Published online Jun 16, 2024. doi: 10.12998/wjcc.v12.i17.3194
Revised: April 20, 2024
Accepted: April 28, 2024
Published online: June 16, 2024
Processing time: 120 Days and 0 Hours
Drug-eluting stents (DES) are used to treat lower extremity arterial disease. During DES treatment, aneurysmal degeneration occasionally occurs, especially with fluoropolymer-based DES. However, the incidence of pseudoaneurysms after DES placement is rarely reported in the lower extremity region, although there have been several reports on pseudoaneurysm formation after DES pla-cement in the coronary artery region.
We report the case of a 64-year-old man who presented with fever and pain in his left hand after dialysis. Bacteremia was diagnosed by blood culture, and after admission, he developed pain on the medial side of the right thigh. A pseudoaneurysm was observed in the right superficial femoral artery (SFA) at the proximal end of a previously placed DES. The bacteremia was thought to have been caused by a pseudoaneurysm of the left superficial brachial artery, and the pseudoaneurysm of the left superficial brachial artery was removed after antibiotic treat
Although pseudoaneurysm after DES placement in the lower extremity region is rare, it must be considered in patients with bacteremia.
Core Tip: We report a relatively rare case of pseudoaneurysm formation after the placement of a drug-eluting stent in the superficial femoral artery. This pseudoaneurysm was discovered after the development of bacteremia and removed because of suspicion of an infected aneurysm. This report describes an uncommon presentation of pseudoaneurysm, which suggests that pseudoaneurysm should be considered as a differential diagnosis along with degenerative aneurysm in patients with bacteremia after placement of a drug-eluting stent.
- Citation: Akai T, Ninomiya S, Kaneko T. Superficial femoral artery pseudoaneurysm at implantation site of drug eluting stent discovered due to bacteremia: A case report. World J Clin Cases 2024; 12(17): 3194-3199
- URL: https://www.wjgnet.com/2307-8960/full/v12/i17/3194.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i17.3194
Endovascular treatment has been increasingly considered for the management of lower extremity arterial disease (LEAD)[1]. However, optimal treatment strategies remain subject to debate and may vary based on factors such as lesion location and patient comorbidities. The choice between endovascular repair and other interventions is typically made on a case-by-case basis. Drug-eluting stents (DES) have been categorized as appropriate strategies for the endovascular treatment of superficial femoral and popliteal arteries according to a Report of the American College of Cardiology Appropriate Use Criteria Task Force[2]. Meanwhile, in Global Vascular Guidelines[3], it is concluded that there are few high-quality comparative data to guide the choice of a specific endovascular approach in chronic limb-threatening ischemia. ELUVIA™, fluoropolymer-based DES (FP-DES), has shown a good patency rate in the IMPERIAL trial[4], although a post hoc core laboratory review of ultrasonographic images from the IMPERIAL trial revealed aneurysmal degeneration in 1.9% (6/309) of patients in the FP-DES group. In a single-center retrospective study, degenerative aneurysm formation with flow was reported in 1.5% (2/130) of the patients after DES placement in the arterial region of the lower extremities[5]. Conversely, pseudoaneurysm formation after DES placement is rarely reported in the lower-extremity region, although there are several studies on the incidence of pseudoaneurysms after DES placement in the coronary arteries[6-9].
Herein, we report an unusual case of a pseudoaneurysm in the right superficial femoral artery (SFA) at the site of placement of a DES, which was discovered owing to infection and successfully resected.
A 64-year-old man presented to the emergency department with a fever of 38.9 °C and pain in his left hand.
The patient had undergone dialysis the previous day, following which he experienced chills, and developed a fever and pain in the left hand the next morning. Bacteremia was diagnosed by blood culture, and the patient was admitted to our hospital. After admission, the patient complained of pain on the medial side of his right thigh.
The patient had no history of smoking or allergies. Eight years prior, he was diagnosed with chronic kidney disease. Furthermore, 5 years ago, he was diagnosed with dilated cardiomyopathy, and treatment was started at the cardiology department. Four years prior, the left brachial artery was made superficial, and dialysis was introduced. One year ago, two DES: EluviaTM 7.0 mm × 120 mm, EluviaTM 6.0 mm × 120 mm) were placed in the right SFA for right LEAD.
