Published online Jun 26, 2024. doi: 10.12998/wjcc.v12.i18.3368
Revised: April 22, 2024
Accepted: April 30, 2024
Published online: June 26, 2024
Processing time: 111 Days and 7.4 Hours
With advancements in the diagnosis and treatment of lung diseases, lung segment surgery has become increasingly common. Postoperative rehabilitation is critical for patient recovery, yet challenges such as complications and adverse outcomes persist. Incorporating humanized nursing modes and novel treatments like nitric oxide inhalation may enhance recovery and reduce postoperative complications.
To evaluate the effects of a humanized nursing mode combined with nitric oxide inhalation on the rehabilitation outcomes of patients undergoing lung surgery, focusing on pulmonary function, recovery speed, and overall treatment costs.
A total of 79 patients who underwent lung surgery at a tertiary hospital from March 2021 to December 2021 were divided into a control group (n = 39) receiving a routine nursing program and an experimental group (n = 40) receiving addi
The experimental group demonstrated significant improvements in pulmonary function, reduced average recovery time, and lower total treatment costs compared to the control group. Moreover, the quality of life in the experimental group was significantly better in the 3 months post-surgery, indicating a more effective rehabilitation process.
The combination of humanized nursing mode and nitric oxide inhalation in postoperative care for lung surgery patients significantly enhances pulmonary rehabilitation outcomes, accelerates recovery, and reduces economic burden. This approach offers a promising reference for improving patient care and rehabilitation efficiency following lung surgery.
Core Tip: This study investigates the combined impact of a humanized nursing mode and nitric oxide inhalation on the rehabilitation outcomes following lung surgery. Focusing on enhancing postoperative recovery, the research demonstrates significant improvements in pulmonary function, notably through higher Forced Expiratory Volume in the first second/Forced Vital Capacity values, alongside shorter recovery periods and reduced overall treatment costs for the experimental group. By integrating humanized nursing practices with the therapeutic benefits of nitric oxide, this approach not only presents a novel strategy for improving patient care post-lung surgery but also highlights the potential for reducing the economic burden on patients. The findings advocate for a more personalized, effective rehabilitation process, suggesting a promising avenue for future research in postoperative care and patient rehabilitation strategies.
- Citation: Wang QL, Wang ZB, Zhu JF. Operation room nursing based on humanized nursing mode combined with nitric oxide on rehabilitation effect after lung surgery. World J Clin Cases 2024; 12(18): 3368-3377
- URL: https://www.wjgnet.com/2307-8960/full/v12/i18/3368.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i18.3368
With the increasingly mature inspection technology of lung tumors, infections, fibrosis and other diseases, there are more and more perfect schemes for the treatment of lung diseases, and lung segment surgery has become a common treatment method[1,2]. With the improvement of surgical technology and equipment, lung segment surgery has become more safe and feasible, and different specific surgical methods for patients at the time of surgery can also be more conducive to patients’ postoperative rehabilitation[3,4]. Complications and adverse consequences after lung segment surgery are one of the difficulties in the rehabilitation of lung segment surgery. After lung segment surgery, patients’ lung function will be reduced due to the injury or resection of the surgical area, causing patients to have respiratory dysfunction[5,6]. In the surgical incision area, the severe pain of the sore will affect the patient’s life comfort, and even cause the patient to be unable to live a normal life. Complications such as infection, pneumothorax, and deep vein thrombosis that may occur during lung surgery may prolong the intensive care unit (ICU) stay of patients and increase the difficulty of rehabilitation[7,8]. Nursing in the operating room is an important link in the surgical treatment. During the operation, ensure that the operating environment is clean and sterile, monitor the vital signs of patients, and ensure the physiological stability of patients during the operation; Impart relevant professional knowledge to patients and family members after surgery, monitor the rehabilitation of patients, and formulate corresponding rehabilitation plans. The humanized nursing mode pays more attention to the individual differences and needs of patients, and provides humanized nursing according to the special situation and psychological situation of patients through the concern of patients. More comprehensive and targeted monitoring of patients’ safety and rehabilitation quality during nursing, and timely analysis and solution of problems in the process of rehabilitation can help reduce patients’ pain and discomfort during the postoperative rehabilitation period and reduce the incidence of adverse reactions. Nitric oxide is a potent vasodilator that can relax smooth muscle cells, promote vasodilation, and increase blood flow and oxygen supply. Nitric oxide has anti-inflammatory effect, can inhibit the inflammatory response and the release of inflammatory mediators, can promote tissue repair and regeneration, promote wound healing and tissue reconstruction at a certain concentration, and the use of nitric oxide after lung surgery is conducive to the rehabilitation of patients. Based on this, this study designed a rehabilitation program of operating room nursing combined with nitric oxide based on humanized nursing mode, aiming to improve the rehabilitation effect of patients after lung surgery, and provide effective clinical treatment basis for the rehabilitation after lung surgery[9-13].
