Published online Jun 16, 2024. doi: 10.12998/wjcc.v12.i17.3151
Revised: April 11, 2024
Accepted: April 22, 2024
Published online: June 16, 2024
Processing time: 140 Days and 15 Hours
While diverticular disease is prevalent in the West, the formation of giant colonic diverticula is rare. To date, approximately 200 cases have been reported, with only a handful treated surgically using a minimally invasive approach. Furthermore, the natural history of giant colonic diverticula is not well documented.
This report describes the case of a 66-year-old man who developed a giant colonic diverticulum with primary symptoms including dull and chronic pain in the right lower quadrant at presentation. The patient had undergone several computed to
This rare case demonstrates the natural history of giant colonic diverticulum formation and supports the feasibility of robot-assisted surgery.
Core Tip: Giant colonic diverticula are a rare complication of diverticular disease. Although the symptoms may sometimes be indolent, the present case suggests that they may continue to worsen if managed conservatively. In appropriate patients, a minimally invasive approach is feasible and can lead to enhanced postoperative recovery.
- Citation: Bachelani AM. Natural history and surgical treatment of a giant colonic diverticulum: A case report. World J Clin Cases 2024; 12(17): 3151-3155
- URL: https://www.wjgnet.com/2307-8960/full/v12/i17/3151.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i17.3151
Diverticular disease remains prevalent in the West, affecting approximately 50% of patients by the age of 50 years. Common complications of this condition include acute and perforated diverticulitis, large bowel obstruction, and he
A 66-year-old male presented with chronic right lower quadrant abdominal pain.
The patient’s symptoms were chronic abdominal pain localized to the right lower quadrant and had been present for approximately 2 years. A surgical referral was requested because computed tomography (CT) revealed a giant colonic diverticulum.
The patient had a history of atrial fibrillation, chronic obstructive pulmonary disease, hypertension, and hyper
The patient denied having any family history of diverticular disease.
Upon examination, his abdomen was soft and non-tender with no palpable mass.
His laboratory results including the white blood cell count were within normal limits.
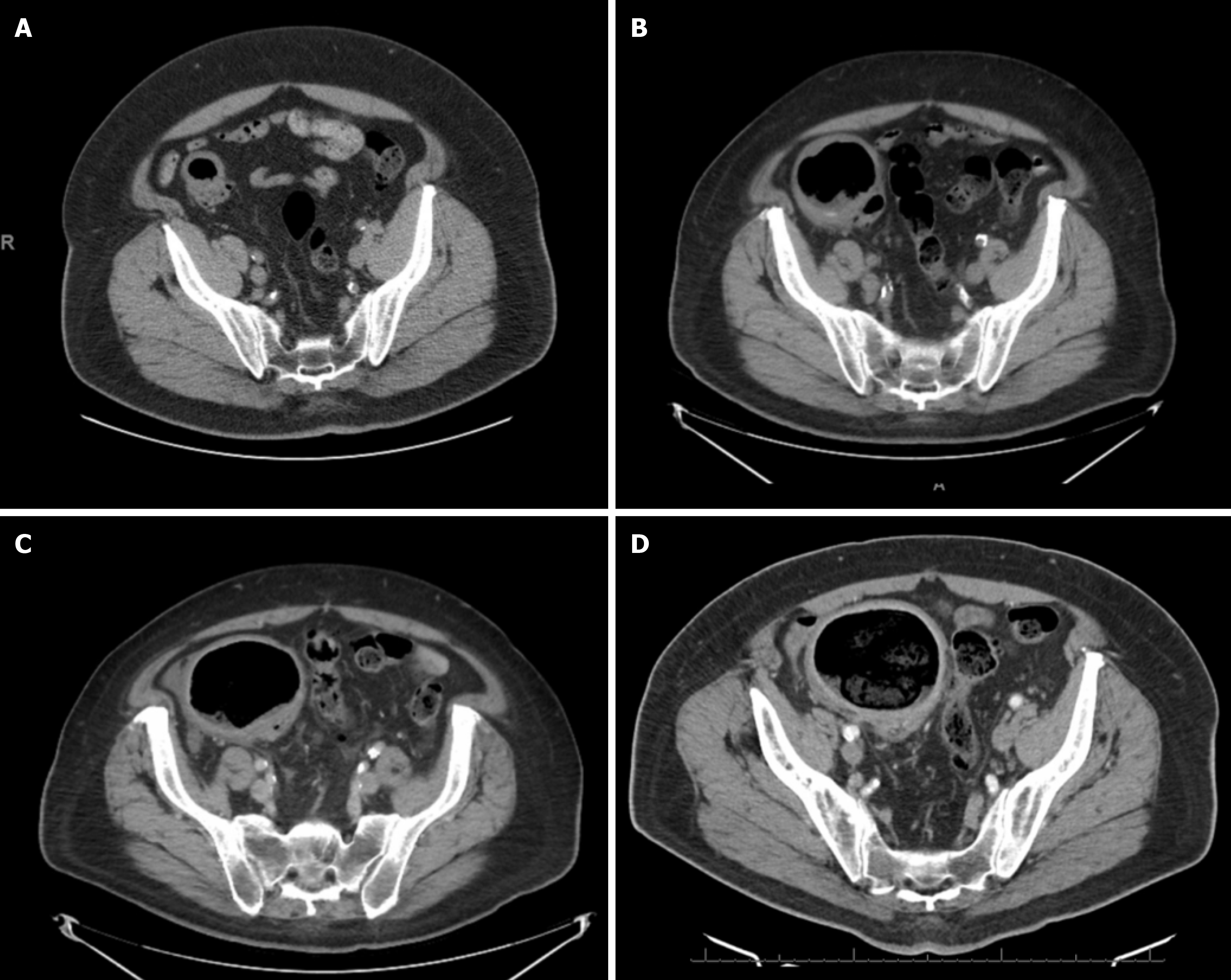
The patient had recently undergone CT of the abdomen and pelvis, which revealed a giant sigmoid colonic diverticulum in the right lower quadrant with thickening of the colon wall and measuring 9.7 cm in diameter (Figure 1).
Two years before this presentation, the patient had undergone a CT scan during an episode of acute diverticulitis. This scan revealed a diverticulum approximately 3 cm in diameter (Figure 2). One year later, he underwent another CT scan when he developed abdominal distension after cardiac ablation, at which point the diverticulum was approximately 6 cm in diameter. Six months later, the patient presented to the emergency department with right upper quadrant pain and underwent a CT scan, which revealed findings consistent with acute cholecystitis. Incidentally, the diverticulum was also seen, and measured 8 cm in diameter at that time.
Notably, the patient underwent a recent colonoscopy that revealed sigmoid diverticular disease in addition to two small tubular adenomas, although the giant diverticulum could not be visualized.
After reviewing the patient’s history and imaging findings, the final diagnosis was giant colonic diverticulum.
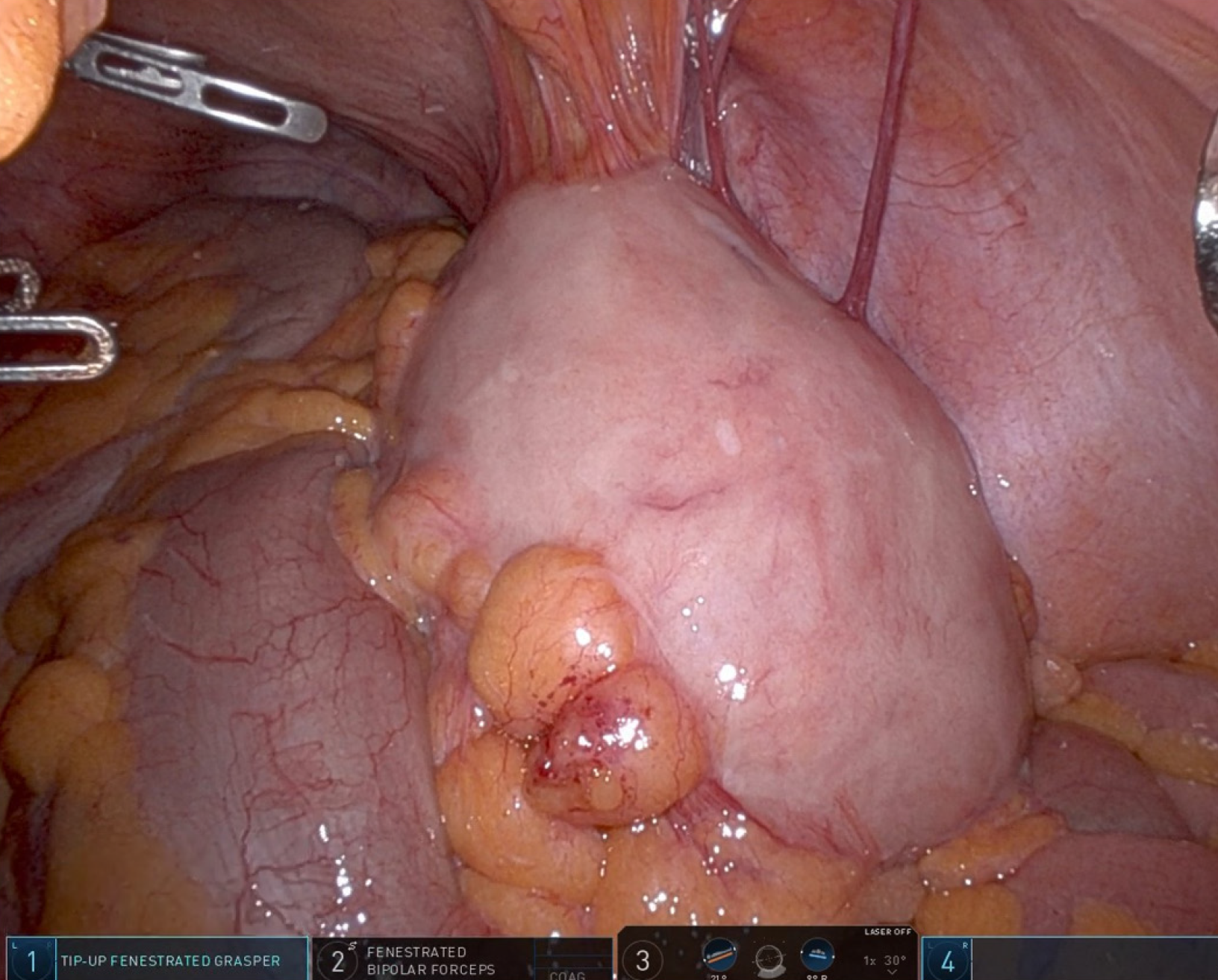
After a discussion, the patient underwent robot-assisted sigmoid colectomy. Prior to the operation, the patient underwent an enhanced recovery after surgery (ERAS) protocol, which included both mechanical and oral antibiotic bowel preparations and administration of intrathecal morphine. The operation was uneventful, and primary anastomosis was per
His postoperative course was uneventful; utilizing an enhanced recovery protocol, the patient showed an early return to bowel function and was discharged on postoperative day 2. During postoperative visits, the patient experienced re
Giant colonic diverticulum is a rare complication of diverticular disease, with only a few cases reported in the literature. McNutt et al[2] classified this into three types, with most patients (type 2) developing the condition because of subserosal perforation. It is theorized that this gradually increases in size owing to a ball-valve mechanism, in which air and stool can enter the diverticulum but not exit. Some patients also present with a colonic pseudodiverticulum with remnants of the muscularis mucosa and muscularis (type 1). The rarer type is a true diverticulum that typically has a congenital origin and is found during childhood (type 3). The patient in this case report was most likely to have a type 2 giant colonic di
Although occasionally detected incidentally, the most common symptoms include abdominal pain, constipation, bloating, and diarrhea. In some patients, abdominal masses were palpable. Typically, a diagnosis is made using CT; however, in certain instances, it may be diagnosed via barium enema or even plain radiography.
Giant colonic diverticula may also result in complicated diseases that require urgent intervention. While several cases of perforated giant colonic diverticula have been reported[3], there have also been reports of obstruction[4] and colonic volvulus[5].
Originally, diverticulectomy was considered an option for treating patients with giant colonic diverticula. In a case series involving four patients, Choong and Frizelle[6] described resecting the diverticulum at the base and oversewing the resultant colonic defect. However, as giant colonic diverticula is now considered a complication of diverticular disease, and sigmoid diverticulosis is typically present, segmental colectomy has become the preferred approach.
In a 2015 case series of 166 patients with giant colonic diverticula, most patients were treated with segmental colon resection and primary anastomosis[1]. Other treatment options included Hartmann’s procedure. Only five patients were treated laparoscopically. In 2019, the first reported robotic colectomy was performed for the treatment of a giant colonic diver
This case reinforces the feasibility of a robotic approach for the treatment of giant colonic diverticula. Given its myriad benefits, MIS should be considered whenever possible for treating this condition. Furthermore, by demonstrating the enlargement of a giant colonic diverticulum over a two-year period, this report may help elucidate the clinical course of patients with giant colonic diverticula who may be at a high risk of undergoing surgery.
| 1. | Nigri G, Petrucciani N, Giannini G, Aurello P, Magistri P, Gasparrini M, Ramacciato G. Giant colonic diverticulum: clinical presentation, diagnosis and treatment: systematic review of 166 cases. World J Gastroenterol. 2015;21:360-368. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 56] [Cited by in RCA: 49] [Article Influence: 4.9] [Reference Citation Analysis (35)] |
| 2. | McNutt R, Schmitt D, Schulte W. Giant colonic diverticula--three distinct entities. Report of a case. Dis Colon Rectum. 1988;31:624-628. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 46] [Article Influence: 1.2] [Reference Citation Analysis (2)] |
| 3. | Khaikin M, Zbar AP, Mezhibovsky V, Gutman M, Weidenfeld J, Aviel-Ronen S. Perforated giant sigmoid diverticulum. Tech Coloproctol. 2013;17:251-252. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (2)] |
| 4. | Majeski J, Durst G Jr. Obstructing giant colonic diverticulum. South Med J. 2000;93:797-799. [PubMed] |
| 5. | Carr JA. Case report of a giant colonic sigmoid diverticulum causing sigmoid volvulus. Int J Surg Case Rep. 2017;31:197-199. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (1)] |
| 6. | Choong CK, Frizelle FA. Giant colonic diverticulum: report of four cases and review of the literature. Dis Colon Rectum. 1998;41:1178-1185. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 70] [Article Influence: 2.6] [Reference Citation Analysis (2)] |
| 7. | Benlice C, Aytac E, Baca B, Hamzaoglu I, Karahasanoglu T. Robotic sigmoidectomy for giant diverticula with the da Vinci Xi - a video vignette. Colorectal Dis. 2019;21:977-978. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (1)] |
| 8. | Klarenbeek BR, Veenhof AA, Bergamaschi R, van der Peet DL, van den Broek WT, de Lange ES, Bemelman WA, Heres P, Lacy AM, Engel AF, Cuesta MA. Laparoscopic sigmoid resection for diverticulitis decreases major morbidity rates: a randomized control trial: short-term results of the Sigma Trial. Ann Surg. 2009;249:39-44. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 241] [Cited by in RCA: 240] [Article Influence: 15.0] [Reference Citation Analysis (1)] |
| 9. | Veneroni S, Porzani S, Fancellu A. Giant colonic diverticulum: perioperative management with ERAS protocol. ANZ J Surg. 2023;93:1712-1714. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (1)] |