Published online Jun 16, 2024. doi: 10.12998/wjcc.v12.i17.3265
Revised: April 22, 2024
Accepted: April 29, 2024
Published online: June 16, 2024
Processing time: 91 Days and 13.6 Hours
This study aimed to describe the findings of double superior mesenteric veins (SMVs), a rare anatomical variation, on multidetector computer tomography (MDCT) and magnetic resonance imaging (MRI) images.
We describe the case of a 34-year-old male, who underwent both MDC and MRI examinations of the upper abdomen because of liver cirrhosis. MDCT and MRI angiography images of the upper abdomen revealed an anatomic variation of the superior mesenteric vein (SMV), the double SMVs.
The double SMVs are a congenital abnormality without potential clinical manife
Core Tip: Although double superior mesenteric veins (SMVs) are rare, they might be a congenital abnormality that do not show any clinical symptoms. Knowledge of the possibility of such variations could be beneficial during a pancreaticoduodenectomy, treatment of thrombosis and aneurysms of SMV, as well as in radiological interpretations and treatments.
- Citation: Tang W, Peng S. Multidetector computer tomography and magnetic resonance imaging of double superior mesenteric veins: A case report. World J Clin Cases 2024; 12(17): 3265-3270
- URL: https://www.wjgnet.com/2307-8960/full/v12/i17/3265.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i17.3265
The superior mesenteric vein (SMV) is the largest branch of the portal vein system[1]. Pancreatoduodenectomy, colectomy, portosystemic shunts, and liver transplantation, as well as several surgeries on the pancreas and extrahepatic biliary pathways, require detailed knowledge of the normal anatomy of SMV and its variations[2-4].
The normal anatomy of SMV is generally described as a single trunk, located on the right side of the artery of the same name, with its chief tributaries including the ileocolic, gastrocolic, right colic, and middle colic veins[5]. The anatomic patterns of the SMV, as described on multidetector computer tomography (MDCT), have been reported in some studies[6]. A single common SMV trunk was observed in most of these studies[7], and the absence of the main trunk of the SMV, and double SMVs were observed in very few studies[8]. The anatomic variation of double SMVs has been described on MDCT, to our knowledge, there are no descriptions of double SMVs based on magnetic resonance imaging (MRI). In the study, we describe a case of double SMVs in patients with liver cirrhosis who underwent both MDCT and MRI examinations of the upper abdomen, and discuss the possible mechanism underlying this anatomical variation.
The case report was a retrospective and observational study. The Institutional Ethical Committee approved the study protocol. The chief complaints were darkening urine of 1 wk’s duration and vomiting blood (approximately 100 mL) and tarry stools 2 d prior to presentation.
The patient was a 34-year-old male with a history of viral hepatitis B for more than 10 years without regular treatment. One week prior to presentation, the patient noticed darkening urine without any decrease in urine output after taking a drug to treat a cold. The urine color returned to normal after 3 d. Two days before presentation, the patient reported vomiting about 100 mL of dark-red blood containing blood clots with no obvious causes, and producing tarry stools five times a day. The patient had drank about 1000 mL of beer the day before vomiting. An endoscopy of the stomach presented varicose veins in the esophagus and stomach fundus at the outpatient clinic. The patient was admitted to the Department of Gastroenterology with cirrhosis and upper gastrointestinal bleeding.
The patient had a history of viral hepatitis B for more than 10 years.
The patient denied any family history of viral hepatitis. Smoking for 8 years, 10-20 cigarettes per day. Drinking for over 10 years, with approximately 2000-3000ml of beer per day.
On physical examination, the vital signs were a hepatic face, with a dark and dull facial color; in addition to emaciation, with mild abdominal distention and varicose veins in the abdominal wall; Liver enlargement was also detected, extending approximately 3 cm to the lower edge of the rib arch, as well as spleen enlargement extending 2 cm below the rib margin; Small artery dilation of local skin on the face, neck, chest, and back of hand forming “spider angioma” were observed.
The abnormal indicators of hepatitis B virus screening and liver function laboratory examination were as follows: Hepatitis B surface antigen positive; aspartate aminotransferase (58 U/L↑); glutamyl transpeptidase (607 U/L↑); leucine aminotransferase (81 U/L↑); prealbumin (111.4 mg/L↓); albumin (35.6 g/L↓); total bile acids (48.5 μmol/L↑); total bilirubin (61.4 μmol/L↑); and Direct bilirubin (46.1 μmol/L↑).
After admission, an abdominal ultrasonography showed uneven liver echo, splenomegaly, and a small amount of ascites, indicative of liver cirrhosis and portal hypertension. Contrast-enhanced MDCT and MRI of the upper abdomen were completed for further characterization and revealed an anatomical variation of the superior mesenteric vein (SMV), namely, the double SMVs, in addition to liver cirrhosis, portal hypertension, splenomegaly, tortuous and dilated vessels in the splenic hilum, collateral circulation formation in the lower esophagus and stomach fundus, and a small number of ascites.