A convenience sampling was conducted in a 3A hospital in Nanjing, and selected patients who underwent lung surgery from March 2021 to December 2021 as the research group. When selecting the research target group, the target group needs to be 18 years old; Cardiac function was in the range of grade II to grade III; Brain, kidney, liver and other important organs of the human body need to be free of serious functional disorders; The function of limbs is intact and sound; Good mental state, clear consciousness, able to communicate smoothly, with complete cognitive and behavioral ability; Voluntary participation in the study. When screening the population, the population with acute coronary syndrome, new onset atrial fibrillation or flutter, acute myocarditis or pericarditis, severe hypertrophic obstructive cardiomyopathy, high-grade atrioventricular block and venous thrombosis, and severe chronic obstructive pulmonary disease or respiratory failure should be excluded. In addition, patients with uncontrolled hypertension, resting heart rate greater than or equal to 120 beats per minute or malignant arrhythmia should be excluded. In the study, patients who voluntarily withdrew from the study, worsened their condition, lost to follow-up and insufficient experimental comp
| Project | First round | Second round |
| Problem judgment basis | 0.923 | 0.941 |
| Familiarity with the problem | 0.882 | 0.894 |
| Determine the authority coefficient of experts | 0.902 | 0.918 |
| Kendall’sw | 0.185 | 0.129 |
| χ2 value | 192.180 | 120.840 |
| df | 61.000 | 55.000 |
| P value | 0.000 | 0.000 |
Based on size calculation, sample loss probability in the research process was estimated, and the sample size was expanded by 20%. Finally, the total number of samples was determined to be 79. Thirsty-nine cases constituted the control group and 40 constituted experimental group. Table 2 shows the basic information of patients.
| Data items | Experimental group | Control group | t/χ2 | P value |
| Average age (yr) | 52.60 | 49.28 | 1.0751 | 0.286 |
| Gender (men/women) | 19/21 | 22/17 | 0.6282 | 0.428 |
| BMI average index | 23.65 | 23.03 | 0.7921 | 0.431 |
| Smoking history | 2 | 4 | 0.2093 | 0.648 |
| A history of alcoholism | 1 | 3 | 0.2913 | 0.590 |
| Previous hypertension | 13 | 7 | 2.2112 | 0.137 |
| Previous coronary heart disease | 8 | 4 | 1.4552 | 0.228 |
| Previous diabetes | 6 | 4 | 0.0873 | 0.768 |
| Stroke (Tia) | 4 | 3 | 0.0003 | 0.999 |
| Chronic lung disease | 0 | 0 | 0.000 | 0.999 |
| Atrial fibrillation | 8 | 7 | 0.0542 | 0.816 |