The patient had no significant personal or family history.
He had multiple painful purpuras on his left fingertips that were likely Osler nodes.
Gram positive cocci were positive in 4 × 4 blood cultures, and methicillin-susceptible Staphylococcus aureus was detected. Blood tests showed increased white blood cells count (9.1 × 109/L, with 92.2% neutrophils) and C-reactive protein level (4.42 × 104 μg/dL), and decreased hemoglobin level (89 g/L).
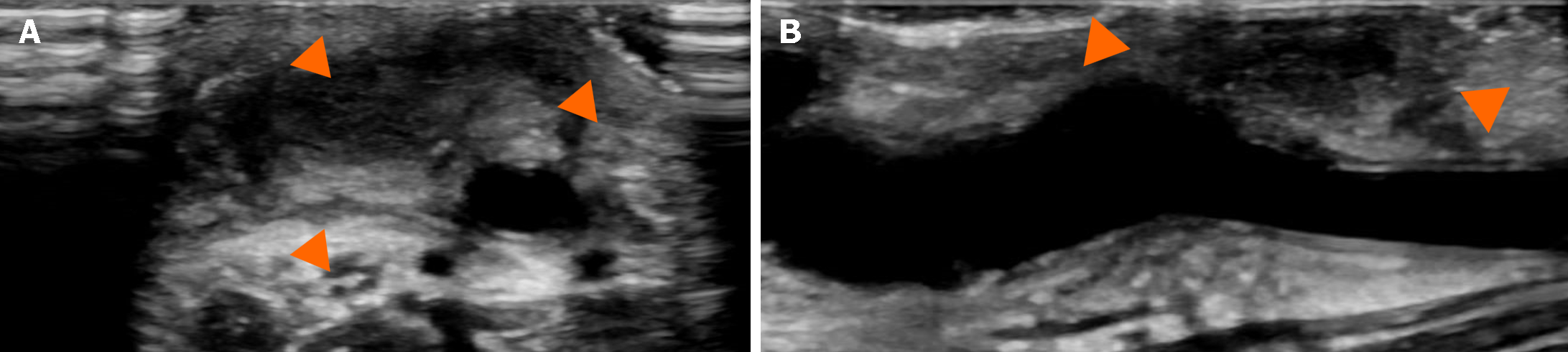
Since transthoracic cardiac ultrasound showed no vegetation, infective endocarditis was ruled out. A pseudoaneurysm was observed in the left superficial brachial artery using ultrasonography (Figure 1).
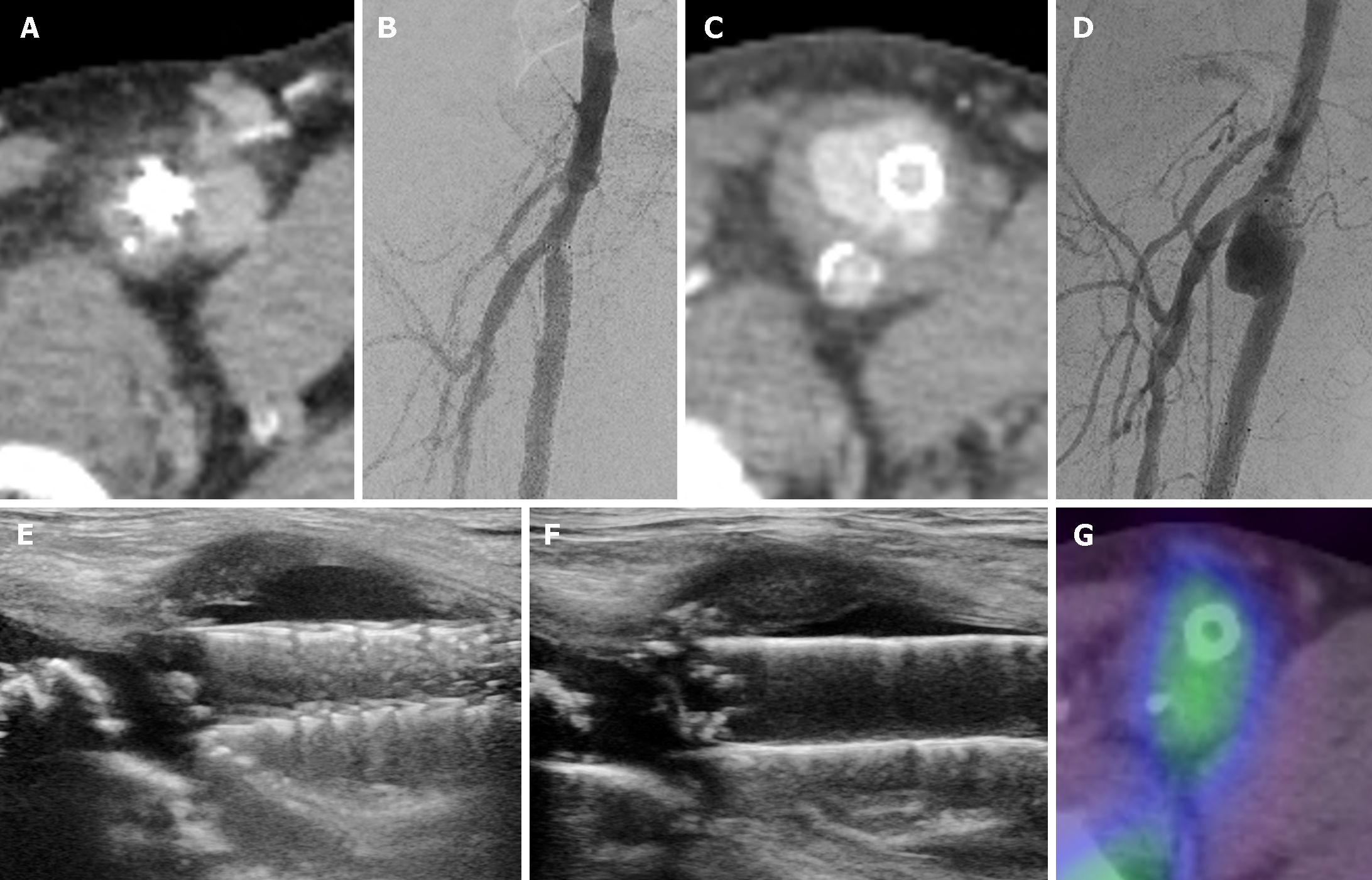
The area proximal to where the DES was placed in the right SFA was also dilated. Although it was only mildly dilated at the time of admission (Figure 2A and B), it showed marked expansion, especially from the third week to the seventh week of admission (Figure 2C and D). Subsequently, its expansion rate slowed down (Figure 2E and F). Gallium scintigraphy performed 3 wk after admission revealed only slight accumulation in the aneurysm (Figure 2G).
The final diagnosis was a pseudoaneurysm of the SFA at the proximal edge of the DES, which was suspected to be an infectious aneurysm.
The patient was treated with cefazolin (2 g/day via intravenous infusion); the aneurysm grew rapidly for a period of time, but the inflammatory response temporarily subsided 3 wk after admission. However, the inflammatory response relapsed 5 to 6 wk after admission. A pseudoaneurysm was detected in the left superficial brachial artery, which was resected. The bacterial culture of the excised aneurysm was negative, and inflammatory indicators improved after surgery. Infection was suspected due to expansion of the proximal part of the DES implantation site. The patient was then discharged 3 months after admission on oral antibiotics (cephalexin, 250 mg twice a day). During an outpatient visit, although the infection was found to be controlled, the aneurysm continued to expand slowly; consequently, we decided to perform surgery 7 months after initial admission.
