Published online Jun 16, 2024. doi: 10.12998/wjcc.v12.i17.3235
Revised: April 9, 2024
Accepted: April 19, 2024
Published online: June 16, 2024
Processing time: 99 Days and 7.4 Hours
This reported procedure combines the orthopedic surgical robot with the unil
A 44-year-old patient presented to our hospital. Combining various clinical data, we diagnosed the patient with lumbar disc herniation with radiculopathy, lumbar spondylolisthesis, and lumbar spinal stenosis. We developed a surgical plan of "UBE decompression + UBE-LIF + orthopedic surgery robot-assisted percu
We present an extremely rare case of multiple-segment lumbar decompression and fusion surgery for lumbar disc herniation via robot-assisted UBE and achieved good results. Therefore, the technique is worthy of clinical promotion.
Core Tip: We report a case of multiple-segment lumbar decompression and fusion surgery for lumbar disc herniation via robot-assisted unilateral biportal endoscopy and review the literature. This report provides a reference for spine surgeons to use several advanced technologies for smarter and less invasive treatment and offers new ideas and strategies for the development of digital orthopedics and minimally invasive endoscopy.
- Citation: Liu YD, Xu DF, Deng Q, Zhang YJ, Guo TF, Peng RD, Li JJ. Treatment of lumbar disc herniation with robot combined with unilateral biportal endoscopic technology: A case report. World J Clin Cases 2024; 12(17): 3235-3242
- URL: https://www.wjgnet.com/2307-8960/full/v12/i17/3235.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i17.3235
After preoperative discussion in the department, combined with the patient's current symptoms and relevant medical history, in addition to considering the patient's age and occupation, the traditional open surgery commonly used in the past could help the patient to resume normal activities, but the incision in the operation was large and required extensive stripping of the paravertebral muscles, which to a certain extent affected the postoperative recovery of spinal function and nerves and would have a greater impact on the patient's work and life. At the same time, pedicle screw internal fixation is subjected to tremendous internal pressure, which to a certain extent weakens the muscle support and muscle protection of the already injured spine. Robotic-assisted unilateral dual-channel spinal endoscopic decompression, fusion, and internal fixation do not require stripping of the paravertebral muscles, which is less invasive and largely reduces damage to the patient's musculature and neural structures. In addition, the robotic-assisted vertical installation of pedicle screws facilitates adequate protection of the structure and stability of the vertebral body. At the same time, minimally invasive surgical treatment has less intraoperative bleeding, less patient stress, and higher surgical safety. In addition, the patient and his family requested minimally invasive surgical treatment, so the patient was offered "unilateral biportal endoscopy (UBE) decompression + UBE-lumbar interbody fusion (UBE-LIF) + orthopedic surgery robot-assisted perc
On October 17, 2022, a 44-year-old female employee presented to our hospital with "low back pain with bilateral hip pain and discomfort for 5 months, aggravated for 1 month".
Five months ago, the patient presented with no obvious cause of lumbar pain and discomfort with bilateral hip pain, numbness and discomfort, notably on the right side, and occasionally numbness and discomfort on the dorsal side of the thumb. She did not pay any attention to the symptoms, but after one month, the symptoms worsened and she was hospitalized in a local hospital for more than half a month. After discharge, the above symptoms recurred due to exertion and prolonged walking, but no special treatment was given during this period. The above-mentioned symptoms were aggravated again in January before admission to the hospital, and were slightly relieved after rest. The patient is now sleeping poorly and has normal bowel movements.
The patient's previous health was fair and denied previous underlying disease.
Patient denies history of infectious disease; denies history of surgery, denies history of trauma; patient has 2 daughters, spouse and daughters are in good health. Denies family history of hereditary disease.
The patient had low back pain, restricted movement, positive local percussion pain, positive straight leg raise test, left leg could be raised 70° and positive strengthening test; right leg could be raised 60° and positive strengthening test; positive closed-air jerk test, positive right femoral nerve pull test, bilateral iliopsoas muscle (L2-4), quadriceps muscle (L2-4), anterior tibialis muscle (L4-5), long toe extensor (L4-S1), and gastrocnemius, and hallux valgus (L5-S2) muscle strength grade 4. Bilateral hip pain and numbness were more severe on the right side, and the right Achilles tendon reflex was diminished. The visual analogue scale (VAS) score was 7 (moderate pain).
