Published online Jun 16, 2024. doi: 10.12998/wjcc.v12.i17.3253
Revised: April 10, 2024
Accepted: April 19, 2024
Published online: June 16, 2024
Processing time: 91 Days and 1.1 Hours
In addition to the non-specific symptomatology of ocular rosacea, currently, there are no reliable diagnostic tests for the disease, which may lead to its misdiagnosis. Here, we report a case of ocular rosacea presenting with multiple recurrent cha
A 63-year-old female patient presented with multiple chalazion and dry eyes in both eyes, with no facial erythema. Initial management done were application of steroid eye ointment on both eyelids, hot compresses, and eyelid margin cleaning; noting that there was no relief of symptoms. Surgical excision of the chalazion was done on both eyes, however, bilateral recurrence occurred post-operatively. The pathological studies showed infiltration of a small amount of fibrous tissue with many chronic inflammatory cells. Immunohistochemistry studies were positive for LL-37. Resolution of the chalazion occurred after oral administration of doxycycline and azithromycin.
Our findings show that ophthalmologists should recognize the ocular manifestations of skin diseases.
Core Tip: In this study, we demonstrate for the first time that bilateral recurrent chalazion refractory to conventional treatment may indicate ocular rosacea. Given that ocular rosacea solely presents with ocular symptoms without facial manifestations, it is not only prone to misdiagnosis by dermatologists but also frequently mistaken as mere blepharitis by ophthalmologists. Therefore, our identification of the potential association between bilateral recurrent chalazion lacking facial symptoms and ocular rosacea holds significant implications in alerting both dermatologists and ophthalmologists.
- Citation: Han XM, Zhou YM, Cen LS. Ocular rosacea without facial erythema involvement manifesting as bilateral multiple recurrent chalazions: A case report. World J Clin Cases 2024; 12(17): 3253-3258
- URL: https://www.wjgnet.com/2307-8960/full/v12/i17/3253.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i17.3253
Rosacea is a chronic inflammatory facial disease, with ocular rosacea classified as the first out of four distinct clinical subtypes in 2002[1]. The diagnosis of ocular rosacea is based on medical history and clinical observation. Ocular rosacea appears as a spectrum of disease, from meibomian gland dysfunction to the appearance of a chalazion. Eye examination shows a series of features, including chalazion, telangiectasia of the lid margin, interpalpebral conjunctival injection, spade-shaped infiltrates in the cornea, scleritis, and sclerokeratitis[2]. Thus, differentiating the symptoms of ocular rosacea from that of other ocular surface diseases may be difficult. Moreover, there is no definitive laboratory test for the diagnosis of ocular rosacea; thus, ocular rosacea could be easily misdiagnosed by ophthalmologists.
Corneal and conjunctival sensitivity do not change significantly in ocular rosacea; thus, the reported ocular symptoms may not be correlated with the objective test results[3]. Moreover, given that patients with mild symptoms may not seek medical help, and the skin is not usually examined during ophthalmology consults, a certain number of ocular rosacea cases remain undetected. Herein, we present a case of ocular rosacea with recurrent bilateral chalazion, without facial manifestations.
A 63-year-old female patient visited our hospital complaining of multiple red nodules on bilateral eyes and dry eyes for about 4 wk.
Four weeks ago, the patient presented with bilateral red nodules on the upper and lower eyelids without any apparent precipitating factors. The nodules were non-tender, and the patient denied any visual impairment or facial erythema.
The patient suffered from hemicrania and insomnia and would medicate with zolpidem and diazepam when insomnia symptoms were more severe. There was no history of trauma, viral infection, systemic disease, pre-existing ocular disease, or ocular surgery.
The patient's smoking and alcohol consumption history were assessed, with her denying any recent travel, engagement in unsafe sexual activity, or substance abuse.