The 42 patients in control group received routine nursing program. First, the disease-related knowledge and respiratory function exercise methods were taught before admission, then the preoperative life precautions were taught, then the postoperative functional rehabilitation and drainage tube nursing guidance were given, and finally the pre-discharge education was given. During the treatment, drug therapy combined with nutritional intervention and exercise rehabilitation were used as rehabilitation means. On the basis of routine nursing program, the experimental group was added with humanized thought, and graded evaluation and humanized intervention were carried out in the process of rehabilitation. The design of humanized nursing mode is composed of outpatient pre rehabilitation, preoperative rehabilitation, postoperative rapid rehabilitation, discharge guidance and return visit after discharge, and three-level rehabilitation strategies are set for preoperative rehabilitation and postoperative rapid rehabilitation. Cardiac function, B-type na
During the recovery period, the proportion of exhaled gas in the first second of the patient’s forced exhalation in the weight of all gases was calculated. The oral pressure data generated by patients’ inspiratory inhalation at maximum speed and strength were collected when blocking the airway at the position of residual volume or functional residual volume. The data of oral pressure produced by patients with maximum speed and force inspiration were collected when blocking the airway at the position of total lung volume. The number of breaths per minute was counted and the lung function was evaluated. The duration of ICU stay and life quality 3 months after operation were statistically analyzed, and the rehabilitation effect was evaluated.
Data were analyzed by Pss25.0 software. Mean plus or minus standard deviation expressed measurement data. The median measured the non-normal distribution data. Mann Whitney test was used. The t test was used to measure the normal distribution data. All theoretical numbers T ≥ 5 and total sample size n ≥ 40 were tested with Pearson chi square. The theoretical number 1 ≤ T < 5, however n ≥ 40, is tested using the chi square of continuity correction. If T < 1 or n < 40, using Fisher’s test. P < 0.05 represents significant difference.
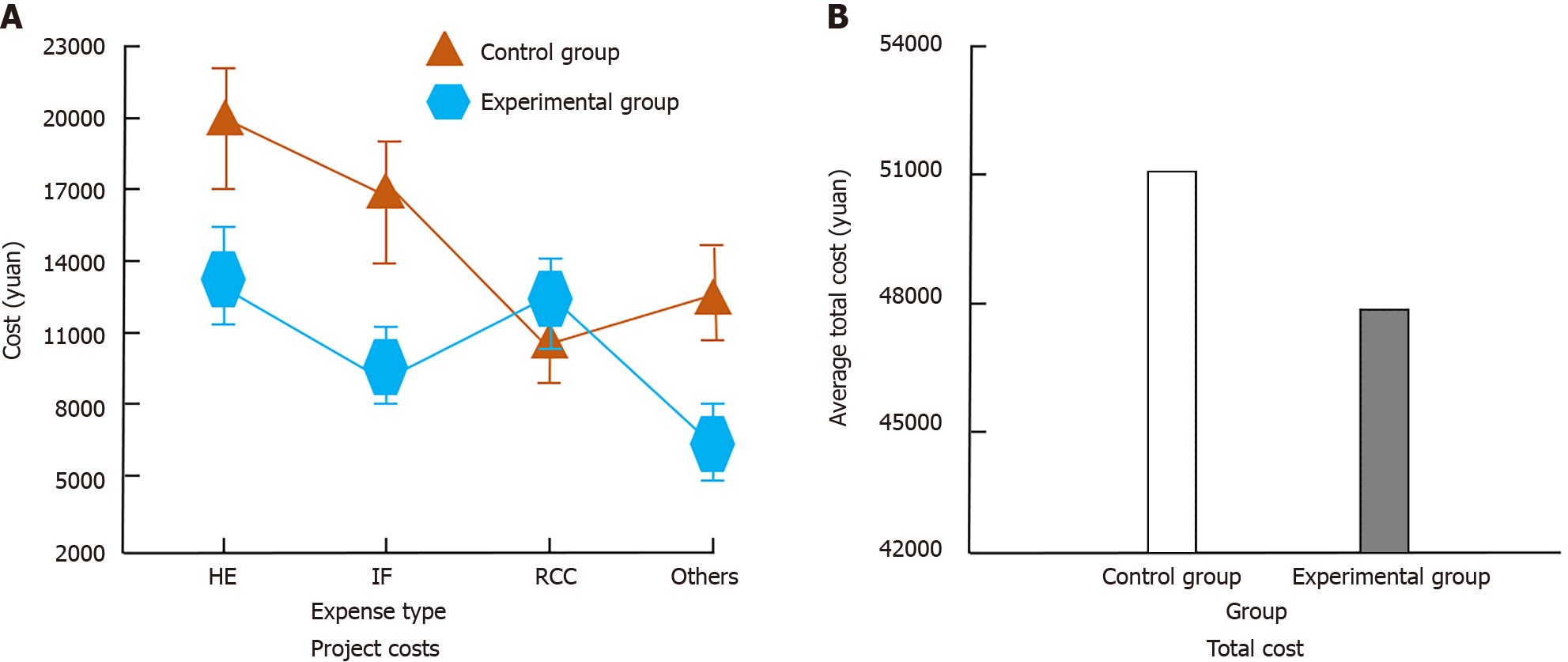
Figure 1 shows the comparison results of hospitalization expenses, examination expenses, rehabilitation nursing expenses and other expenses between the two groups.
In Figure 1, average total cost of control group was about 51089 Yuan, and that of experimental group was about 47743 Yuan. Although the rehabilitation nursing fees of experimental group were higher, other costs were lower. Considering that experimental group had more nursing procedures, it was normal. The total treatment cost in the experimental group was lower, indicating that the research method reduced patients’ treatment cost.
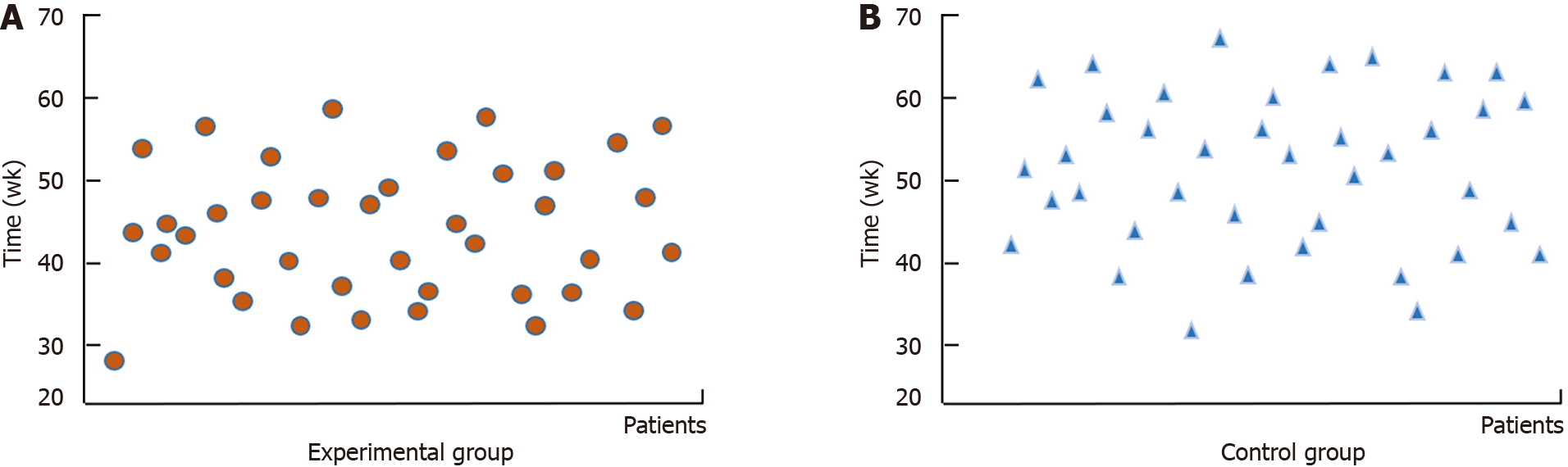
Figure 2 shows the comparison of postoperative complete recovery time between the two groups. In Figure 2, the maximum value of the rehabilitation time interval of the experimental group was less, and the length of the rehabilitation time interval was also less, indicating that the research method can effectively accelerate the rehabilitation speed of patients, and can more accurately control the rehabilitation speed of patients.