Hemoglobin 100 g/L, erythrocyte pressure volume 34.40%, erythrocyte mean volume 72.6 fL, erythrocyte mean hem
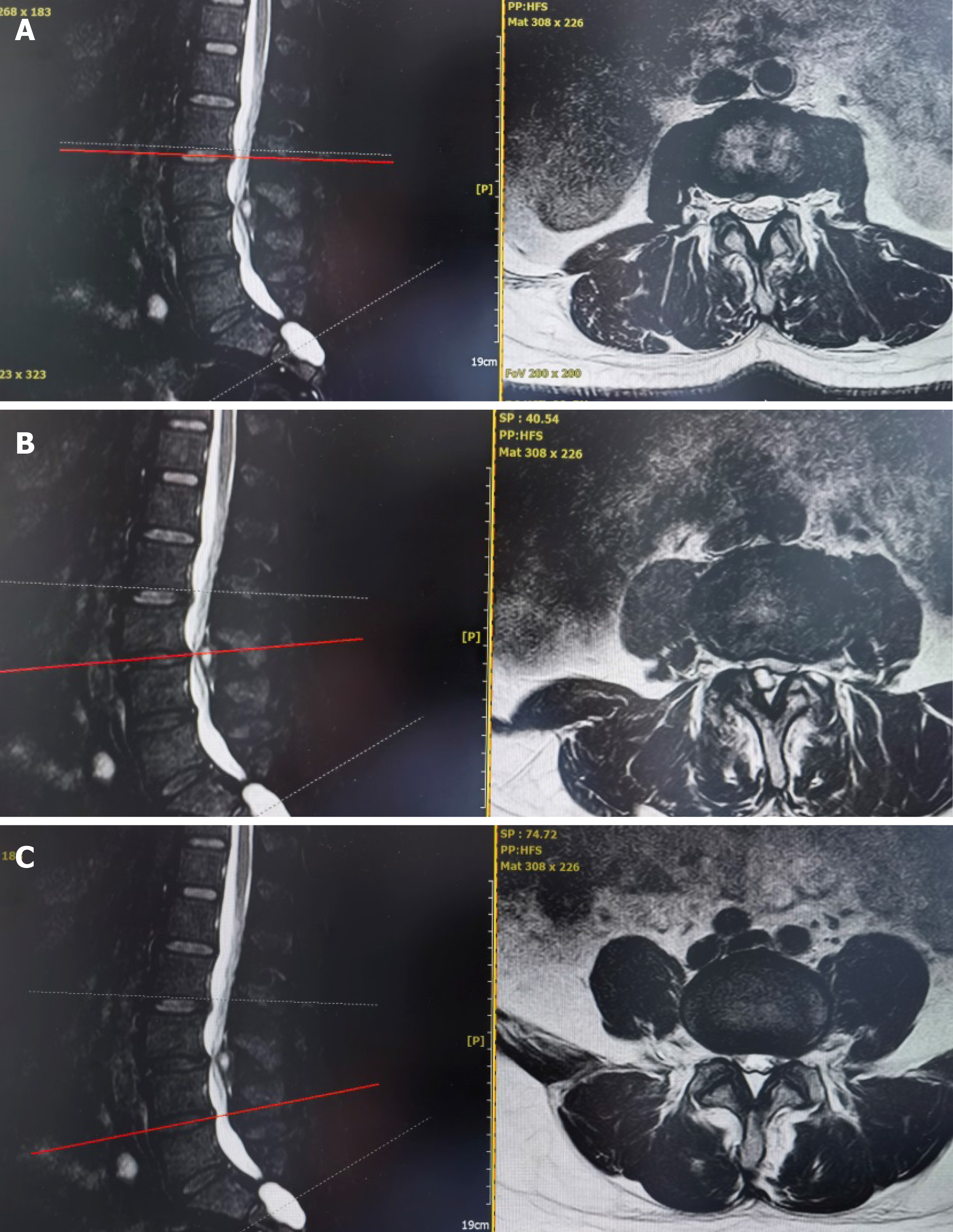
Lumbar spine digital radiography showed that the L3 and 4 vertebrae slipped 1° forward. Computed tomography of the lumbar spine showed that the L2-3 disc was herniated posteriorly to the right; the L3-4 disc was bulging, and the L3 and 4 vertebrae were slipped 1° forward; the spinal canal was narrowed in the same plane. Magnetic resonance imaging of the lumbar spine showed that the L2-3 disc was herniated posteriorly to the right, and the L3-4, L4-5, and L5-S1 discs were deformed and bulging; the L3 vertebral body slipped 1° forward, and the spinal canal was stenosed in the same plane (Figure 1).
Based on the patient's imaging data and his symptoms, we diagnosed the patient with lumbar disc herniation and lumbar spondylolisthesis.