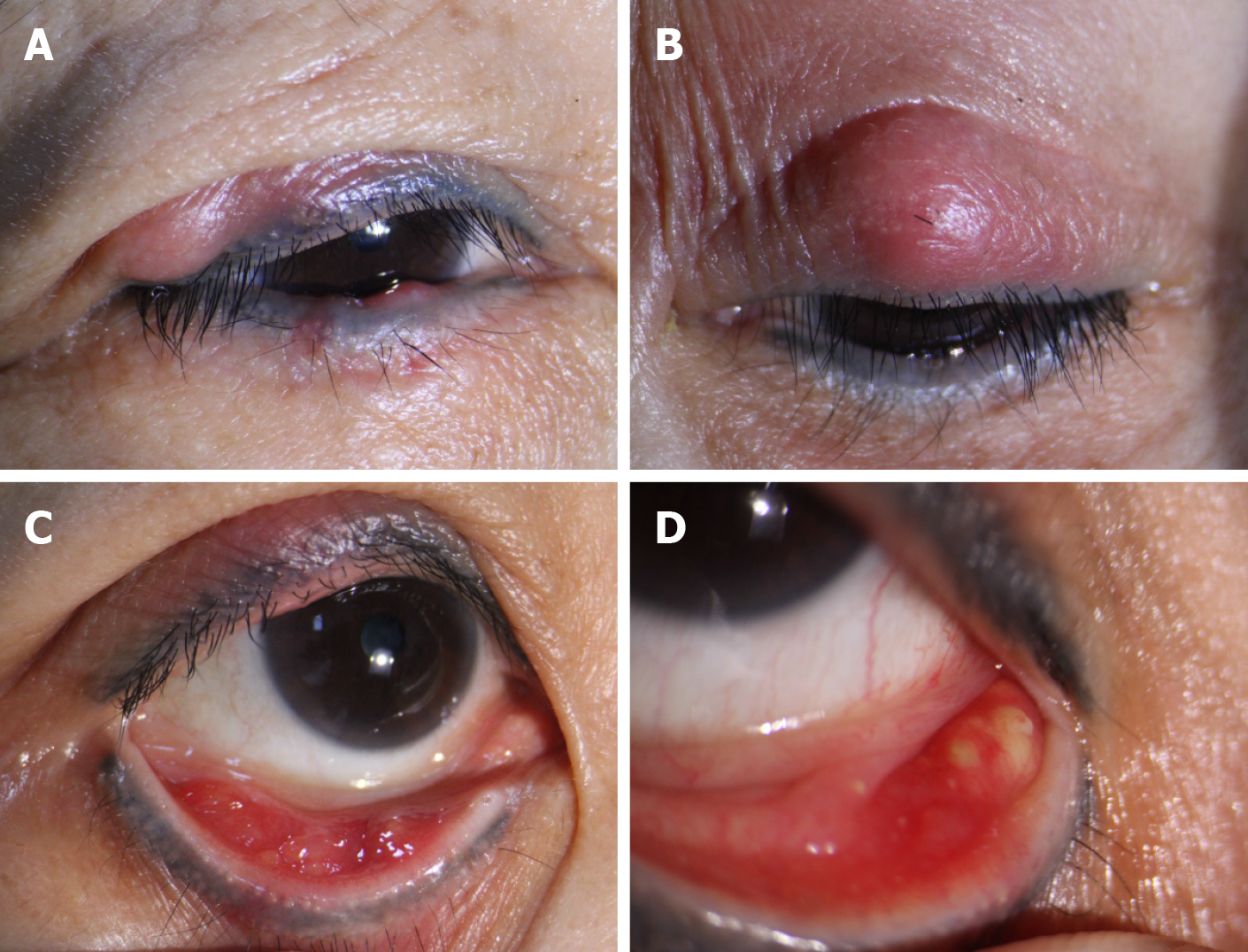
Ophthalmological examination (Figure 1) showed palpebral conjunctiva congestion, no corneal epithelial defects, eyelid margin telangiectasia, and multiple, non-tender, erythematous, fleshy nodular lesions on the bilateral upper and lower eyelids. The tear film rupture time was < 5 s. The visual acuity and examinations of the anterior and posterior segment were normal. There was no lesion on the nose and cheek.