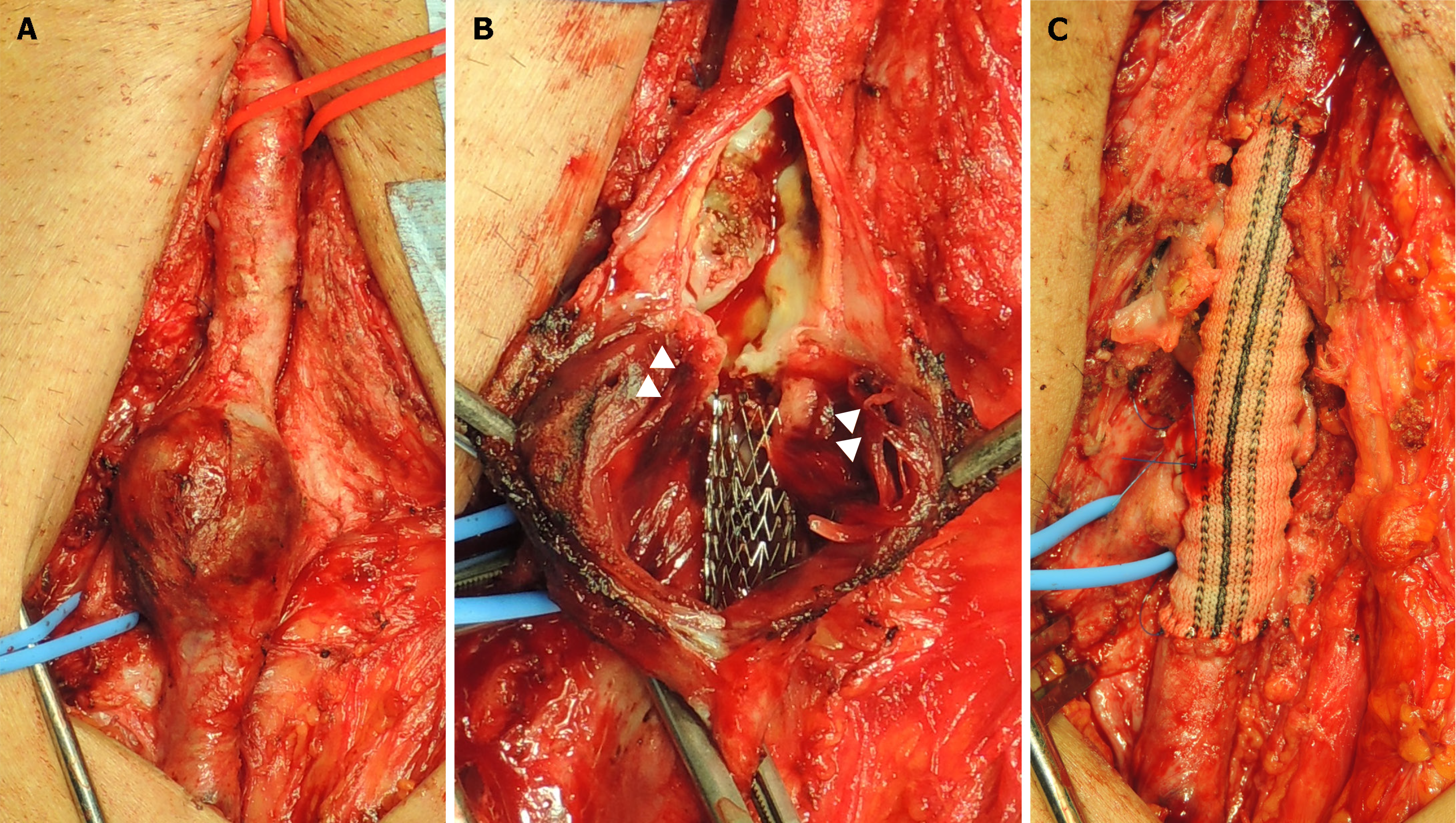
Surgery was performed under general anesthesia. Incisions were made in the right groin, right common femoral artery (CFA), and deep femoral artery (DFA), and the SFA was isolated (Figure 3A). Each blood vessel was clamped, and the aneurysm was incised. Although the stent was exposed inside the crumbled blood vessel wall, no abscesses were observed, including those in the surrounding area (Figure 3B). After partially dissecting the stent, a rifampicin-soaked 8 mm Gelsoft Plus™ graft was implanted from the right CFA to the right SFA. The right DFA was anastomosed side to end to the graft (Figure 3C). The excised aneurysm contained no arterial wall components and was a pseudoaneurysm. The bacterial culture of the excised aneurysm was negative.