In combination with the patient's clinical symptoms and imaging data, we developed a robot assisted surgery plan for the patient to perform multi levels lumbar decompression and fusion under UBE. The operation process is as follows:
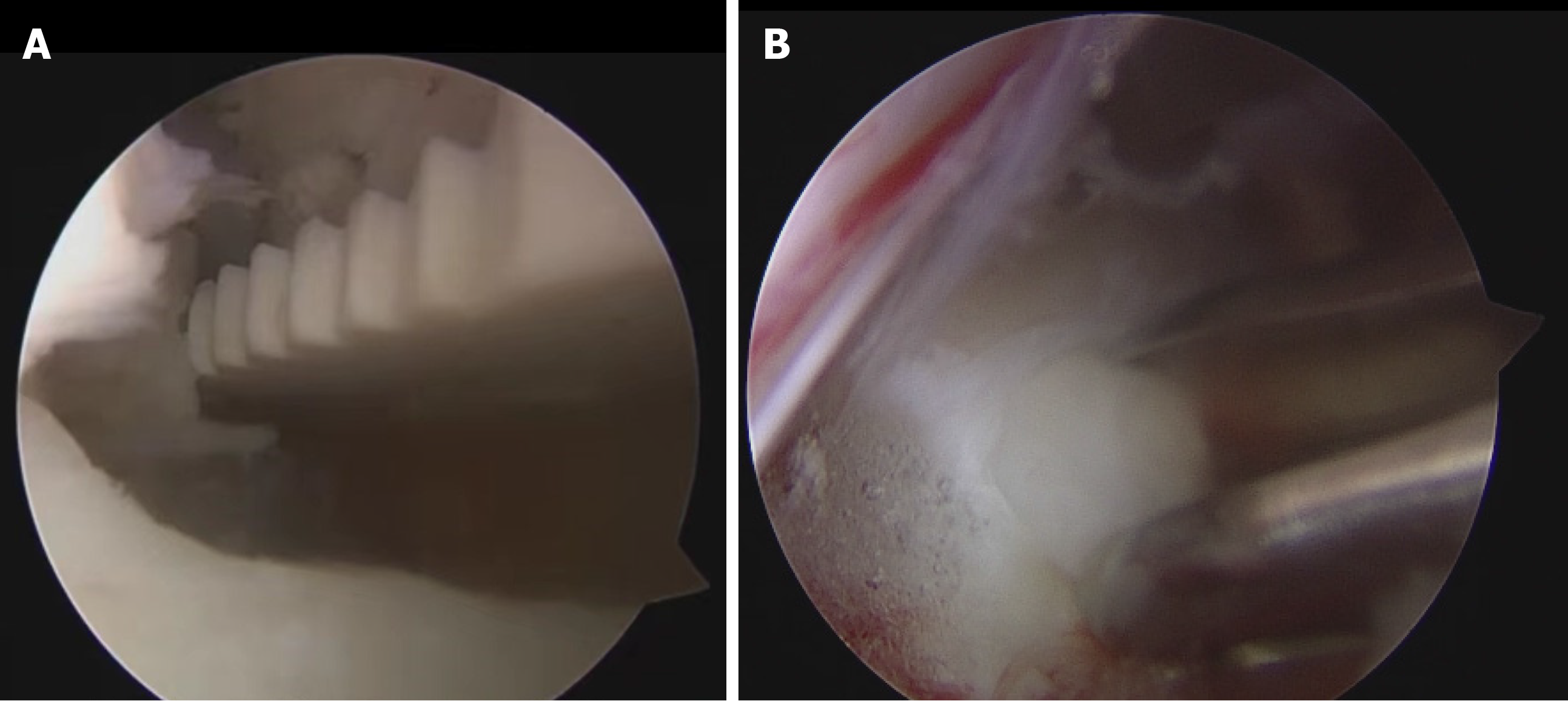
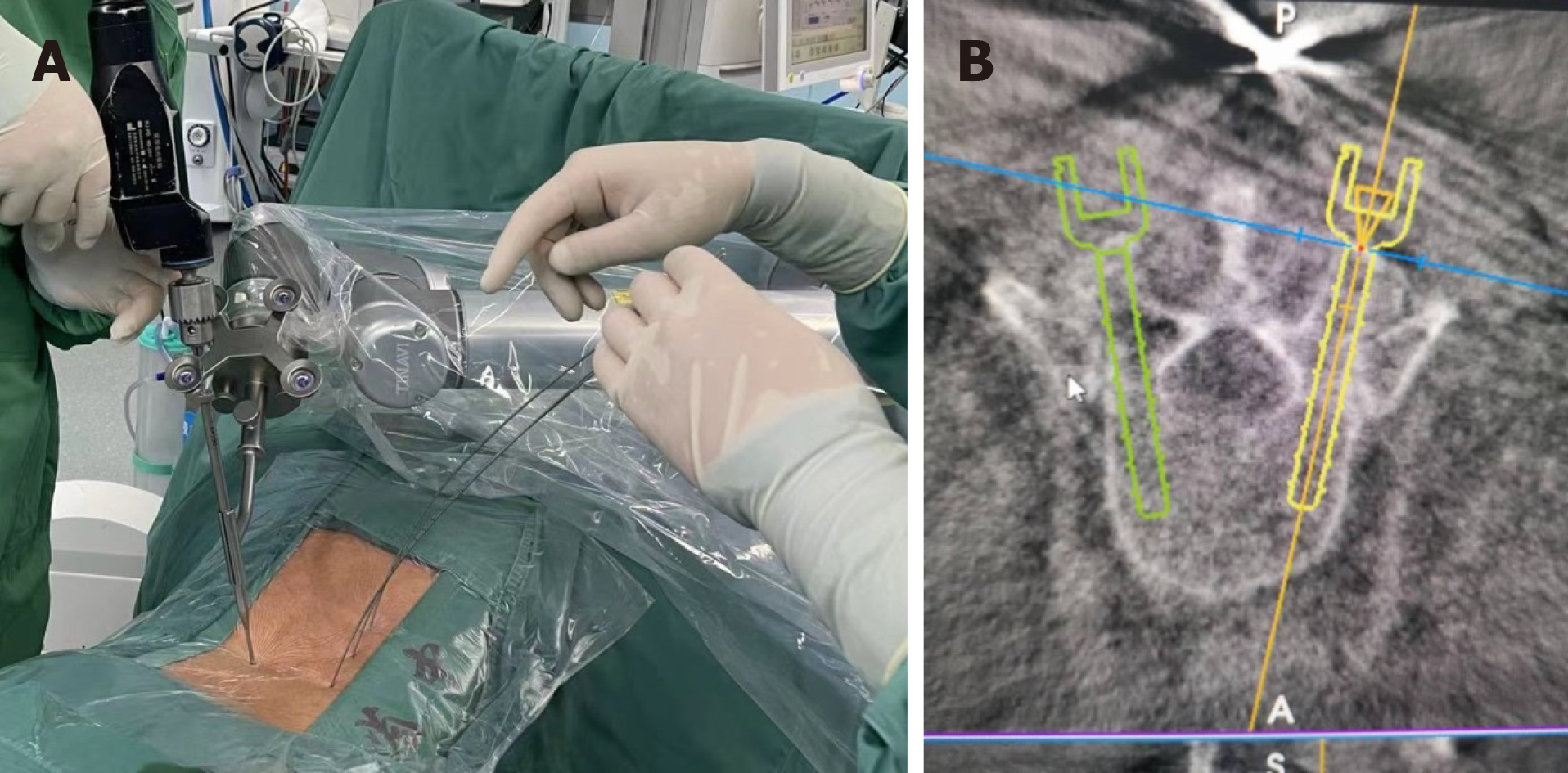
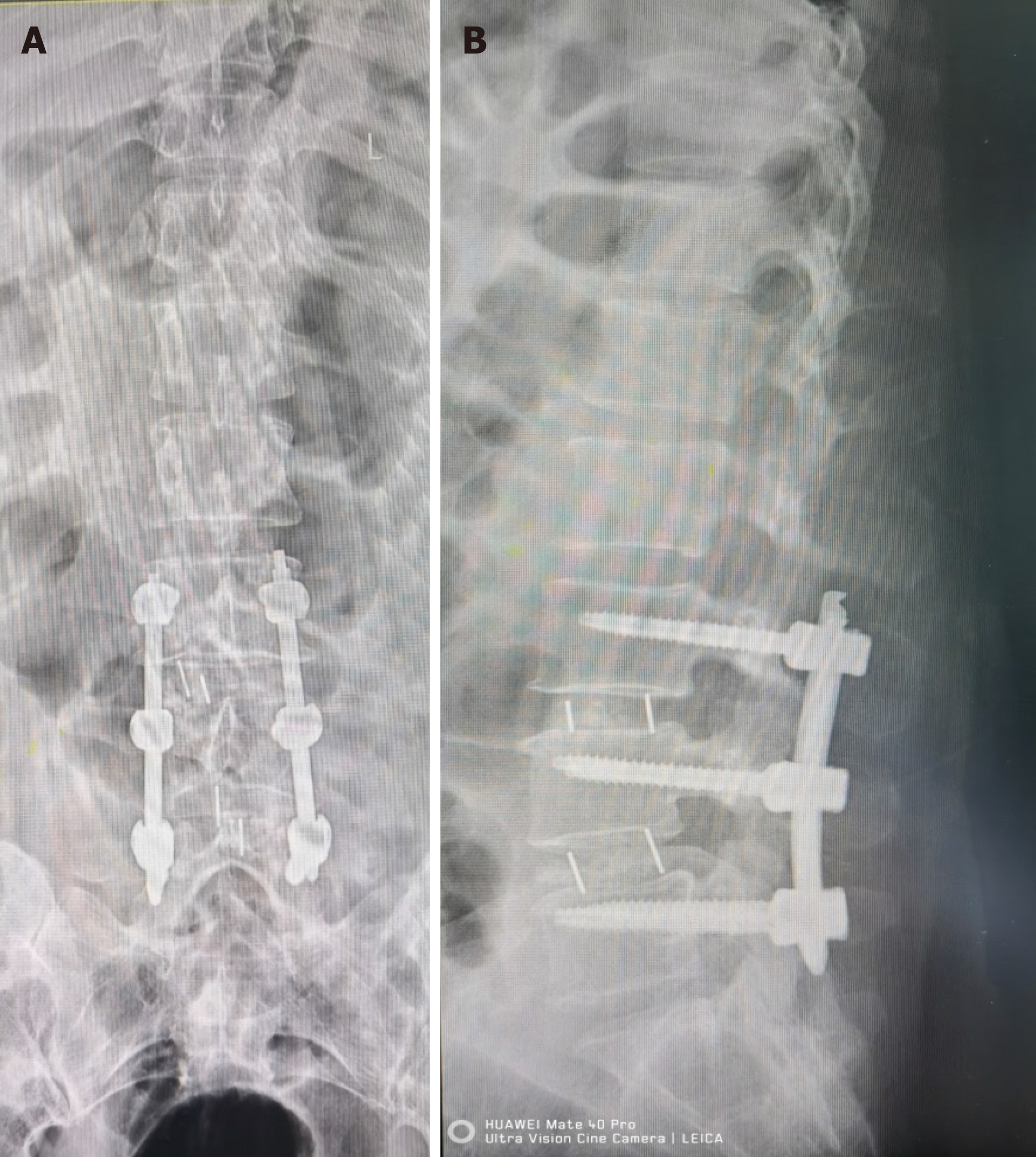
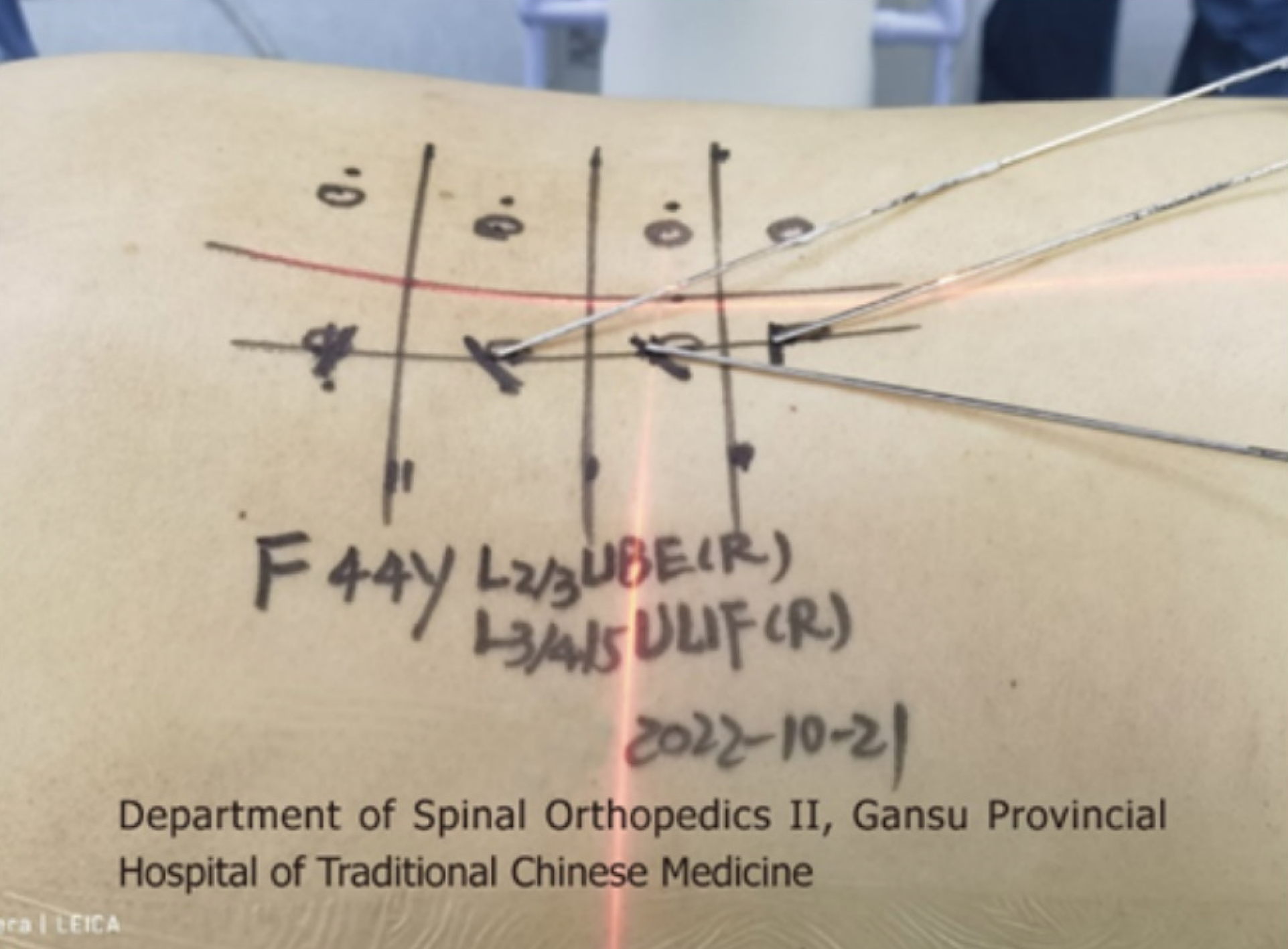
(1) After the general anesthesia takes effect, the patient takes a prone position and places a silica gel prone position support frame on the abdomen. 3D C-arm X-ray machine (SIEMENS, Germany) is used to fluoroscopically locate the three intervertebral space planes L2-3, L3-4 and L4-5, mark the back median line, mark the horizontal line on the body surface at the junction point between the root of spinous process and vertebral lamina of each segment, mark the line on the inner edge of the right pedicle L2-3, and mark the 1.5 cm mark on the head and tail of the line on the inner edge of the pedicle with the horizontal line as the central line as the incision. The operation area was routinely disinfected and sterile towel sheets were laid; (2) Cut the skin about 1cm in each incision, and place the soft tissue expansion tube in the direction of L2-3 intervertebral lamina through the incision. Fluoroscopy confirms that the tip of the expansion tube is located at the right side of L2-3 intervertebral lamina. Adjust the arthroscopic imaging system under the platform until the image is clear, and adjust the white balance. Endoscopy was placed through the head side channel, and the tail side incision was used as the working channel to place