There was no regional lymphadenopathy, and her general examination was unremarkable.
Except for the elevated blood lipids and elevated cholesterol levels (total cholesterol, 7.51 mmol/L; high-density cholesterol, 2.74 mmol/L; and low-density cholesterol, 4.62 mmol/L), other indicators of hematology and biochemical examinations were within the normal range. Serological tests for human immunodeficiency virus and syphilis were negative.
The final diagnosis for the patient was recurrent chalazion in both eyes, ocular rosacea, dry eye, and hyperlipidemia.
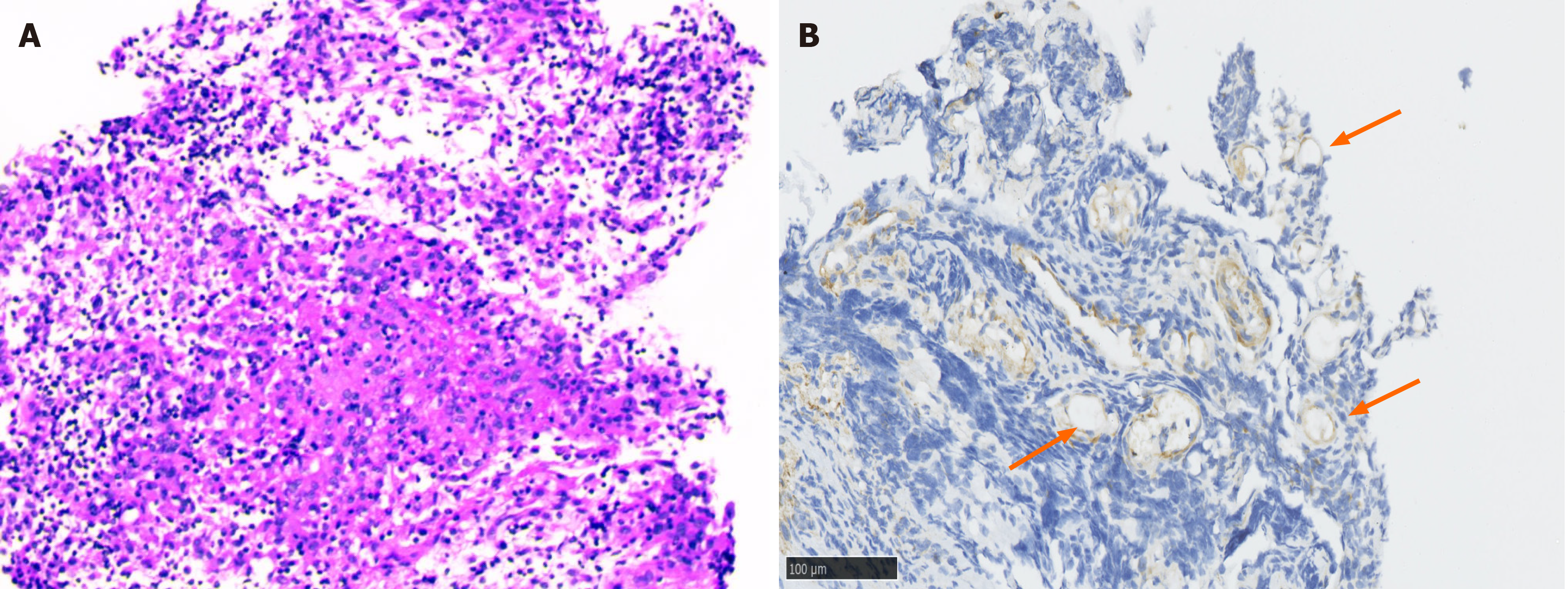
Diagnosed with binocular chalazion and dry eye, the patient was prescribed with artificial tears (Hialid 0.1, Santen Pharmaceutical Co., Ltd., Osaka, Japan), which was applied four times a day, steroid eye ointment (TobraDex, s.a. AlCON-COUVREUR n.v., Puurs, Belgium) which was applied twice a day, and advised hot compresses and the eyelid scrub regimen. After a week, the patient reported slight relief of dry eye symptoms, however, persistence of the red nodules was noted. Local incision and curettage were performed for both eyes, and the excised tissues were sent for pathological examination (Figure 2A). Local tobramycin and dexamethasone eye ointment were given post-surgery.