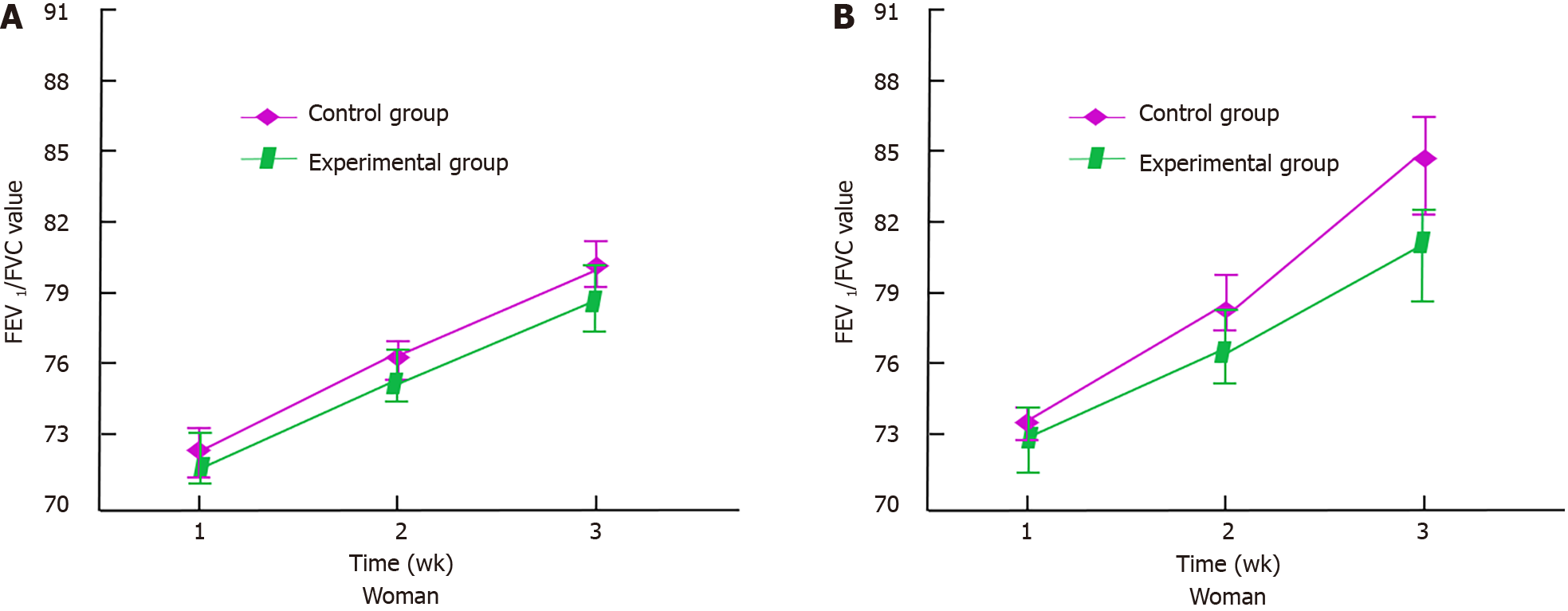
Figure 3 shows the changes of Forced Expiratory Volume in the first second/Forced Vital Capacity (FEV1/FVC) values in the two groups after operation.
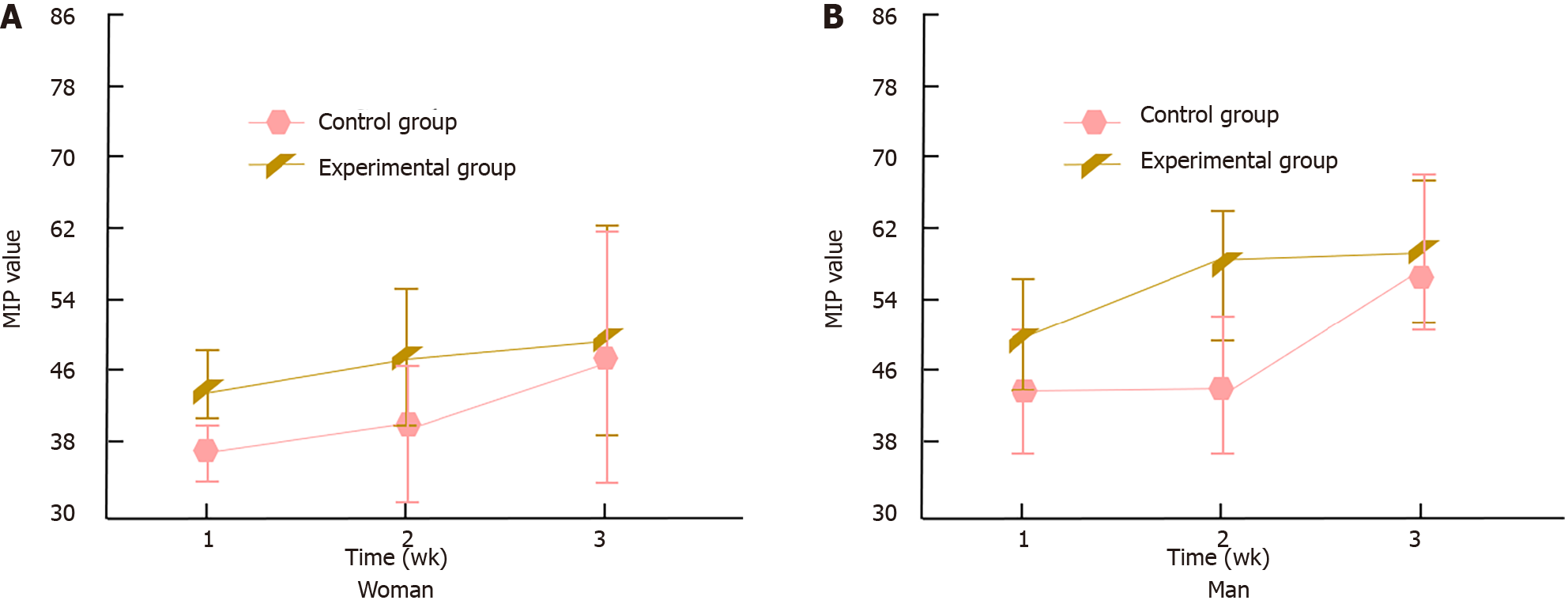
In Figure 3, FEV1/FVC value of patients increased continuously within 3 wk after operation. The FEV1/FVC value in experimental group was higher, indicating that research method can effectively prevent obstructive ventilation dysfunction, and the fluctuation range of FEV1/FVC value of patients in experimental group was smaller, indicating that research method can control the rehabilitation speed of patients more balanced. Figure 4 shows the changes in maximum inspiratory pressure (MIP) after surgery in two groups of patients.
