% in the 21-29 years age range, 30.1% in the 30-39 years range, 27.3% in the 40-49 years range, and 9.3% above 50 years old.
| Participant results | |
| Do you live in a non-urban United States of America? | |
| Yes | 396 (95.2) |
| No | 20 (4.8) |
| What is your gender? | |
| Male | 286 (68.8) |
| Female | 130 (31.2) |
| What is age demographic? | |
| 21-29 | 137 (34.6) |
| 30-39 | 119 (30.1) |
| 40-49 | 108 (27.3) |
| Over 50 | 37 (9.3) |
| What was your drinking level (pre-COVID-19) in methodology you have to mention how on what basis you divided low, moderate, heavy? | |
| Low | 29 (7.3) |
| Moderate | 269 (67.9) |
| Heavy | 47 (11.9) |
| Alcohol abuse | 41 (10.4) |
| Alcoholism | 10 (2.5) |
| What was your drinking level (during the ongoing COVID-19 pandemic)? | |
| Low | 18 (4.5) |
| Moderate | 184 (46.5) |
| Heavy | 106 (26.8) |
| Alcohol abuse | 67 (16.9) |
| Alcoholism | 21 (5.3) |
| For those that chose alcohol abuse or alcoholism did you seek medical or therapeutic treatment (pre-COVID)? | |
| Yes | 33 (64.7) |
| No | 17 (33.3) |
| For those that chose alcohol abuse or alcoholism did you seek medical or therapeutic treatment (during the ongoing COVID-19 pandemic)? | |
| Yes | 63 (71.6) |
| No | 25 (28.4) |
| Did your alcohol consumption increase during the COVID-19 pandemic compared to before the COVID-19 pandemic? | |
| Yes | 157 (62.9) |
| No | 92 (37.1) |
| Was it easier or harder to obtain access to alcohol during the COVID-19 pandemic compared to before the COVID-19 pandemic? | |
| Easier | 301 (76) |
| Harder | 95 (24) |
| Was it easier or harder to obtain access to medical or therapeutic programs relating to alcohol abuse and alcoholism during the COVID-19 pandemic compared to before the COVID-19 pandemic? | |
| Easier | 17 (19.3) |
| Harder | 71 (80.7) |
The results indicate that males were the predominant gender in responding to this survey at 68.8%, with the age range of 21-29 years at 34.6% in the cross-section. This can be observed in Figures 1 and 2, respectively. Most of the participants were 21-29 years old (34.6%), followed by 30-39 years old (30.1%) and 40-49 years old (27.3%), with less than 10% of participants being over 50 years old-precisely 9.3%.
Low alcohol consumption levels decreased by 2.8% (P = 0.237) during the COVID-19 pandemic compared to pre-COVID-19. Moderate alcohol consumption levels decreased by 21.4% (P < 0.001) during the COVID-19 pandemic compared to pre-COVID-19. Heavy alcohol levels increased by 14.9% (P < 0.001). Alcohol abuse consumption levels increased by 6.5% (P = 0.0439) during COVID-19 compared to pre-COVID-19. Alcoholic consumption levels increased by 2.8% (P = 0.877), as illustrated in Figure 1.