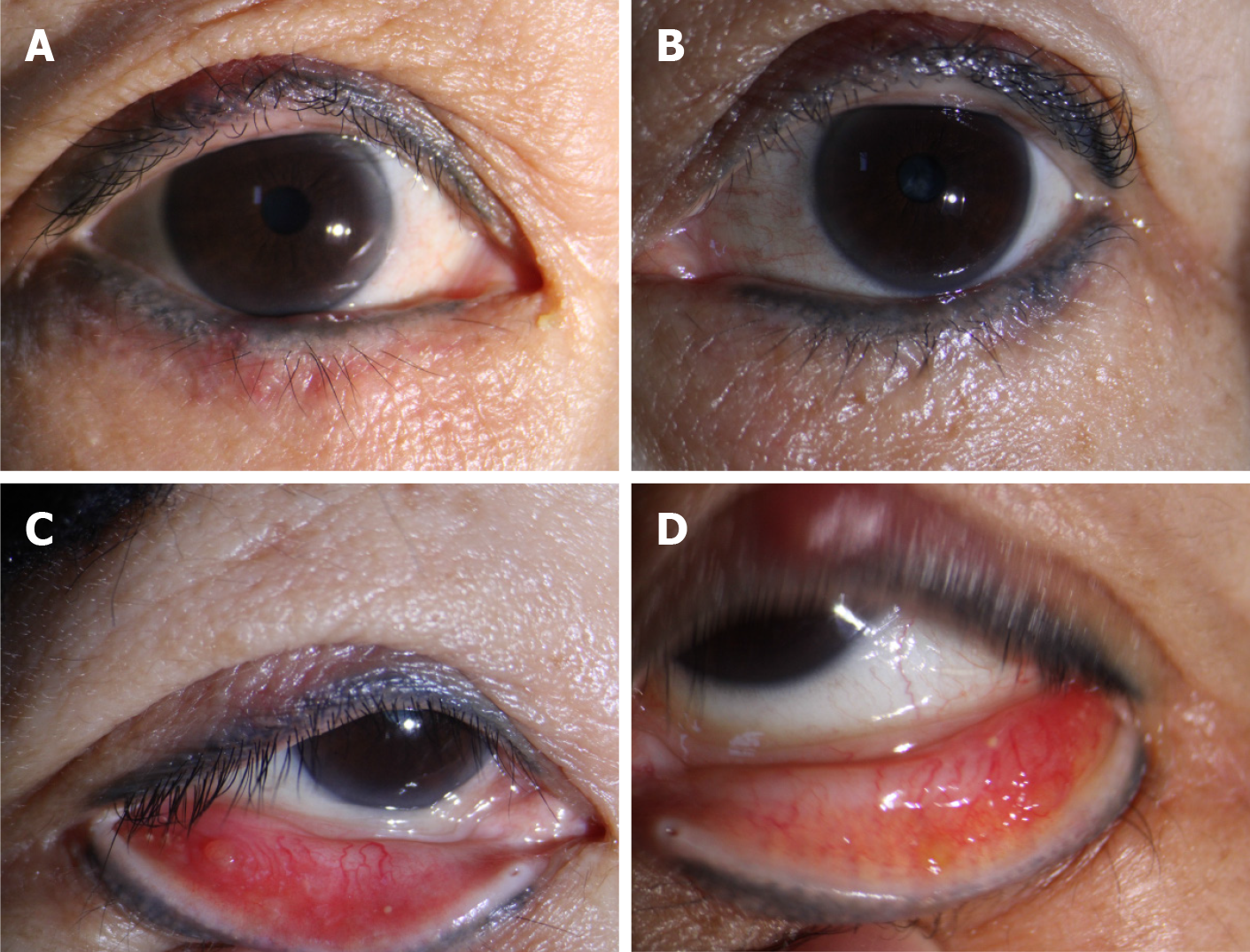
Oral doxycycline (0.1 g, Yongxing Pharmaceutical Co., Ltd., Jiangsu Province, China) was given once daily, and the symptoms improved significantly after a week. However, the patient complained of stomach discomfort; thus, we switched to azithromycin 0.25 g (0.25 g, Pifzer Pharmaceutical Co., Ltd., CT, United States) once daily. After 2 wk of treatment, the conjunctival follicles, dilated palpebral blood vessels, and nodules on both eyes subsided (Figure 3).