The postoperative course was uneventful, and the patient was discharged on the sixth postoperative day. After discharge, oral antibiotics (cephalexin, 250 mg twice a day) were continued up to the present time. For 2 years after surgery, no recurrent infection or aneurysm was observed.
There are several reports of pseudoaneurysm formation after DES placement in coronary arteries[6-9]. The underlying mechanisms are thought to be vascular injury during percutaneous coronary intervention and prevention or delay of vascular healing by the eluted drug, which may be caused by inhibition of neointimal hyperplasia and induction of hypersensitivity reactions in the coronary artery endothelium[9,10]. Degenerative aneurysm formation is known to occur in the lower extremity region, especially after FP-DES placement[5,11-13]. In a multicenter prospective study, Iida et al[12] reported that aneurysmal degeneration, defined as a dark halo around the stenting site on duplex ultrasonography, was found in 16.8% of the limbs. In our case, the aneurysm was discovered as a result of infection and rapidly enlarged over a period of 1-2 months. The excised aneurysm was diagnosed as a pseudoaneurysm, which formed at the proximal end of the stent. The mechanism was thought to be ulceration of the intima due to the stent edge and infection of the area where healing was delayed by paclitaxel. To the best of our knowledge, our case is the first time that pseudoaneurysm formation after DES placement in the lower-extremity region will be reported in the literature. Indeed, a search performed in a PubMed Medline database using the following combination of keywords: “pseudoaneurysm” AND “drug-eluting stent” AND “peripheral” OR “limb” OR “extremity” retrieved no results. In a single-center FP-DES registry for long femoropopliteal lesions after standard balloon angioplasty failure, Bisdas et al[13] reported that aneurysm formation occurred in 8.1% (5/62) of the patients and one of them presented with clinical worsening caused by stent occlusion. Currently, the treatment and prognosis of aneurysmal degeneration are unclear, and patients are carefully monitored. However, since pseudoaneurysms carry a risk of rupture, it is important to diagnose and differentiate between pseudoaneurysms and aneurysmal degeneration. Although the incidence of pseudoaneurysms is currently unknown, physicians should monitor any formation of aneurysms after DES placement during outpatient follow-up, especially in patients with diabetes, those undergoing dialysis (as in this case), and those undergoing dental treatments that pose a risk of bacteremia.
In this case, a pseudoaneurysm of the SFA was discovered following an infection. Osler’s nodes were observed on the left fingertips, and it seems highly likely that the pseudoaneurysm of the left superficial brachial artery was the original source of bacteremia. Although the pseudoaneurysm in the SFA itself may not be the source of infection, we cannot rule out an infected aneurysm. When treating an infected aneurysm in the lower leg in the same manner as that of the aorta[14,15], the infection must be controlled first by conservative treatment with antibiotics. However, in case a pseudoaneurysm is suspected, careful observation and determination of the timing of treatment are necessary.
Several treatment methods may be considered for pseudoaneurysms of the lower leg. Although not applicable in this case, thrombin injection may be considered for cases where the neck of the aneurysm is narrow, such as a pseudoaneurysm caused by an arterial puncture[16]. Other options include endovascular treatment with a covered stent[17], embolization[18], or a combination of these[19]. In this case, we chose to surgically excise the aneurysm because the DFA bifurcation was close and there was a possibility of an infected aneurysm. Depending on the location of the aneurysm, the aneurysm may be removed alone, although revascularization is necessary at locations related to the SFA and DFA, as in the present case. If the infection is poorly controlled, methods such as non-anatomical reconstruction followed by resection of the aneurysm or allogeneic vascular grafting may be necessary. However, if the infection is under control, as in this case, in situ reconstruction may be sufficient. If the entire stent is thought to be infected, complete removal should be considered, although the indications should be carefully considered because of the high surgical invasiveness.