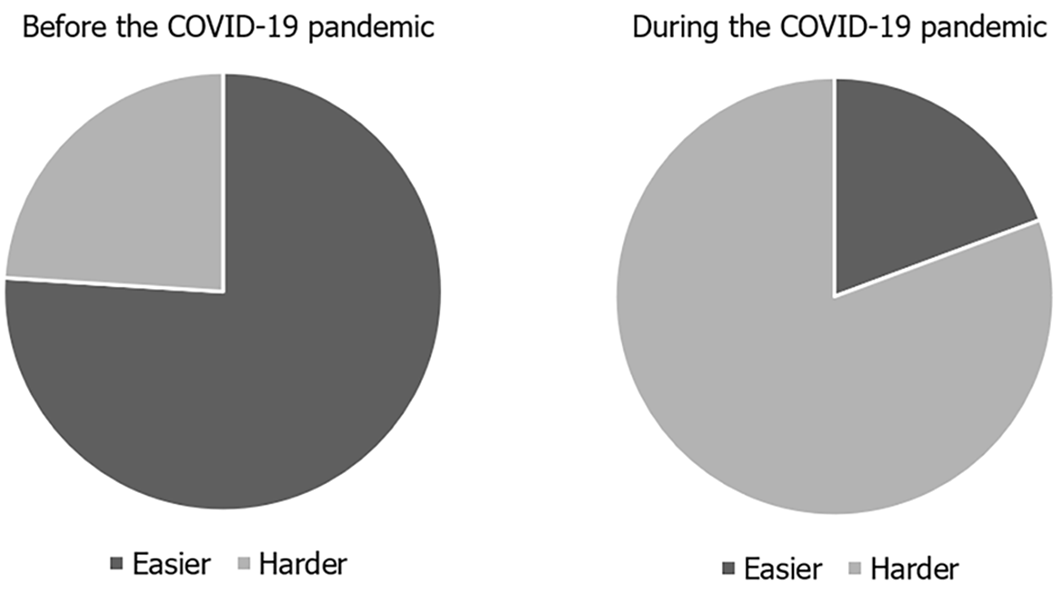
Out of the 396 participants, 249 (62.9%) reported that their alcohol consumption increased during the COVID-19 pandemic compared to pre-COVID-19. The cross-section was compared to pre-COVID-19 and during COVID-19 alcohol consumption characteristics using one-way ANOVA statistical analysis. When comparing the 62.9% increase in alcohol consumption to alcohol consumption levels, we obtained a P value of < 0.001. The number of people describing their relationship with alcohol as alcohol abuse or alcoholism pre-COVID was 50, compared to 68 participants during the ongoing COVID-19 pandemic. Therefore, there was a 7% increase in participants identifying as having alcohol abuse or alcoholism during the ongoing COVID-19 pandemic compared to pre-COVID. Those characterized in the alcohol abuse and alcoholic category for consumption were asked if therapeutic or medical treatment was sought pre-COVID-19 and during the COVID-19 pandemic. 64.7% said yes during the pre-COVID-19 timeframe, and 71.6% said yes during COVID-19. This represented a 6.9% increase during COVID-19 compared to pre-COVID-19. 76.0% of participants said it was easier to obtain alcohol during the COVID-19 pandemic compared to pre-COVID-19 levels.
In addition, 80.7% of participants reported that it was harder to obtain medical or therapeutic care for alcohol-related chief complaints during COVID-19 compared to pre-COVID-19.
The demographics of the cross-section were predominantly male (68.8%) with an age range of 21-29 years (34.6%). These results were correlated with the finding that a total of 23.8% of respondents were both male and between the ages of 21-29 years. A t-test was performed to demonstrate that these demographic results were significant (P = 0.0487) in relation to the cross-section. This might be attributed to the survey reaching fewer women or fewer women responding to the survey. It is necessary to acknowledge that the accidental nature of this survey could restrict its ability to accurately represent non-urban areas across the United States.
Heavy alcohol consumption levels increased by 14.9% during the COVID-19 pandemic compared to pre-COVID-19 levels (P < 0.001). The level of alcohol consumption at the level of alcohol abuse increased by 6.5% during COVID-19 compared to pre-COVID-19 (P = 0.0439). Alcoholic consumption levels increased by 2.8% during the COVID-19 pandemic compared to pre-COVID-19 levels (P = 0.877). Alcohol consumption, particularly in non-urban parts of the United States, increased during the COVID-19 pandemic. When comparing drinking levels pre-COVID-19 and during the ongoing COVID-19 pandemic, there was only a 2.8% decrease in the number of participants who reported consuming a low amount of alcohol during the ongoing pandemic (P = 0.0237).