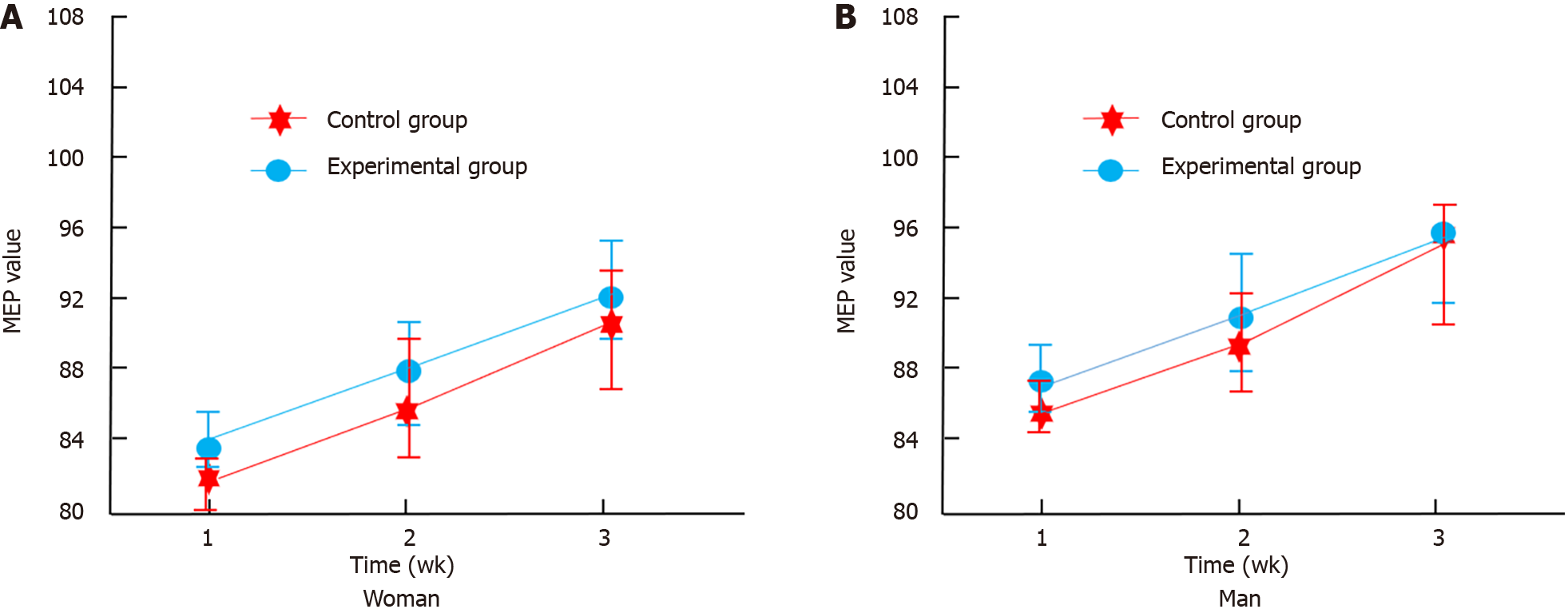
In Figure 4, patients MIP value increased continuously within 3 wk after operation, but the fluctuation range was large. It shows that the research method can effectively maintain the maximum suction pressure of patients after surgery. Figure 5 shows the changes in motor evoked potential (MEP) after surgery in two groups of patients.
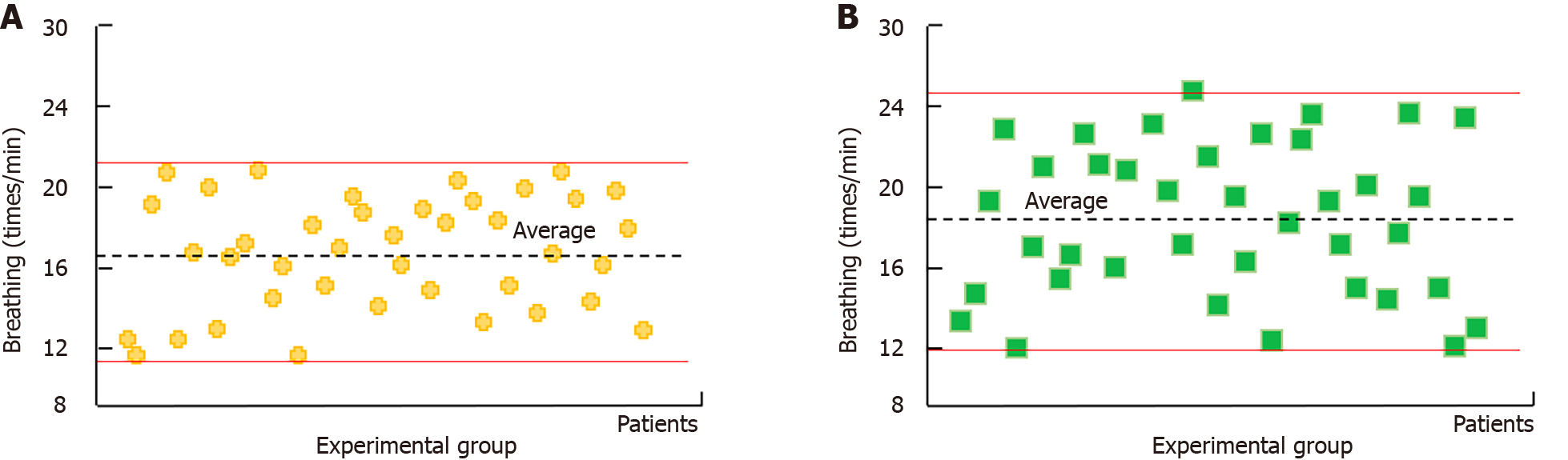
In Figure 5, patients MEP value increased continuously within 3 wk after operation. It shows that the research method can effectively maintain the maximum expiratory pressure of patients after surgery. Figure 6 shows the average number of breaths per minute after surgery.