After 4 wk, the patient complained of the persistence of symptoms. New red, non-tender nodules were noted on both eyes. Thus, patient underwent another surgery for excision of the red nodules. Then, pathological and immunohistochemical examinations were performed, wherein the dilated postcapillary venules (arrows) tested positive for cathelicidin (LL-37) (Figure 2B).
The ocular variant of rosacea accounts for 10%-50% of the total number of rosacea cases[2]. Externally, readily apparent signs of ocular rosacea include lid margin and conjunctival telangiectases, plugging of the meibomian glands, and chalazion. In this case, bilateral recurrent chalazion were the dominant feature. Chalazion is a chronic inflammatory granuloma, primarily caused by secretion retention of the meibomian gland[4]. Rosacea primarily affects areas where there is a rich supply of sebaceous glands. Chronic inflammation blocks glandular ducts and rosacea is one of the main risks, resulting in chalazion[5].
The nose and cheeks are the most common areas affected by rosacea. In the present case, there were no papules and pustules on the patient’s face, and the eyelids were the only affected areas. Thus, in this case, the chalazion could be the manifestation of the effect of rosacea on the meibomian gland. It is proposed that sebaceous glands may participate in the chronic inflammatory process of rosacea[6]. Skin areas with rich sebaceous gland supply are distinguished by a distinct, noninflammatory immune surveillance[7]. As one of important pathogenesis factors, mites prefer to reside in skin areas particularly where there is rich sebaceous gland supply. In our biopsy of the chalazion, which involved the dermal layer of the eyelid skin, chronic inflammatory changes were found, specifically, dilated venules, which is similar to the findings of lymphoplasmacytic infiltrates in another study[8,9]. Results of our pathological examination also ruled out a malignant tumor, which has a high incidence in the elderly population.
LL-37 is recognized as a biological indicator of rosacea, which is upregulated in lesions of patients with rosacea[10]. In this case, our immunohistochemistry examination of the chalazion showed a positive result for LL-37. Moreover, the chalazion were red, swollen, and non-tender. Manifestations of acute inflammation, such as hordeolum, and other infections were excluded. Most chalazion can be relieved by application of hot compress and topical eye ointment. In this case, the chalazion were persistently red and swollen even after the initial therapy and could not be removed through conventional surgery; however, the chalazion resolved after oral intake of the prescribed medications. Here, we propose persistent bilateral chalazion as another form of papule- or pustule-like eyelid mass.
Telangiectasia is also one of typical clinical manifestations of ocular rosacea. In this case, telangiectases were found on the eyelid margins. Chronic interpalpebral bulbar hyperemia and a papillary reaction were also observed. Keshtcar-Jafari et al[11] found a significant relationship between the severity of telangiectasia and ocular involvement. Hyperemia increases in the interpalpebral space is a characteristic of rosacea conjunctivitis, which presents as persistent non-specific interpalpebral conjunctival injection.
Given that the diagnosis of rosacea is based on clinical manifestations, the sensitivity and specificity of a rosacea diagnosis may inevitably be influenced by varying clinical presentation from different populations. Thus, the exact prevalence of rosacea remains unknown. Moreover, it may be difficult for dermatologists to identify the skin manifestations of rosacea for patient populations with deep-pigmented skin color. Rosacea was thought to be limited to fair-skinned populations, but it can actually affect all ethnicities and skin types, including dark-skinned people[12,13], such as black-skinned and Middle Eastern patients. The presence of some features may obscure the evaluation of other skin manifestations such as inflammatory papules against the background of intense erythema and oedema. Thus, a thorough eye examination can aid dermatologists to correctly diagnose rosacea.