While analyzing the results for the moderate alcohol consumption level, there was also a decrease in the number of participants who reported consuming a moderate level of alcohol. During the Pre-COVID-19 period, 269 participants reported consuming a moderate level of alcohol, and during the ongoing COVID-19 pandemic, this number was reduced to 184 participants (P < 0.001). Other studies ultimately found that the pandemic and lockdown were associated with increased alcohol use[8]. At every stratified level, people were more likely to consume a higher quantity of alcohol during this specific period. Over the course of the pandemic, residents of the United States received several influxes of cash in the form of stimulus checks because they had to stay home and not work. We did not consider how an increase in funds could have influenced alcohol consumption because people use cash in a variety of ways. We also did not consider the impact that being with family consistently might lead to an increase in alcohol consumption, as demonstrated in the month of December when the highest amount of alcohol consumption took place during holidays spent with family. Perhaps being around family and friends all the time had an impact on alcohol consumption as well.
Out of the 396 participants, 249 (62.9%) said that their alcohol consumption increased during the COVID-19 pandemic when compared to pre-COVID-19 (P < 0.001). A cross-sectional survey of United States adults on alcohol consumption during the COVID-19 Pandemic reported a 60% increase in drinking habits, with 34.1% reporting binge drinking and 7.0% reporting extreme binge drinking. Participants who experienced COVID-19-related stress consumed more drinks (P = 0.040) and a greater number of days drinking (P = 0.007). Furthermore, participants reported that the reasons for increased drinking included increased stress (45.7%), increased alcohol availability (34.4%), and boredom (30.1%)[9]. A quantitative survey focused on COVID-19 findings demonstrate how COVID-19 disruptions at the structural and community level affected outcomes related to mental health and drug use at the individual level[10]. A cross-sectional sample of social media users in the U.S. examined if age modified the association of anxiety and depression symptomatology and alcohol use during the COVID-19 pandemic. The survey had 5850 respondents, out of which, 29% reported increased alcohol use. This study also found that a much greater proportion of older people (40–60 years) reported increased drinking if they also had symptoms of anxiety and depression, compared to those without symptoms[11]. This study shows effects of COVID-19 pandemic on mental health and the impact it has on alcohol consumption. A scoping review study underscores how the unequal distribution of pain burden among marginalized communities exacerbates pre-existing disparities, ultimately leading to detrimental psychological and physical health consequences during COVID-19. Service disruptions resulting from social distancing mandates and infrastructural constraints hindered patients' access to necessary care, exacerbating their suffering and worsening health outcomes. The compounding effects of pain disparities and healthcare disruptions highlight the urgent need for targeted interventions to address these issues within vulnerable populations[12].
There are some limitations that should be considered when interpreting this study’s data. Firstly, the survey was a convenience sample recruited through social media. Therefore, we were not able to make contact with all potential participants, which possibly explains why a little over 90% of respondents were under 50 years old. In addition, the relatively small sample size might impact the results, as it only represents a small section of the population. The recruitment method might be flawed, as the sample was mostly male and does not necessarily reflect the non-urban population. This may lead to differences in alcohol consumption. This study did not consider underage drinking, which is a factor that could be explored in further studies. Other factors such as race, class, gender, and disability were also not considered. The reasons for increased alcohol consumption were not explored in the survey. General access and COVID-19-related access to health care could also have been addressed and compared to the ease of obtaining access to medical or therapeutic programs related to Alcohol abuse and Alcoholism during the COVID-19 Pandemic compared to before the COVID-19 Pandemic.