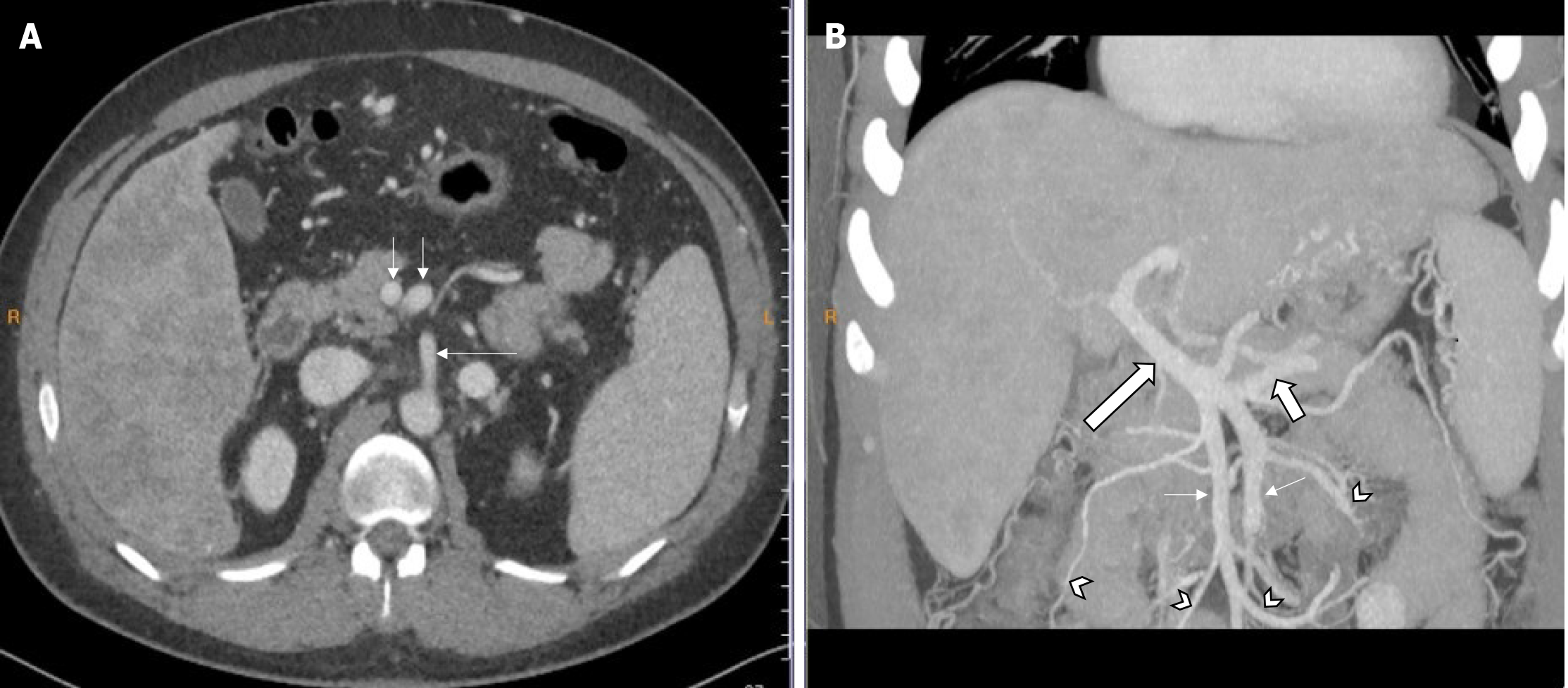
On MDCT and MRI images, in terms of the position of the double SMVs and the superior mesenteric artery (SMA), the left SMV was located in front of the SMA, and the right SMV was located on the right front side of the SMA (Figure 1A). The left and right SMVs joined the portal vein in parallel, together with the splenic veins (Figure 1B and Figure 2). The left SMV received the blood from the proximal small intestine, and the right SMV received the blood from the distal small intestine and the proximal colon (Figure 1B and Figure 2).
The final diagnosis was as follows: Viral hepatitis B, decompensated liver cirrhosis, portal hypertension, upper gastrointestinal bleeding, ascites, and anatomical variation of SMV.
During hospitalization, the patient received treatment methods for liver cirrhosis, such as nutritional support, maintaining the electrolyte balance, anti-hepatitis B virus therapy, protecting liver function, and reducing portal vein pressure.