It is believed that rosacea is a skin disease that is involved with other bodily systems. The severity of rosacea was associated with mental illness[14,15] such as depression and anxiety disorders. In this case, the patient has a history of neurologic disorders, specifically, hemicrania and insomnia. Egeberg et al[16] found patients with phymatous rosacea with no significant association with migraine, whereas patients with ocular rosacea showed an increased risk of migraine occurrence, especially for females. Wang et al[17] showed that patients with rosacea had poor sleep quality, and there was a positive correlation between the severity of rosacea and sleep quality. They verified that sleep deprivation affects immune function by affecting immune cells and inflammatory factors. The patient was initially diagnosed with hyperlipidemia, which was easily misdiagnosed because she had no history of risk factors associated with hyperlipidemia such as overweight, diabetes, and cardiovascular disease. Studies have confirmed that patients with rosacea are more prone to having dyslipidemia as well, given the increased levels of total cholesterol, low-density lipoprotein, and triglycerides[18,19]. In the study of Duman et al[20], it was found that the activation of nucleotide-binding oligomerization domain-like receptor 3 may lead to the release of interleukin 1b and induce lipoprotein. Structural changes hinder the ability to break down and transport cholesterol. In a case-control study of Duman et al[20], the incidence of high total cholesterol (> 200 mg/dL) and low-density lipoprotein cholesterol (> 130 mg/dL) levels were more commonly found in patients with rosacea compared to that of the control patients. Rainer et al[21] also found a significant association between hyperlipidemia and rosacea in a skin severity-dependent manner in a case control study. These findings show that the mana
To our knowledge, this is the first case of ocular rosacea that presented as bilateral recurrent chalazion without facial manifestations. Ophthalmologists should be aware of the ocular manifestations of skin disease.
We are grateful to the patient and her family for their collaboration.
| 1. | Wilkin J, Dahl M, Detmar M, Drake L, Feinstein A, Odom R, Powell F. Standard classification of rosacea: Report of the National Rosacea Society Expert Committee on the Classification and Staging of Rosacea. J Am Acad Dermatol. 2002;46:584-587. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 542] [Cited by in RCA: 522] [Article Influence: 22.7] [Reference Citation Analysis (0)] |
| 2. | Rodrigues-Braz D, Zhao M, Yesilirmak N, Aractingi S, Behar-Cohen F, Bourges JL. Cutaneous and ocular rosacea: Common and specific physiopathogenic mechanisms and study models. Mol Vis. 2021;27:323-353. [PubMed] |
| 3. | Örnek N, Karabulut AA, Örnek K, Onaran Z, Usta G. Corneal and conjunctival sensitivity in rosacea patients. Saudi J Ophthalmol. 2016;30:29-32. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 4. | Suzuki T, Katsuki N, Tsutsumi R, Uchida K, Ohashi K, Eishi Y, Kinoshita S. Reconsidering the pathogenesis of chalazion. Ocul Surf. 2022;24:31-33. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 5. | Nemet AY, Vinker S, Kaiserman I. Associated morbidity of chalazia. Cornea. 2011;30:1376-1381. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 34] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 6. | Lee SH, Lee SB, Heo JH, Yoon HS, Byun JW, Choi GS, Shin J. Sebaceous glands participate in the inflammation of rosacea. J Eur Acad Dermatol Venereol. 2020;34:e144-e146. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 7. | Dajnoki Z, Béke G, Kapitány A, Mócsai G, Gáspár K, Rühl R, Hendrik Z, Juhász I, Zouboulis CC, Bácsi A, Bíró T, Törőcsik D, Szegedi A. Sebaceous Gland-Rich Skin Is Characterized by TSLP Expression and Distinct Immune Surveillance Which Is Disturbed in Rosacea. J Invest Dermatol. 2017;137:1114-1125. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 47] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 8. | Starr PA, Macdonald A. Oculocutaneous aspects of rosacea. Proc R Soc Med. 1969;62:9-11. [PubMed] |
| 9. | Ooi XT, Tan KB, Chandran N. A case of pediatric rosacea-Skin and ocular involvement. Clin Case Rep. 2019;7:2414-2416. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 10. | Woo YR, Lim JH, Cho DH, Park HJ. Rosacea: Molecular Mechanisms and Management of a Chronic Cutaneous Inflammatory Condition. Int J Mol Sci. 2016;17:1562. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 70] [Cited by in RCA: 121] [Article Influence: 13.4] [Reference Citation Analysis (0)] |
| 11. | Keshtcar-Jafari A, Akhyani M, Ehsani AH, Ghiasi M, Lajevardi V, Baradran O, Toosi S. Correlation of the severity of cutaneous rosacea with ocular rosacea. Indian J Dermatol Venereol Leprol. 2009;75:405-406. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 15] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 12. | Alexis AF, Callender VD, Baldwin HE, Desai SR, Rendon MI, Taylor SC. Global epidemiology and clinical spectrum of rosacea, highlighting skin of color: Review and clinical practice experience. J Am Acad Dermatol. 2019;80:1722-1729.e7. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 87] [Article Influence: 14.5] [Reference Citation Analysis (0)] |
| 13. | Al-Dabagh A, Davis SA, McMichael AJ, Feldman SR. Rosacea in skin of color: not a rare diagnosis. Dermatol Online J. 2014;20:13030. [PubMed] |
| 14. | Gupta MA, Gupta AK, Chen SJ, Johnson AM. Comorbidity of rosacea and depression: an analysis of the National Ambulatory Medical Care Survey and National Hospital Ambulatory Care Survey--Outpatient Department data collected by the U.S. National Center for Health Statistics from 1995 to 2002. Br J Dermatol. 2005;153:1176-1181. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 81] [Cited by in RCA: 72] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 15. | Egeberg A, Hansen PR, Gislason GH, Thyssen JP. Patients with Rosacea Have Increased Risk of Depression and Anxiety Disorders: A Danish Nationwide Cohort Study. Dermatology. 2016;232:208-213. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 70] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 16. | Egeberg A, Ashina M, Gaist D, Gislason GH, Thyssen JP. Prevalence and risk of migraine in patients with rosacea: A population-based cohort study. J Am Acad Dermatol. 2017;76:454-458. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 32] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 17. | Wang Z, Xie H, Gong Y, Ouyang Y, Deng F, Tang Y, Li J. Relationship between rosacea and sleep. J Dermatol. 2020;47:592-600. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 18] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 18. | Chen Q, Shi X, Tang Y, Wang B, Xie HF, Shi W, Li J. Association between rosacea and cardiometabolic disease: A systematic review and meta-analysis. J Am Acad Dermatol. 2020;83:1331-1340. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 41] [Article Influence: 8.2] [Reference Citation Analysis (0)] |
| 19. | Zhao S, Wang Y, Mu Y, Yu B, Ye P, Yan X, Li Z, Wei Y, Ambegaonakr BM, Hu D; DYSIS-China Study Investigators. Prevalence of dyslipidaemia in patients treated with lipid-lowering agents in China: results of the DYSlipidemia International Study (DYSIS). Atherosclerosis. 2014;235:463-469. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 75] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 20. | Duman N, Ersoy Evans S, Atakan N. Rosacea and cardiovascular risk factors: a case control study. J Eur Acad Dermatol Venereol. 2014;28:1165-1169. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 77] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 21. | Rainer BM, Fischer AH, Luz Felipe da Silva D, Kang S, Chien AL. Rosacea is associated with chronic systemic diseases in a skin severity-dependent manner: results of a case-control study. J Am Acad Dermatol. 2015;73:604-608. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 89] [Cited by in RCA: 94] [Article Influence: 9.4] [Reference Citation Analysis (0)] |