In Figure 6, average number of breaths per minute in the control group ranged from 12.03 to 24.76 after surgery, and that in all patients was 18.21. The average number of breaths per minute in the experimental group was between 10.56 and 21.03, and that in all patients was 16.43. The patients’ average respiration per minute after operation was within the standard index range, and the average respiration times of experimental group were slightly lower, indicating that experimental method can better protect lung function of patients.
Observations were made on the patient’s mechanical ventilation time, clinical pulmonary infection score, ICU hospitalization time, and incidence of secondary intubation, as shown in Table 3.
In Table 3, there was no significant difference in each index (P > 0.05). Patients’ life quality was observed 3 months after operation, and the Minnesota quality of life scale, cardiopulmonary rehabilitation MWT, and chronic heart failure scale were used as scoring items, as shown in Table 4.
In Table 4, difference showed in the Minnesota quality of life score before the intervention (P = 0.016), and difference was more significant after the intervention. The results of MWT of cardiopulmonary rehabilitation in two groups were statistically different (P = 0.011). Six-minute walk test results of cardiopulmonary rehabilitation in the experimental group reached 529.75 ± 66.68, which was higher than 493.08 ± 70.32 in the other, indicating that cardiopulmonary rehabilitation effect in experimental group was better. No difference showed in chronic heart failure score between them at 3 months after operation (P = 0.346).
Lung segment surgery is a common and effective treatment of lung disease. During the operation, doctors will locate and remove the diseased lung segment, and carry out necessary repair and suture, which can effectively control the spread of disease and improve patients life quality and respiratory function[14]. During lung segment surgery, patients may have bleeding, and severe bleeding requires additional nursing measures[15]. After the completion of lung surgery, patients need to face the problem of possible postoperative infection. Postoperative pain and dyspnea will lead to the decline of the patient’s living standard. In severe cases, special nursing needs to be arranged[16,17]. Operating room nursing can help patients with surgery and postoperative rehabilitation during lung segment surgery, generally including assisting in surgical operation, ensuring patient safety, imparting health knowledge, and managing postoperative recovery[18,19]. When patients enter the stage of postoperative rehabilitation, the quality of nursing has become an important factor affecting the recovery speed of patients. The humanized nursing mode starts from the aspects of personalized care, patient satisfaction, and working environment optimization, and timely monitors and analyzes the overall health and recovery of patients, which helps to reduce the physical discomfort and psychological anxiety of patients after lung surgery[20-22]. After lung surgery, different patients’ physical recovery is different, and using the same nursing methods may lead to problems such as reduced recovery speed or adverse reactions. At present, the nursing of patients after lung surgery includes nutritional support, respiratory rehabilitation training, pain management, gas assistance and other means. Gas assistance is simple and generally does not conflict with other auxiliary means. It has become a commonly used auxiliary means, in which nitrogen oxide is the most common material.
The FEV1 value reflects the volume of exhaled gas volume in the first second when the patient exhales with the most force after the maximum deep inspiration, and the FVC value reflects the maximum volume of exhaled gas when the patient exhales with the fastest speed after the maximum deep inspiration. In clinic, the ratio of FEV1 value and FVC value is abbreviated as one second rate, which is used as a detection index of lung function to judge whether there is restrictive ventilation dysfunction or obstructive ventilation dysfunction in patients’ lungs. In the rehabilitation process after lung surgery, the FEV1/FVC value of patients will rise from a low level to a normal level. Two kinds of nursing rehabilitation programs were used for the rehabilitation nursing of patients after lung segment surgery, and both methods could improve the FEV1/FVC value of patients. The patients FEV1/FVC values were statistically significant. In the monitoring time of 3 wk after operation, the FEV1/FVC value of female patients in the experimental group increased to 79.72 ± 1.23, and the FEV1/FVC value of male patients increased to 84.78 ± 1.84, which were higher than the FEV1/FVC value of patients in control group. The experimental method can more effectively avoid patients’ ventilation dysfunction. MIP value reflects the maximum value of oral suction pressure that the patient can produce as best as possible when the airway is blocked in functional residual air position and residual air position. Clinically, MIP value, as a detection index of respiratory muscle function of patients, is used to judge the respiratory muscle function after the occurrence of respiratory system related diseases. In the process of rehabilitation after lung surgery, the MIP value of patients will continue to rise from a lower level. Two kinds of nursing rehabilitation programs were used for the rehabilitation nursing of patients after lung segment surgery, and both methods could improve the MIP value of patients. During the monitoring time of 3 wk after operation, the MIP value of female patients in the experimental group increased to 50.13 ± 11.29, and that of male patients increased to 58.89 ± 7.14, which were higher. It shows that research method can more effectively improve respiratory muscle function of patients after lung surgery. The MEP value reflects the expiratory pressure that can be produced by full expiratory effort after airway blockade at the total lung volume level. Clinically, MEP value, as a detection index of shouting respiratory muscle strength, is used to judge the respiratory system muscle function of patients after surgery. In the rehabilitation process after lung surgery, the MEP value of patients will continue to rise from a lower level. Two kinds of nursing rehabilitation programs were used for the rehabilitation nursing of patients after lung segment surgery, and both methods could improve the MEP value of patients. In the monitoring time of 3 wk after operation, the MEP value of female patients in the experimental group increased to 92.03 ± 2.89, and that of male patients increased to 95.99 ± 3.38, which were higher. The research method can more effectively improve the respiratory system muscle function of patients after lung surgery.
