Published online Jun 16, 2024. doi: 10.12998/wjcc.v12.i17.3144
Revised: April 12, 2024
Accepted: April 19, 2024
Published online: June 16, 2024
Processing time: 141 Days and 6.9 Hours
Myositis ossificans (MO) is a rare disease involving the formation of bone outside the musculoskeletal system. While surgical intervention is the main treatment approach, preventing recurrence and standardized rehabilitation are also crucial. Here, we present a surgical strategy to prevent the recurrence of MO.
A 28-year-old female patient was admitted for the first time for a comminuted fracture of the left olecranon. However, incorrect postoperative rehabilitation resulted in the development of elbow joint stiffness with ectopic ossification, cau
The Ilizarov frame is an advantageous surgical technique for facilitating rehabi
Core Tip: In this case report, we report a 28-year-old female with myositis ossificans. The patient had an ulnar humerus fracture early in the course of the disease, and after internal fixation treatment, the wrong rehabilitation method led to the occurrence of myositis ossificans. In this operation, we normalized the rehabilitation plan of the patient by the passive pulling force of Ilizarov technology, which made no recurrence after the removal of myositis ossificans, and achieved a good effect.
- Citation: Zhou MW, Zhang PW, Zhang AL, Wei CH, Xu YD, Chen W, Fu ZB. Ilizarov technique for treating elbow stiffness caused by myositis ossificans: A case report. World J Clin Cases 2024; 12(17): 3144-3150
- URL: https://www.wjgnet.com/2307-8960/full/v12/i17/3144.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i17.3144
Myositis ossificans (MO) is a rare disease characterized by ectopic ossification within soft tissues[1]. It typically occurs following trauma and affects the major muscles of the limbs. However, it can also occur throughout the body, but is more commonly seen in the skeletal muscles of the limbs (such as the quadriceps femoris in the lower limb, the muscles on the inner side of the abdomen, or the muscles in the upper arm) or the soft tissues around joints (such as fibrous tissue, subcutaneous tissue, ligaments, and even blood vessel walls)[2,3]. The etiology and pathogenesis of this disease are still unclear. Trauma and intense exercise can cause muscle rupture, hemorrhage, and hematoma formation[4]. Most patients absorb the hematoma, but some may also develop muscle stiffness and ossification, eventually leading to joint stiffness and disability in the affected muscles. Surgery has been identified as a potential cause of MO, with factors such as sur
However, MO often presents with atypical clinical symptoms and has limited imaging diagnosis for early lesions, leading to confusion with benign and malignant conditions such as musculoskeletal infections, soft tissue sarcomas, and osteosarcomas, which can result in missed diagnosis and misdiagnosis, thereby delaying timely recovery of patients[6]. Pathological biopsy is the gold standard for diagnosing MO, and computed tomography shows typical features as the lesion matures.
Enhancing clinical awareness and attention to MO is necessary because, if left untreated, it can have a significant impact on physical health and increase the economic burden on the patient's family and society. Timely and appropriate treatment and prevention of recurrence of ectopic ossification are crucial, although surgical strategies commonly used for treating MO are challenging in terms of preventing recurrence and ensuring recovery. Based on this, a strategy using the Ilizarov frame is proposed for treatment and prevention of recurrence[7].
We present a case of a 28-year-old woman with nontraumatic MO of the elbow joint, and review the relevant literature.
The patient was a 28-year-old woman who sought treatment at our hospital because of unsatisfactory results following her first elbow joint surgery.
When the patient came to our hospital for treatment, she experienced stiffness and pain in the elbow joint, along with limited bending and straightening ability.
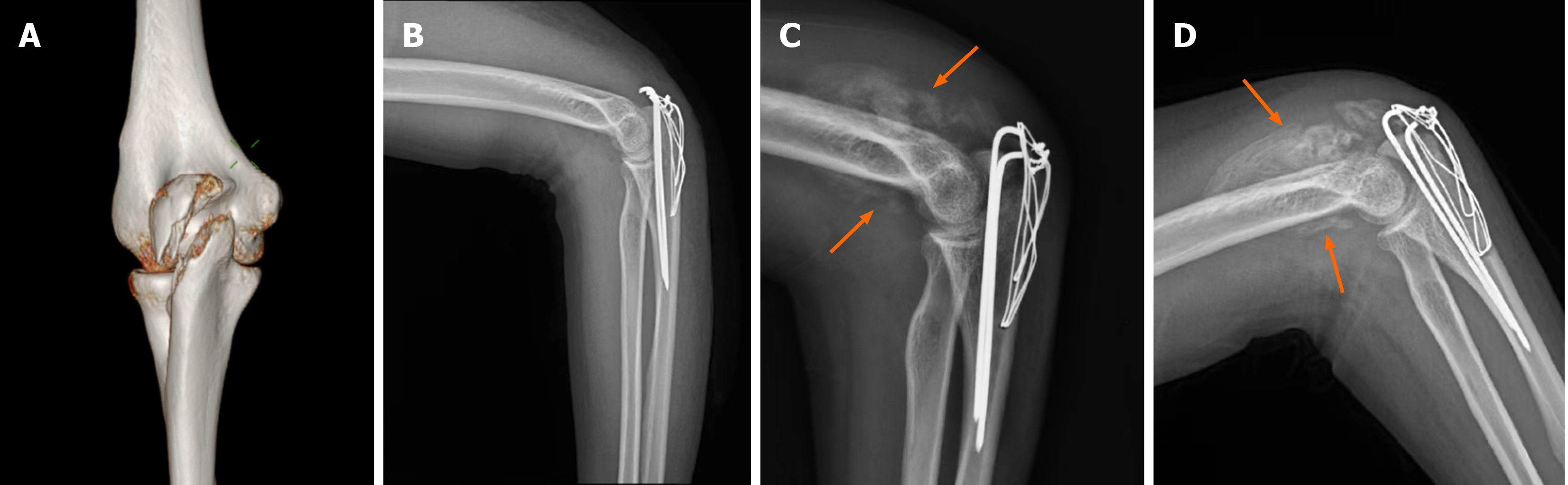
Six months ago, the patient sustained a cycling injury that resulted in a comminuted fracture of the left olecranon (Figure 1A). At our hospital, the patient underwent open reduction and internal fixation surgery for the fracture (Figure 1B). Upon discharge, the patient experienced pain and had difficulty in extending and flexing the left elbow. Un
The patient had no family history of relevant illnesses.
The patient had a body temperature of 36.4°C, blood pressure of 112/72 mmHg, respiratory rate of 12 breaths/min, heart rate of 68 bpm, and was fully alert. A 5-cm surgical scar in the left elbow region was observed, which exhibited no tend
No abnormalities were found in the laboratory examinations.
X-ray examination conducted 6 wk after surgery revealed progressive MO at the site of the previous fracture of the left ulna and elbow joint (Figure 1C). Further assessment resulted in a diagnosis of postoperative elbow stiffness with MO after internal fixation. The left ulnar fracture remained internally fixed, but heterotopic ossification developed after fracture of the left elbow joint. The H-G classification categorized it as type IIIA (Figure 1D).
The clinical diagnosis was MO causing stiffness in the elbow joint.
After routine preoperative examination and treatment, the decision was made to perform internal fixation removal, MO excision, elbow joint release, and combined orthopedic surgery. The operations were conducted with the patient in the supine position and under nerve block anesthesia. Following routine iodine disinfection of the left upper limb, sterile dressings were applied. The incision was made on the posterior side, extending proximally for 12 cm (Figure 2A). Sub
In the first 3 d after surgery, a drainage tube was placed and 160 mL bloody fluid was drained. Postoperative X-ray showed that the joint alignment was good and there were no obvious abnormalities (Figure 3A and B). After 3 d, the drainage tube was removed and ultrasound-guided puncture was performed to ensure no local hematoma. Passive fle
The development of MO in our patient may be attributed to three factors. First, the initial fracture surgery inflicted sig
Violence-induced joint and surrounding soft tissue injuries have been found to have a significant impact on local blood circulation, resulting in local swelling[10]. During the early stage after trauma, the acute phase reaction leads to an in
Excessive rehabilitation training can lead to tissue damage and inflammation, which activates a series of biochemical reactions[18]. These reactions trigger an inflammatory response, activate immune cells, and produce inflammatory me
Before surgery, several factors should be considered. First, it is crucial to acknowledge that patients may lack know
The Ilizarov frame technique offers several advantages. First, it provides good stability and support, which effectively stabilizes the site of the fracture or bone lesion, prevents displacement, and promotes bone healing. Second, the Ilizarov frame can be adjusted in terms of angle and position according to the specific conditions of different patients, enabling individualized treatment. Third, it allows for the preservation of joint mobility, making it particularly useful in cases of joint injury by facilitating rehabilitation. Lastly, the Ilizarov frame eliminates the need for extensive resection or internal implants, thereby reducing the risks associated with surgery. Compared to open surgery, it involves a smaller incision and potentially lowers the risk of complications.
The installation of the Ilizarov frame may cause pain, discomfort and skin damage, requiring the patient's patience and maintenance. Complications such as skin problems and nerve damage may also occur. Moreover, the Ilizarov frame may increase the risk of infection as it needs to penetrate the skin. However, despite these potential drawbacks, the Ilizarov frame is widely used in orthopedic surgery due to its effectiveness in treating complex fractures and deformities.
The Ilizarov frame may be considered as a viable alternative for surgical treatment and prevention of recurrence in MO. It offers the advantages of minimal invasiveness and quick recovery. However, long-term follow-up is necessary to de
| 1. | Ji T, Zhang G, Zhang J, Li Y, Zhang X, Liu Q, Sun N, Liu Z, Li X, Liu Y, Wang S, Ni X. Myositis Ossificans of the Trapezius Muscle: A Case Report and Literature Review. Ear Nose Throat J. 2023;1455613231175316. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |
| 2. | Simmonds J, Taki N, Chilton I, Vecchiotti M. A rare case of pediatric Nontraumatic Myositis Ossificans in the posterior triangle. Int J Pediatr Otorhinolaryngol. 2016;84:116-118. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 8] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 3. | Kokkosis AA, Balsam D, Lee TK, Schreiber ZJ. Pediatric nontraumatic myositis ossificans of the neck. Pediatr Radiol. 2009;39:409-412. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 4. | Lawand J, Loeffelholz Z, Khurshid B, Barcak E. Heterotopic Ossification after Trauma. Orthop Clin North Am. 2023;54:37-46. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 10] [Reference Citation Analysis (0)] |
| 5. | Balboni TA, Gobezie R, Mamon HJ. Heterotopic ossification: Pathophysiology, clinical features, and the role of radiotherapy for prophylaxis. Int J Radiat Oncol Biol Phys. 2006;65:1289-1299. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 199] [Cited by in RCA: 208] [Article Influence: 10.9] [Reference Citation Analysis (0)] |
| 6. | Smilde BJ, Botman E, de Ruiter RD, Smit JM, Teunissen BP, Lubbers WD, Schwarte LA, Schober P, Eekhoff EMW. Monitoring and Management of Fibrodysplasia Ossificans Progressiva: Current Perspectives. Orthop Res Rev. 2022;14:113-120. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 13] [Reference Citation Analysis (0)] |
| 7. | Spiegelberg B, Parratt T, Dheerendra SK, Khan WS, Jennings R, Marsh DR. Ilizarov principles of deformity correction. Ann R Coll Surg Engl. 2010;92:101-105. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 122] [Cited by in RCA: 104] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 8. | Cole PA, Dugarte AJ, Talbot M, Routt MLC Jr. Early resection of ectopic bone in patients with heterotopic ossification about the hip after trauma. Injury. 2020;51:705-710. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 7] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 9. | Dubuisson A, Lombard A, Otto B. Pseudomalignant Myositis Ossificans of the Neck in a Child: Case Report and Review of the Literature. World Neurosurg. 2019;130:95-97. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 9] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 10. | Bai Q, Zou X, Yang G, Fan Y, Wang W, Zhang B, Chang X. Painful and restricted hip due to myositis ossificans circumscripta of the pectineus muscle after pelvic fracture: A case report. Medicine (Baltimore). 2023;102:e33694. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |
| 11. | Haviv R, Moshe V, De Benedetti F, Prencipe G, Rabinowicz N, Uziel Y. Is fibrodysplasia ossificans progressiva an interleukin-1 driven auto-inflammatory syndrome? Pediatr Rheumatol Online J. 2019;17:84. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 19] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 12. | Galeano A, Fraison JB, Viala P, Le Blay P, Jorgensen C, Pers YM. Acute inflammatory myalgia: think of myositis ossificans circumscripta. J Rheumatol. 2013;40:1614-1615. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 13. | de Ruiter RD, Wisse LE, Schoenmaker T, Yaqub M, Sánchez-Duffhues G, Eekhoff EMW, Micha D. TGF-Beta Induces Activin A Production in Dermal Fibroblasts Derived from Patients with Fibrodysplasia Ossificans Progressiva. Int J Mol Sci. 2023;24. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 14. | Vitale V, Bleve C, Mansour M, De Corti F, Giarraputo L, Brugiolo A, Affinita MC, Santoro L, Chiarenza SF, Iannucci G. Non-traumatic Myositis Ossificans as Unusual Cause of Neck Pain During COVID-19 Pandemic: a Case Report. SN Compr Clin Med. 2022;4:96. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 15. | Brance ML, Cóccaro NM, Casalongue AN, Durán A, Brun LR. Extensive progressive heterotopic ossification post-Covid-19 in a man. Bone. 2022;155:116287. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 8] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 16. | Kou S, Kile S, Kambampati SS, Brady EC, Wallace H, De Sousa CM, Cheung K, Dickey L, Wentworth KL, Hsiao EC. Social and clinical impact of COVID-19 on patients with fibrodysplasia ossificans progressiva. Orphanet J Rare Dis. 2022;17:107. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 17. | Godoy IRB, Rodrigues TC, Skaf A. Myositis ossificans following COVID-19 vaccination. QJM. 2021;114:659-660. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 14] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 18. | Peake JM, Neubauer O, Walsh NP, Simpson RJ. Recovery of the immune system after exercise. J Appl Physiol (1985). 2017;122:1077-1087. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 143] [Cited by in RCA: 196] [Article Influence: 21.8] [Reference Citation Analysis (0)] |
| 19. | Nieman DC, Wentz LM. The compelling link between physical activity and the body's defense system. J Sport Health Sci. 2019;8:201-217. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 562] [Cited by in RCA: 697] [Article Influence: 116.2] [Reference Citation Analysis (0)] |
| 20. | Barruet E, Morales BM, Cain CJ, Ton AN, Wentworth KL, Chan TV, Moody TA, Haks MC, Ottenhoff TH, Hellman J, Nakamura MC, Hsiao EC. NF-κB/MAPK activation underlies ACVR1-mediated inflammation in human heterotopic ossification. JCI Insight. 2018;3. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 78] [Article Influence: 11.1] [Reference Citation Analysis (0)] |
| 21. | Sangadala S, Shore EM, Xu M, Bergwitz C, Lozano-Calderon SA, Lin AE, Boden SD, Kaplan FS. Multifocal heterotopic ossification in a man with germline variants of LIM Mineralization Protein-1 (LMP-1). Am J Med Genet A. 2023;191:2164-2174. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 22. | Ravazzolo R, Cappato S, Bocciardi R. Hints on transcriptional control of essential players in heterotopic ossification of Fibrodysplasia Ossificans Progressiva. Bone. 2018;109:187-191. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 23. | Xu YJ, Gao X, Ding H, Bu XM, Wang HB, Wu B. Effects of 1-stage revascularization and temporary external fixation combined with 2-stage Ilizarov technique in the treatment of bone defects in lower limb destruction injury: A case report. Medicine (Baltimore). 2022;101:e30149. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 24. | Boquan Q, Yi R, Tingjiang G, Xi L, Hui Z. Complex foot deformities associated with lower limb deformities: a new therapeutic strategy for simultaneous correction using Ilizarov procedure together with osteotomy and soft tissue release. J Orthop Surg Res. 2020;15:492. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 0.8] [Reference Citation Analysis (0)] |