We report a case of resection of a femoral arterial pseudoaneurysm at a DES-implanted site that was discovered due to bacteremia, thought to be caused by an infection of a superficial brachial arterial pseudoaneurysm. The mechanism of pseudoaneurysm formation in this case may differ from that of degenerative aneurysm formation after DES placement, which has been previously reported. If bacteremia occurs after DES placement, the possibilities of subsequent stent infection and pseudoaneurysm formation must be considered.
| 1. | Stavroulakis K, Borowski M, Torsello G, Bisdas T; CRITISCH Collaborators. One-Year Results of First-Line Treatment Strategies in Patients With Critical Limb Ischemia (CRITISCH Registry). J Endovasc Ther. 2018;25:320-329. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 47] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 2. | Bailey SR, Beckman JA, Dao TD, Misra S, Sobieszczyk PS, White CJ, Wann LS, Bailey SR, Dao T, Aronow HD, Fazel R, Gornik HL, Gray BH, Halperin JL, Hirsch AT, Jaff MR, Krishnamurthy V, Parikh SA, Reed AB, Shamoun F, Shugart RE, Yucel EK. ACC/AHA/SCAI/SIR/SVM 2018 Appropriate Use Criteria for Peripheral Artery Intervention: A Report of the American College of Cardiology Appropriate Use Criteria Task Force, American Heart Association, Society for Cardiovascular Angiography and Interventions, Society of Interventional Radiology, and Society for Vascular Medicine. J Am Coll Cardiol. 2019;73:214-237. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 130] [Cited by in RCA: 124] [Article Influence: 20.7] [Reference Citation Analysis (0)] |
| 3. | Conte MS, Bradbury AW, Kolh P, White JV, Dick F, Fitridge R, Mills JL, Ricco JB, Suresh KR, Murad MH, Aboyans V, Aksoy M, Alexandrescu VA, Armstrong D, Azuma N, Belch J, Bergoeing M, Bjorck M, Chakfé N, Cheng S, Dawson J, Debus ES, Dueck A, Duval S, Eckstein HH, Ferraresi R, Gambhir R, Gargiulo M, Geraghty P, Goode S, Gray B, Guo W, Gupta PC, Hinchliffe R, Jetty P, Komori K, Lavery L, Liang W, Lookstein R, Menard M, Misra S, Miyata T, Moneta G, Munoa Prado JA, Munoz A, Paolini JE, Patel M, Pomposelli F, Powell R, Robless P, Rogers L, Schanzer A, Schneider P, Taylor S, De Ceniga MV, Veller M, Vermassen F, Wang J, Wang S; GVG Writing Group for the Joint Guidelines of the Society for Vascular Surgery (SVS), European Society for Vascular Surgery (ESVS), and World Federation of Vascular Societies (WFVS). Global Vascular Guidelines on the Management of Chronic Limb-Threatening Ischemia. Eur J Vasc Endovasc Surg. 2019;58:S1-S109.e33. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 816] [Cited by in RCA: 923] [Article Influence: 153.8] [Reference Citation Analysis (0)] |
| 4. | Gray WA, Keirse K, Soga Y, Benko A, Babaev A, Yokoi Y, Schroeder H, Prem JT, Holden A, Popma J, Jaff MR, Diaz-Cartelle J, Müller-Hülsbeck S; IMPERIAL investigators. A polymer-coated, paclitaxel-eluting stent (Eluvia) versus a polymer-free, paclitaxel-coated stent (Zilver PTX) for endovascular femoropopliteal intervention (IMPERIAL): a randomised, non-inferiority trial. Lancet. 2018;392:1541-1551. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 147] [Cited by in RCA: 214] [Article Influence: 30.6] [Reference Citation Analysis (0)] |
| 5. | Stavroulakis K, Torsello G, Bosiers M, Argyriou A, Tsilimparis N, Bisdas T. 2-Year Outcomes of the Eluvia Drug-Eluting Stent for the Treatment of Complex Femoropopliteal Lesions. JACC Cardiovasc Interv. 2021;14:692-701. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 48] [Article Influence: 12.0] [Reference Citation Analysis (0)] |