There were differences in the rehabilitation technology used by the two groups. The control group received routine nursing scheme, and the experimental group received operation room nursing by humanized nursing mode combined with nitric oxide rehabilitation scheme. Compared with the two groups, the experimental group had better rehabilitation effect on patients, but due to the complexity of using nursing strategies, the cost of nursing was higher. The recovery time in experimental group was in the range of 25.8-56.6 wk, which was shorter. The duration of mechanical ventilation, clinical pulmonary infection score, ICU stay and the incidence of secondary intubation in experimental group were lower, but comparison was not significant (P > 0.05). The final score of Minnesota quality of life scale in experimental group was 71.65 ± 5.42, which was lower; MWT result of cardiopulmonary rehabilitation was 529.75 ± 66.68, which was better.
According to the above analysis, the two groups of nursing rehabilitation programs can improve the rehabilitation of patients, but there are differences in the effect. The experimental group had better overall rehabilitation effect, but the cost of nursing was relatively higher. At the same time, the individual differences of patients lead to great differences in the rehabilitation effect. More indicators need to be monitored in the actual treatment to improve the rehabilitation efficiency of patients. The study combines a humanized nursing model with nitric oxide inhalation, providing a new perspective for the care and rehabilitation of patients after lung surgery. This comprehensive nursing model not only focuses on the physiological needs of patients, but also values their psychological state and personalized needs, thereby promoting comprehensive recovery of patients at multiple levels. By introducing nitric oxide inhalation during the nursing process, patients can promote pulmonary blood circulation, reduce inflammatory reactions, accelerate wound healing, and thus improve rehabilitation efficiency on a physiological level. Nursing staff provide professional health education to help patients and their families better understand the disease and rehabilitation process, alleviate their anxiety and fear, and enhance their confidence and enthusiasm for rehabilitation. From an economic perspective, research methods can help reduce overall treatment costs for patients and alleviate their financial burden by reducing complications and shortening hospital stay. It is of great significance to improve the quality of life and satisfaction of patients. The research method helps to improve the overall nursing level of patients after lung surgery, and provides more comprehensive, efficient, and humane rehabilitation services for patients.
This retrospective study evaluates the effects of a humanized nursing mode combined with nitric oxide inhalation on postoperative rehabilitation in lung surgery patients. Our findings indicate significant improvements in pulmonary function and recovery times, and a reduction in treatment costs for the experimental group compared to controls. These results suggest that integrating humanized nursing with nitric oxide inhalation can effectively enhance rehabilitation outcomes and reduce the economic burden on patients.
| 1. | Johnson BA, Waddimba AC, Ogola GO, Fleshman JW Jr, Preskitt JT. A systematic review and meta-analysis of surgery delays and survival in breast, lung and colon cancers: Implication for surgical triage during the COVID-19 pandemic. Am J Surg. 2021;222:311-318. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 27] [Cited by in RCA: 82] [Article Influence: 16.4] [Reference Citation Analysis (0)] |
| 2. | Rice D, Rodriguez-Restrepo A, Mena G, Cata J, Thall P, Milton D, Correa A, Woodard T, Antonoff M, Hofstetter W, Roth J, Sepesi B, Swisher S, Walsh G, Vaporciyan A, Mehran R. Matched Pairs Comparison of an Enhanced Recovery Pathway Versus Conventional Management on Opioid Exposure and Pain Control in Patients Undergoing Lung Surgery. Ann Surg. 2021;274:1099-1106. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 22] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 3. | Cai Y, Hao Z, Gao Y, Ping W, Wang Q, Peng S, Zhao B, Sun W, Zhu M, Li K, Han Y, Kuang D, Chu Q, Fu X, Zhang N. Coronavirus Disease 2019 in the Perioperative Period of Lung Resection: A Brief Report From a Single Thoracic Surgery Department in Wuhan, People’s Republic of China. J Thorac Oncol. 2020;15:1065-1072. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 71] [Cited by in RCA: 80] [Article Influence: 16.0] [Reference Citation Analysis (0)] |
| 4. | Zhang Y, Ma X, Shen X, Wang S, Li Y, Hu H, Chen H. Surgery for pre- and minimally invasive lung adenocarcinoma. J Thorac Cardiovasc Surg. 2022;163:456-464. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 35] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 5. | Charlot M, Stein JN, Damone E, Wood I, Forster M, Baker S, Emerson M, Samuel-Ryals C, Yongue C, Eng E, Manning M, Deal A, Cykert S. Effect of an Antiracism Intervention on Racial Disparities in Time to Lung Cancer Surgery. J Clin Oncol. 2022;40:1755-1762. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 36] [Article Influence: 12.0] [Reference Citation Analysis (0)] |