The unprecedented impact of COVID-19 on alcohol consumption in non-urban American communities has resulted in elevated levels of alcoholism and alcohol abuse. The survey unveiled a significant surge in heavy alcohol consumption (P < 0.001) and alcohol abuse (P = 0.0439) during the pandemic, as evidenced by cross-sectional findings. Access to medical or therapeutic programs for alcohol abuse and alcoholism became notably scarcer during the COVID-19 crisis, while access to alcohol itself substantially increased. This shift translated to heightened opportunities for drinking amid the pandemic, juxtaposed with a decline in access to healthcare programs addressing alcohol abuse.
| 1. | Pfefferbaum B, North CS. Mental Health and the Covid-19 Pandemic. N Engl J Med. 2020;383:510-512. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2488] [Cited by in RCA: 2408] [Article Influence: 481.6] [Reference Citation Analysis (0)] |
| 2. | Kupcova I, Danisovic L, Klein M, Harsanyi S. Effects of the COVID-19 pandemic on mental health, anxiety, and depression. BMC Psychol. 2023;11:108. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 61] [Reference Citation Analysis (0)] |
| 3. | Patrick ME, Terry-McElrath YM, Miech RA, Keyes KM, Jager J, Schulenberg JE. Alcohol use and the COVID-19 pandemic: Historical trends in drinking, contexts, and reasons for use among U.S. adults. Soc Sci Med. 2022;301:114887. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 37] [Cited by in RCA: 45] [Article Influence: 15.0] [Reference Citation Analysis (0)] |
| 4. | United States Census Bureau. Urban and Rural. [accessed 2023 Apr 17]. Available from: https://www.census.gov/programs-surveys/geography/guidance/geo-areas/urban-rural.html. |
| 5. | Jenkins WD, Bolinski R, Bresett J, Van Ham B, Fletcher S, Walters S, Friedman SR, Ezell JM, Pho M, Schneider J, Ouellet L. COVID-19 During the Opioid Epidemic - Exacerbation of Stigma and Vulnerabilities. J Rural Health. 2021;37:172-174. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 40] [Cited by in RCA: 75] [Article Influence: 15.0] [Reference Citation Analysis (0)] |
| 6. | Monnat SM. Rural-Urban Variation in COVID-19 Experiences and Impacts among U.S. Working-Age Adults. Ann Am Acad Pol Soc Sci. 2021;698:111-136. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 28] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 7. | Chacon NC, Walia N, Allen A, Sciancalepore A, Tiong J, Quick R, Mada S, Diaz MA, Rodriguez I. Substance use during COVID-19 pandemic: impact on the underserved communities. Discoveries (Craiova). 2021;9:e141. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 37] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 8. | Holland AL, Sharma P, Kurani S, Pazdernik V, Patten C, Kremers HM, Croarkin P, Kamath C, Glasgow A, Sangaralingham L, Geske J, Prasad K, St Sauver J. Longitudinal factors associated with increased alcohol consumption in adults during the COVID-19 pandemic. Am J Drug Alcohol Abuse. 2023;49:481-490. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 9. | Grossman ER, Benjamin-Neelon SE, Sonnenschein S. Alcohol Consumption during the COVID-19 Pandemic: A Cross-Sectional Survey of US Adults. Int J Environ Res Public Health. 2020;17:9189. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 121] [Cited by in RCA: 247] [Article Influence: 49.4] [Reference Citation Analysis (0)] |
| 10. | Walters SM, Bolinski RS, Almirol E, Grundy S, Fletcher S, Schneider J, Friedman SR, Ouellet LJ, Ompad DC, Jenkins W, Pho MT. Structural and community changes during COVID-19 and their effects on overdose precursors among rural people who use drugs: a mixed-methods analysis. Addict Sci Clin Pract. 2022;17:24. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 27] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 11. | Capasso A, Jones AM, Ali SH, Foreman J, Tozan Y, DiClemente RJ. Increased alcohol use during the COVID-19 pandemic: The effect of mental health and age in a cross-sectional sample of social media users in the U.S. Prev Med. 2021;145:106422. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 92] [Cited by in RCA: 122] [Article Influence: 30.5] [Reference Citation Analysis (0)] |
| 12. | Choe K, Zinn E, Lu K, Hoang D, Yang LH. Impact of COVID-19 pandemic on chronic pain and opioid use in marginalized populations: A scoping review. Front Public Health. 2023;11:1046683. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 11] [Article Influence: 5.5] [Reference Citation Analysis (0)] |