the low temperature plasma knife head, stop bleeding, and ablate the tissue. The L2-3 lamina window was continuously flushed with normal saline, and the right lamina window of the patient L2-3 was exposed under the microscope. It was found that the right lamina window of the patient L2-3 was narrow. The lamina window of the patient L2-3 was enlarged with a microscope drill, the ligamentum flavum between the L2-3 lamina was bitten open, and the ligamentum flavum and lamina flavum were bitten laterally and caudally to expand the field of vision and lateral recess, and expose the nerve root and dura mater. During the operation, dura mater and epidural tissue were found to adhere. A nerve hook was used to separate the adhesion, and a nerve examination hook was placed. The nerve root and dura mater were protected inside the nerve retractor. The herniated part of the nucleus pulposus was seen to enter the field of vision. The herniated and loose nucleus pulposus tissues were removed. Under the microscope, the osteotome and the lamina rongeur were used to bite off the lower articular process and part of the upper articular process of the joint segment. There was no obvious stenosis in the recess channels on both sides. Use the disc reamer and curette to scrape off the L3-4 and L4-5 intervertebral disc tissues and upper and lower endplates. After the trial, two intervertebral fusion cages (filled with autologous and allogeneic bone) were implanted at the right side of the L3-4 and L4-5 spaces (Figure 2A). The activity of the nerve root can be explored again, and the compression of the dural sac can be relieved. Again, no residual