| 6. | Tong C, Li T, Huang C, Ji C, Liu Y, Wu J, Xu M, Cao H. Risk Factors and Impact of Conversion to Thoracotomy From 20,565 Cases of Thoracoscopic Lung Surgery. Ann Thorac Surg. 2020;109:1522-1529. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 16] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 7. | Chang JY, Mehran RJ, Feng L, Verma V, Liao Z, Welsh JW, Lin SH, O’Reilly MS, Jeter MD, Balter PA, McRae SE, Berry D, Heymach JV, Roth JA; STARS Lung Cancer Trials Group. Stereotactic ablative radiotherapy for operable stage I non-small-cell lung cancer (revised STARS): long-term results of a single-arm, prospective trial with prespecified comparison to surgery. Lancet Oncol. 2021;22:1448-1457. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 207] [Article Influence: 51.8] [Reference Citation Analysis (0)] |
| 8. | Hino H, Saito T, Matsui H, Taniguchi Y, Murakawa T. Utility of Geriatric Nutritional Risk Index in patients with lung cancer undergoing surgery. Eur J Cardiothorac Surg. 2020;58:775-782. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 16] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 9. | Maringe C, Benitez Majano S, Exarchakou A, Smith M, Rachet B, Belot A, Leyrat C. Reflection on modern methods: trial emulation in the presence of immortal-time bias. Assessing the benefit of major surgery for elderly lung cancer patients using observational data. Int J Epidemiol. 2020;49:1719-1729. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 59] [Cited by in RCA: 101] [Article Influence: 20.2] [Reference Citation Analysis (0)] |
| 10. | Chang SH, Zervos M, Kent A, Chachoua A, Bizekis C, Pass H, Cerfolio RJ. Safety of patients and providers in lung cancer surgery during the COVID-19 pandemic. Eur J Cardiothorac Surg. 2020;58:1222-1227. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 11] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 11. | Veluswamy RR, Whittaker Brown SA, Mhango G, Sigel K, Nicastri DG, Smith CB, Bonomi M, Galsky MD, Taioli E, Neugut AI, Wisnivesky JP. Comparative Effectiveness of Robotic-Assisted Surgery for Resectable Lung Cancer in Older Patients. Chest. 2020;157:1313-1321. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 39] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 12. | Tamminga M, de Wit S, van de Wauwer C, van den Bos H, Swennenhuis JF, Klinkenberg TJ, Hiltermann TJN, Andree KC, Spierings DCJ, Lansdorp PM, van den Berg A, Timens W, Terstappen LWMM, Groen HJM. Analysis of Released Circulating Tumor Cells During Surgery for Non-Small Cell Lung Cancer. Clin Cancer Res. 2020;26:1656-1666. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 30] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 13. | El Husseini K, Baste JM, Bouyeure-Petit AC, Lhuillier E, Cuvelier A, Decazes P, Vera P, Similowski T, Patout M. Respiratory muscle metabolic activity on PET/CT correlates with obstructive ventilatory defect severity and prognosis in patients undergoing lung cancer surgery. Respirology. 2023;28:551-560. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 14. | Furák J, Paróczai D, Burián K, Szabó Z, Zombori T. Oncological advantage of nonintubated thoracic surgery: Better compliance of adjuvant treatment after lung lobectomy. Thorac Cancer. 2020;11:3309-3316. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 13] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 15. | Batihan G, Ceylan KC, Usluer O, Kaya ŞÖ. Video-Assisted Thoracoscopic Surgery vs Thoracotomy for Non-Small Cell Lung Cancer Greater Than 5 cm: Is VATS a feasible approach for large tumors? J Cardiothorac Surg. 2020;15:261. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 15] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 16. | Hu J, Chen Y, Dai J, Zhu X, Gonzalez-Rivas D, Jiang G, Li H, Zhang P. Perioperative outcomes of robot-assisted vs video-assisted and traditional open thoracic surgery for lung cancer: A systematic review and network meta-analysis. Int J Med Robot. 2020;16:1-14. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 12] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 17. | Meijer RPJ, Neijenhuis LKA, Zeilstra AP, Roerink SF, Bhairosingh SS, Hilling DE, Mieog JSD, Kuppen PJK, Sier CFM, Braun J, Burggraaf J, Vahrmeijer AL, Cohen D, Hutteman M. Data-Driven Identification of Targets for Fluorescence-Guided Surgery in Non-Small Cell Lung Cancer. Mol Imaging Biol. 2023;25:228-239. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 7] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 18. | Karush JM, Alex G, Geissen N, Wakefield C, Basu S, Liptay MJ, Seder CW. Predicting Non-home Discharge After Lung Surgery: Analysis of the General Thoracic Surgery Database. Ann Thorac Surg. 2023;115:687-692. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 4] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 19. | Colson YL, Shepard JO, Lennes IT. New USPSTF Guidelines for Lung Cancer Screening: Better but Not Enough. JAMA Surg. 2021;156:513-514. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 15] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 20. | Luo LZ, Liu JJ. Effects of the Humanized Nursing Model in Obstetric Nursing Based on the Use and Gratification Theory. J Mod Nurs Pract Res. 2022;. [DOI] [Full Text] |
| 21. | Ichimura H, Kobayashi K, Gosho M, Nakaoka K, Yanagihara T, Ueda S, Saeki Y, Maki N, Kobayashi N, Kikuchi S, Suzuki H, Goto Y, Sato Y. Preoperative predictors of restoration in quality of life after surgery for lung cancer. Thorac Cancer. 2021;12:835-844. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 5] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 22. | Zhou X, Zeng W, Rong S, Lv H, Chen Y, Mao Y, Tan W, Li H. Alendronate-Modified Nanoceria with Multiantioxidant Enzyme-Mimetic Activity for Reactive Oxygen Species/Reactive Nitrogen Species Scavenging from Cigarette Smoke. ACS Appl Mater Interfaces. 2021;13:47394-47406. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 19] [Article Influence: 4.8] [Reference Citation Analysis (0)] |