After one week of treatment, the patient experienced significant improvement in the corresponding symptoms and was discharged from the hospital. The attending physician advised the patient to continue taking antiviral drugs and liver protection medication, and to quit alcohol. Additionally, the patient was advised to continue with outpatient follow-up.
We define double SMVs as separate left and right mesenteric trunks, both of which join the portal vein in parallel, together with the splenic vein. Graf et al[9] firstly described the double SMVs with helical computed tomography venography in 1997, their study found seven patients with two mesenteric trunks merged separately with the splenic vein in 54 patients. According to reports, the lowest incidence of double SMVs was 9.1%, and the highest was 23.5%[9-11]. The incidence of the double SMVs may differ in other countries, regions, or populations. Therefore, a multicenter study with a larger cohort should be considered for the incidence of double SMVs in the future study.
No studies on MRI imaging of double SMVs have been reported. In our study, magnetic resonance venography cleared showed the trunk and branches of the double SMVs. In recent times, there have been significant advancements in gradient technology and software design that have revolutionized the field of MRI imaging, and it is now possible to implement thin-section three-dimensional (3D) contrast-enhanced dynamic fat-suppressed magnetic resonance imaging in abdominal studies. This technique has the potential to improve the visualization of the SMV and its branches[12].
As far as I know, the anatomic types of SMV trunk can be divided into three types, including a single common trunk with variable length, a right and left trunk merged separately with the splenic vein to form the portal vein (double SMVs), and absence of a common trunk. The anatomic type of double SMVs can be divided into two subtypes (m and p) according to the left trunk joining sites, double trunks joining on the caudal side of the splenoportal confluence (subtype m), and double trunks where the left one joined the splenic vein (subtype p)[11]. According to this anatomical classification definition, the presented case belongs to subtype m.
The absence of a common SMV trunk is as rare as double SMVs. Dubovan et al[8] reported a case of SMV absence with intestinal malrotation. An abdominal MDCT image of this case showed the absence of the main trunk of the SMV. In this case, the SMV was comprised of the proximal section and the distal section of the collateral branches, and the proximal and distal sections of the SMV were not connected but surrounded the SMA independently.
Considering the embryonic development of the venous system, the yolk sac blood vessels formed in the 4th embryo week. Paired yolk sac veins form a venous plexus in the midgut mesentery[13]. Subsequently, venous plexus with endothelium in the midgut mesentery provides the SMV. The SMV is considered to develop in situ in the midgut mesentery secondary to regression of the left vitelline vein[14]. As SMV embryogenesis is a very delicate process, it is conceivable that defects in vascular connections and regression within this vein network could lead to anatomic variants of the SMV. However, the specific embryology mechanism underlying the formation of the three anatomical configurations of the SMV remains unknown, and further research is needed.
Insufficient understanding of the unique structure of double SMVs may have surgical consequences. For example, precise identification of anatomical variations of the SMV is imperative for D3 lymphadenectomy in right-sided colon cancer due to its critical anatomical landmark[15]. For patients with double SMVs and the left SMV trunk located on the left or anterolateral side of the SMA, attention should be paid to avoid damaging the left SMV trunk during intraoperative D3 lymphadenectomy. If a patient is found to have a double SMV anatomical variation through 3D reconstruction images of MDCT or MRI before surgery, it is not necessary to dissect the left SMV during the operation. This can help minimize the risk of intraoperative bleeding, which in turn can facilitate lymph node dissection and tumor removal[16].
In a patient with a double SMV anatomical type, if there is tumor invasion and an isolated thrombus present on the right trunk of the double SMVs, or if there are serious injuries to the right SMV during a right hemicolectomy, removal of the right SMV in the absence of anastomosis may be considered. This decision should be based on MDCT or MRI images that show unobstructed venous return from the small intestine and distal colon veins. In addition, the right trunk of double SMVs can not be mistaken as a relatively thick ileocolic vein and resected during the operation during a laparoscopic right hemicolectomy[17].
To our knowledge, only a few studies have reported clinical management strategies for double SMA anatomical variation in right-sided colon cancer[16]. The clinical management strategy of double SMVs in colon cancer described above is based on a retrospective analysis of individual cases and a summary of personal experience. There is currently no cohort comparative study based on a certain sample size to analyze the clinical management strategy of double SMVs in colon cancer. The management of double SMVs during pancreaticoduodenectomy and the treatment of SMV thrombosis and aneurysms have not been reported yet. Due to the low incidence of double SMA anatomical variations, it is not yet widely understood how this anatomical variation affects patient management in specific clinical settings.
Although double SMVs are rare, they might be a congenital abnormality that do not show any clinical symptoms. The purpose of this case study was to draw attention to the anatomical variations of SMVs. Knowledge of the possibility of such variations could be beneficial during a pancreaticoduodenectomy, treatment of thrombosis and aneurysms of SMV, as well as in radiological interpretations and treatments.
| 1. | Kim HJ, Ko YT, Lim JW, Lee DH. Radiologic anatomy of the superior mesenteric vein and branching patterns of the first jejunal trunk: evaluation using multi-detector row CT venography. Surg Radiol Anat. 2007;29:67-75. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 41] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 2. | Negoi I, Beuran M, Hostiuc S, Negoi RI, Inoue Y. Surgical Anatomy of the Superior Mesenteric Vessels Related to Colon and Pancreatic Surgery: A Systematic Review and Meta-Analysis. Sci Rep. 2018;8:4184. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 73] [Cited by in RCA: 56] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 3. | Negoi I, Beuran M, Hostiuc S, Negoi RI, Inoue Y. Surgical Anatomy of the Superior Mesenteric Vessels Related to Pancreaticoduodenectomy: a Systematic Review and Meta-Analysis. J Gastrointest Surg. 2018;22:802-817. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 24] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 4. | Akita M, Maeda E, Nishimura T, Abe K, Kozuki A, Yokoyama K, Tanaka T, Kishi S, Kaneda K. Anatomical change of SMV branches after the Cattell Braasch maneuver facilitates safe resection around the uncinated process in pancreatoduodenectomy. BMC Surg. 2021;21:341. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 5. | Horton KM, Fishman EK. CT angiography of the mesenteric circulation. Radiol Clin North Am. 2010;48:331-345, viii. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 42] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 6. | Zerin JM, DiPietro MA. Mesenteric vascular anatomy at CT: normal and abnormal appearances. Radiology. 1991;179:739-742. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 44] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 7. | Katz MH, Fleming JB, Pisters PW, Lee JE, Evans DB. Anatomy of the superior mesenteric vein with special reference to the surgical management of first-order branch involvement at pancreaticoduodenectomy. Ann Surg. 2008;248:1098-1102. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 66] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 8. | Dubovan P, Tomáš M, Pavlendová J, Dolník J, Aziri R, Pinďák D. Superior mesenteric vein absence with intestinal malrotation: a case report. BMC Surg. 2022;22:39. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 9. | Graf O, Boland GW, Kaufman JA, Warshaw AL, Fernandez del Castillo C, Mueller PR. Anatomic variants of mesenteric veins: depiction with helical CT venography. AJR Am J Roentgenol. 1997;168:1209-1213. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 50] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 10. | Kuzu MA, İsmail E, Çelik S, Şahin MF, Güner MA, Hohenberger W, Açar Hİ. Variations in the Vascular Anatomy of the Right Colon and Implications for Right-Sided Colon Surgery. Dis Colon Rectum. 2017;60:290-298. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 54] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 11. | Sakaguchi T, Suzuki S, Morita Y, Oishi K, Suzuki A, Fukumoto K, Inaba K, Kamiya K, Ota M, Setoguchi T, Takehara Y, Nasu H, Nakamura S, Konno H. Analysis of anatomic variants of mesenteric veins by 3-dimensional portography using multidetector-row computed tomography. Am J Surg. 2010;200:15-22. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 78] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 12. | Ito K, Blasbalg R, Hussain SM, Mitchell DG. Portal vein and its tributaries: evaluation with thin-section three-dimensional contrast-enhanced dynamic fat-suppressed MR imaging. Radiology. 2000;215:381-386. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 48] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 13. | Kim JH, Jin ZW, Yamamoto M, Murakami G, Abe SI, Rodríguez-Vázquez JF. Anatomy of the vitelline vein remnant in human embryos and fetuses. Surg Radiol Anat. 2022;44:1219-1230. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 14. | Abe H, Yamamoto M, Yanagisawa N, Morimoto R, Murakami G, Rodríguez-Vázquez JF, Abe S. Regressing vitelline vein and the initial development of the superior mesenteric vein in human embryos. Okajimas Folia Anat Jpn. 2017;94:87-92. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 4] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 15. | Peltrini R, Luglio G, Pagano G, Sacco M, Sollazzo V, Bucci L. Gastrocolic trunk of Henle and its variants: review of the literature and clinical relevance in colectomy for right-sided colon cancer. Surg Radiol Anat. 2019;41:879-887. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 25] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 16. | Guo S, Yu T, Chen X, Cui M, Liu D, Xu S, Lu J, Zhang H. Variations of the double superior mesenteric vein are not rare: An observational study using computed tomography, three-dimensional image reconstruction, and surgery. Eur J Surg Oncol. 2023;49:106972. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 17. | Alsabilah J, Kim WR, Kim NK. Vascular Structures of the Right Colon: Incidence and Variations with Their Clinical Implications. Scand J Surg. 2017;106:107-115. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 41] [Article Influence: 4.6] [Reference Citation Analysis (0)] |