nucleus pulposus was found on the opposite side and head and tail side. The neurolysis of nerve root was ideal. No active bleeding was observed under microscope. Five mL methylprednisolone was injected around the nerve root, and the cuff hook and endoscope were withdrawn; (3) Install the robot range finder, adjust the robot mechanical arm, scan the three-dimensional images of L3, 4 and 5 vertebrae with the C-arm and send them to the robot navigation system (Beijing Tianzhihang Medical Technology Co., Ltd., China), design the pedicle needle entry point, screw direction and length, install the robot mechanical arm protective sleeve, simulate the robot and fine tune the mechanical arm, and successively implant positioning pins on the L3, 4 and 5 sides of the pedicle, Radi
Postoperative condition: On the third day after operation, the patient's straight leg lifting test was 85° on the left side and 80° on the right side, and the patient could perform ground exercise and functional exercise under the guidance of the doctor. We recommend that patients keep a light diet and take active functional exercise. After completing regular follow-up (days 10, 20, and 30), the patients showed significant improvement in all symptoms and a gradual decrease in VAS scores. Patients had good compliance. Figure 2B shows intraoperative unilateral biportal endoscopy nerve decom
In 1996, Kambin[1] first tried and reported the removal of herniated intervertebral discs using unilateral dual channel endoscopy; In 2017, Heo et al[2] and others named the unilateral dual channel endoscopic technology "UBE" for the first time. Unlike the current mature coaxial single channel percutaneous spinal endoscopy (percutaneous endoscopic lumbar diskectomy and microendoscopic diskectomy), which rely on one channel, UBE technology can work through two independent channels (operation channel and observation channel). The observation channel is used for optical instrument sensing and continuous saline flushing. The operation channel is used for surgical operation. In addition, compared with the disadvantages of single channel endoscopic technology (narrow operation range, limited field of vision, steep learning curve, and the need for specific instruments), UBE has an independent visual operation field of vision, and uses the "polysplius triangle space" and "muscle lamina space" between muscles, bones, and ligaments to create work channels to avoid unnecessary damage to the spine and related structures[3]. At present, the main challenge of UBE is how to establish appropriate liquid flushing, minimize the complications such as dural tear, epidural hematoma, and nerve root injury, and accurately locate the surgical area. The precise puncture location and high stability of orthopedic surgical robots can effectively remedy the above shortcomings. With the continuous development of optical imaging technology and surgical instruments, the diagnosis and treatment spectrum of UBE has also been expanding. UBE technology has not only covered degenerative diseases in the neck, chest, lumbar and other parts, but also is gradually covering the indications of traditional spinal surgery, especially in terms of space occupying in the spinal canal, spinal tuberculosis, vertebral fracture, etc[4].
LIF is a common surgical method for the treatment of lumbar spondylolisthesis or instability. It has experienced a leap forward development from traditional open surgery to minimally invasive surgery. With the rapid development of UBE technology, it is gradually reported at home and abroad that LIF (UBE-LIF) is performed through UBE technology. The clinical effect is worthy of affirmation. In 2017, Heo et al[2] and others successfully applied UBE technology to vertebral body fusion surgery for the first time, called UBE-LIF. Since the 1980s, the conventional open "full decompression of spinal canal combined with interbody bone graft fusion and fixation" has been the golden operation for the treatment of spinal related degenerative diseases. With the development of spinal endoscopy, the traditional open surgery is gradually being replaced by minimally invasive surgery to achieve better results and patient satisfaction. UBE-LIF refers to one of the minimally invasive vertebral body fusion operations that can be performed under unilateral dual channel endoscopy without specific surgical instruments, which can significantly reduce the damage to local normal anatomical structures (such as muscles, ligaments and bones themselves)[5]. A large number of clinical studies have proved that because UBE-LIF technology does not use tubular retractors, it can preserve paravertebral muscles more completely and prevent muscle ischemia, thus achieving satisfactory safe and effective results. With the vigorous development of artificial intelligence navigation technology, the combination of UBE-LIF and robot assisted nail positioning technology can realize the joint application of advanced technologies, further optimize the efficacy of fusion surgery, and improve the accuracy, minimally invasive, intelligence and low radiation of spinal surgery[6].
In 1992, the world's first spinal robot assisted surgery was completed by Lavallée et al[7] at the Grenoble Medical College in France, marking a new stage in the surgical treatment of spinal diseases. Pedicle screw fixation is an important step in vertebral fusion. At present, orthopedic surgical robots are mainly used in spinal surgery for preoperative planning, navigation and positioning, and screw implantation. Compared with manual nailing, robot assisted nailing can effectively improve the accuracy of nailing, reduce the radiation exposure risk of patients and operators, and reduce vascular and neural damage. At the same time, the robot system makes the surgery more stereoscopic in vision, and can reconstruct real-time nail placement effect and 3D image visualization from multiple angles, so that the operator can participate in the nail placement process more clearly and intuitively[8]. Cui et al[9] and other researchers found that the number of class A screws (Rampersaud classification) in robot assisted nail placement group was significantly higher than that in conventional surgery group. The intraoperative blood loss, postoperative drainage volume, hospital stay, rehabilitation time, and VAS score 3 d after surgery of robot assisted MIS-TLIF were lower than those of the traditional operation group. The "Tianji" surgical robot used in the operation is an intelligent navigation and positioning system based on 3D imaging technology for space simulation and path planning. The system is characterized by active positioning and man-machine cooperation, and accurate implantation of percutaneous screws is achieved according to the preoperative planning path, thus improving the surgical effect[10].
This report combines the orthopedic surgical robot with UBE-LIF, completes minimally invasive decompression and fusion of the diseased segment using UBE's wide observation field and operation space, and completes percutaneous pedicle screw implantation using the intelligence and accuracy of the orthopedic surgical robot. The progressiveness of this operation lies in the superposition of the advantages of two new technologies. Under the monitoring of the imaging instrument, the purpose of the treatment is to achieve the maximum effect in the way of maximum minimally invasive and maximum accuracy, so as to maximize the benefits of patients. At present, there are few reports on the application of intelligent navigation robots in UBE endoscopic fusion. The perfect combination of doctors, robots and spinal endoscopes is the embodiment of intelligence and minimally invasive spinal surgery and the key to solving a series of spinal surgery problems. The clinical application of UBE-LIF assisted by orthopedic surgical robot is a profound change to the concept of large wound and deep wound cavity of conventional vertebral fusion surgery, which can achieve the maximum effect at a smaller cost, and conforms to the concept of minimally invasive surgery, intelligent surgery and rapid rehabilitation surgery, as well as the development trend of accuracy and safety[11]. However, there are still problems in the joint application of these two new technologies. For example, problems such as slip error, long learning period and long operation time still need to be solved. The author believes that, through continuous research and exploration, the orthopaedic surgical robot assisted UBE-LIF surgery will lead the development of spinal surgery towards a more intelligent and minimally invasive direction, and also provide new ideas and strategies for the development of digital orthopaedics and minimally invasive endoscopy.
Through literature search, this is the first report of multi level lumbar decompression and fusion under robot assisted unilateral dual channel spinal endoscopy at home and abroad.
We provide an extremely rare case of Treatment of lumbar disc herniation with multi segment lumbar decompression and fusion surgery under robot assisted UBE and achieved good results. Therefore, the technique is worthy of clinical promotion.
| 1. | Kambin P. Diagnostic and therapeutic spinal arthroscopy. Neurosurg Clin N Am. 1996;7:65-76. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 15] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 2. | Heo DH, Son SK, Eum JH, Park CK. Fully endoscopic lumbar interbody fusion using a percutaneous unilateral biportal endoscopic technique: technical note and preliminary clinical results. Neurosurg Focus. 2017;43:E8. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 101] [Cited by in RCA: 182] [Article Influence: 26.0] [Reference Citation Analysis (0)] |
| 3. | Kang MS, Heo DH, Kim HB, Chung HT. Biportal Endoscopic Technique for Transforaminal Lumbar Interbody Fusion: Review of Current Research. Int J Spine Surg. 2021;15:S84-S92. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 30] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 4. | Gatam AR, Gatam L, Mahadhipta H, Ajiantoro A, Luthfi O, Aprilya D. Unilateral Biportal Endoscopic Lumbar Interbody Fusion: A Technical Note and an Outcome Comparison with the Conventional Minimally Invasive Fusion. Orthop Res Rev. 2021;13:229-239. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 21] [Reference Citation Analysis (0)] |
| 5. | Kim JE, Choi DJ. Biportal Endoscopic Transforaminal Lumbar Interbody Fusion with Arthroscopy. Clin Orthop Surg. 2018;10:248-252. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 49] [Cited by in RCA: 90] [Article Influence: 12.9] [Reference Citation Analysis (0)] |
| 6. | Park MK, Park SA, Son SK, Park WW, Choi SH. Clinical and radiological outcomes of unilateral biportal endoscopic lumbar interbody fusion (ULIF) compared with conventional posterior lumbar interbody fusion (PLIF): 1-year follow-up. Neurosurg Rev. 2019;42:753-761. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 70] [Article Influence: 11.7] [Reference Citation Analysis (0)] |
| 7. | Lavallée S, Sautot P, Troccaz J, Cinquin P, Merloz P. Computer-assisted spine surgery: a technique for accurate transpedicular screw fixation using CT data and a 3-D optical localizer. J Image Guid Surg. 1995;1:65-73. [PubMed] [DOI] [Full Text] |
| 8. | Ghasem A, Sharma A, Greif DN, Alam M, Maaieh MA. The Arrival of Robotics in Spine Surgery: A Review of the Literature. Spine (Phila Pa 1976). 2018;43:1670-1677. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 112] [Cited by in RCA: 139] [Article Influence: 19.9] [Reference Citation Analysis (0)] |
| 9. | Cui GY, Han XG, Wei Y, Liu YJ, He D, Sun YQ, Liu B, Tian W. Robot-Assisted Minimally Invasive Transforaminal Lumbar Interbody Fusion in the Treatment of Lumbar Spondylolisthesis. Orthop Surg. 2021;13:1960-1968. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 47] [Article Influence: 11.8] [Reference Citation Analysis (0)] |
| 10. | Verhey JT, Haglin JM, Verhey EM, Hartigan DE. Virtual, augmented, and mixed reality applications in orthopedic surgery. Int J Med Robot. 2020;16:e2067. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 108] [Article Influence: 21.6] [Reference Citation Analysis (0)] |
| 11. | Akazawa T, Torii Y, Ueno J, Umehara T, Iinuma M, Yoshida A, Tomochika K, Ohtori S, Niki H. Accuracy of computer-assisted pedicle screw placement for adolescent idiopathic scoliosis: a comparison between robotics and navigation. Eur Spine J. 2023;32:651-658. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 14] [Reference Citation Analysis (0)] |