| 6. | Namazi MH, Khani M, Faghihi Langroudi T, Abedi F, Tabary M, Khaheshi I. Coronary pseudoaneurysm 1 week after complex percutaneous coronary intervention with drug-eluting stent. Clin Case Rep. 2020;8:1296-1298. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 7. | Reddy S, Rao K R, Mahant TS, Goel S, Cheluvashetty SB. Unusual Presentation of a Rapidly Progressive Coronary Artery Pseudoaneurysm after Drug Eluting Stent Placement. Cureus. 2021;13:e13305. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 8. | Gersch S, Baraki H, Toischer K. Progression and interventional therapy of a coronary pseudoaneurysm: a case report. Eur Heart J Case Rep. 2023;7:ytac478. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 9. | Sharma R, Ruia AV. A case report of pseudoaneurysm of coronary artery within a month of percutaneous coronary intervention. Eur Heart J Case Rep. 2022;6:ytac175. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 10. | Joner M, Finn AV, Farb A, Mont EK, Kolodgie FD, Ladich E, Kutys R, Skorija K, Gold HK, Virmani R. Pathology of drug-eluting stents in humans: delayed healing and late thrombotic risk. J Am Coll Cardiol. 2006;48:193-202. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2103] [Cited by in RCA: 2119] [Article Influence: 111.5] [Reference Citation Analysis (0)] |
| 11. | Diamantopoulos A, Gupta Y, Zayed H, Katsanos K. Paclitaxel-coated balloons and aneurysm formation in peripheral vessels. J Vasc Surg. 2015;62:1320-1322. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 13] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 12. | Iida O, Takahara M, Soga Y, Yamaoka T, Fujihara M, Kawasaki D, Ichihashi S, Kozuki A, Nanto S, Sakata Y, Mano T; CAPSICUM Investigators. 1-Year Outcomes of Fluoropolymer-Based Drug-Eluting Stent in Femoropopliteal Practice: Predictors of Restenosis and Aneurysmal Degeneration. JACC Cardiovasc Interv. 2022;15:630-638. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 70] [Article Influence: 23.3] [Reference Citation Analysis (0)] |
| 13. | Bisdas T, Beropoulis E, Argyriou A, Torsello G, Stavroulakis K. 1-Year All-Comers Analysis of the Eluvia Drug-Eluting Stent for Long Femoropopliteal Lesions After Suboptimal Angioplasty. JACC Cardiovasc Interv. 2018;11:957-966. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 76] [Article Influence: 12.7] [Reference Citation Analysis (0)] |
| 14. | Luo CM, Chan CY, Chen YS, Wang SS, Chi NH, Wu IH. Long-term Outcome of Endovascular Treatment for Mycotic Aortic Aneurysm. Eur J Vasc Endovasc Surg. 2017;54:464-471. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 52] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 15. | Sugimoto M, Banno H, Idetsu A, Matsushita M, Ikezawa T, Komori K. Surgical experience of 13 infected infrarenal aortoiliac aneurysms: preoperative control of septic condition determines early outcome. Surgery. 2011;149:699-704. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 24] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 16. | Mishra A, Rao A, Pimpalwar Y. Ultrasound Guided Percutaneous Injection of Thrombin: Effective Technique for Treatment of Iatrogenic Femoral Pseudoaneurysms. J Clin Diagn Res. 2017;11:TC04-TC06. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 11] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 17. | Baldwin D, Mashbari H, Chow KL, Sarhan M. Ruptured Superficial Femoral Artery Anastomotic Pseudoaneurysm after 30 Years. Case Rep Vasc Med. 2019;2019:1679214. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 18. | Watanabe S, Kanazawa R, Uchida T, Higashida T, Yamazaki K, Kono T. Endovascular Embolization of Femoral Pseudoaneurysm Associated with Therapeutic and Diagnostic Neuroendovascular Procedures. J Neuroendovasc Ther. 2023;17:8-14. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 19. | Mahjoob MP, Khaheshi I, Naderian M. Stent-assisted coiling of large common femoral artery pseudoaneurysm following coronary artery catheterization: an uncommon and novel approach. Rom J Intern Med. 2017;55:57-59. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |