Published online Jun 16, 2024. doi: 10.12998/wjcc.v12.i17.3123
Revised: March 17, 2024
Accepted: April 19, 2024
Published online: June 16, 2024
Processing time: 162 Days and 2.6 Hours
Due to mechanical imbalance in the spine, elderly scoliosis patients tend to develop vertebral fracture nonunion, i.e., Kümmell disease, when osteoporotic vertebral compression fractures occur. However, accompanying vertebral rotational deformities make surgical procedures challenging risky. Such patients are usually compelled to undergo conservative treatment and there are very few reports on minimally invasive surgeries for them. We first-time report a patient with Kümmell disease and lumbar scoliosis treated with percutaneous kypho
An 89-year-old female was admitted to the hospital due to delayed low back pain after a fall. She was diagnosed with Kümmell disease based on physical and radiologic examinations. The patient experienced severe scoliosis and sub
PKP has good efficacy in treating Kümmell disease. However, surgical risks are elevated in scoliosis patients with Kümmell disease due to the abnormal anatomical structure of the spine. O-arm assisted operations play a crucial role in decreasing surgical risks.
Core Tip: We reported a case of severe lumbar scoliosis combined with vertebral fracture nonunion with extremely high surgical risks due to severe vertebral deformity. We performed O-arm-guided kyphoplasty on the patient and achieved good results. This paper describes some of the experiences and techniques in performing Kyphoplasty for such patients.
- Citation: Saijilafu, Zhou JW, Wang GL, Sun KH, Xie JL. Percutaneous kyphoplasty in the treatment of Kümmell disease in lumbar scoliosis: A case report. World J Clin Cases 2024; 12(17): 3123-3129
- URL: https://www.wjgnet.com/2307-8960/full/v12/i17/3123.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i17.3123
Kümmell disease refers to vertebral fracture nonunion following osteoporotic vertebral compression fractures (OVCF) and is a form of vertebral body avascular necrosis. Kümmell disease usually occurs several weeks to months after a minor injury, presenting with persistent low back pain. X-ray and computed tomography (CT) examinations reveal vertebral compression deformities and vacuum clefts within the vertebra[1]. Tsujio et al[2] found that 13.5% of OVCF patients developed Kümmell disease after 6 months of conservative treatment. Previous studies have shown that vertebral augmentation procedures, including percutaneous kyphoplasty (PKP) and percutaneous vertebroplasty (PVP), to be effective in treating Kümmell disease[1]. Due to mechanical imbalance in the spine, scoliosis patients tend to develop Kümmell disease, when OVCF occur. Given the accompanying vertebral rotational deformities, performing vertebral augmentation procedures in scoliosis patients presents challenges and higher risks. In this paper, we report a patient with Kümmell disease and lumbar scoliosis treated with PKP under O-arm guidance.
An 89-year-old female was admitted to the hospital due to low back pain for 2 wk following a fall 4 wk ago.
The patient fell down accidentally at home 4 wk ago, landing on her buttocks. She did not experience dizziness or significant discomfort at that time. However, she began experiencing worsening low back pain 2 wk post-fall. Lower limb numbness and weakness were absent. Low back pain was alleviated after lying down. She sought medical attention at a hospital and CT scan showed lumbar scoliosis, a L2 vertebral body fracture, and a L1-2 vertebral body fusion. She was admitted for further evaluation and treatment by the orthopedics department for “lumbar vertebral fracture nonunion (Kümmell disease), lumbar scoliosis, and lumbar vertebral fusion” in October 2023.
The patient had a history of hypertension for 20 years, regularly takes oral amlodipine besylate and hydrochlorothiazide for treatment, and the blood pressure was well controlled.
The patient denied a family history of OVCF.
The patient exhibited normal head and neck mobility, uneven shoulders, and thoracolumbar scoliosis. The Adams test was positive, and the tenderness was noted upon percussion in the thoracolumbar spine. Sensation in both lower limbs was normal, and muscle tone was not elevated, with muscle strength graded as 5. The straight leg raising test was positive on the right side. Both knee reflexes and ankle reflexes were normal, and the Babinski sign was negative.
No significant surgical contraindications were revealed in preoperative laboratory examinations.
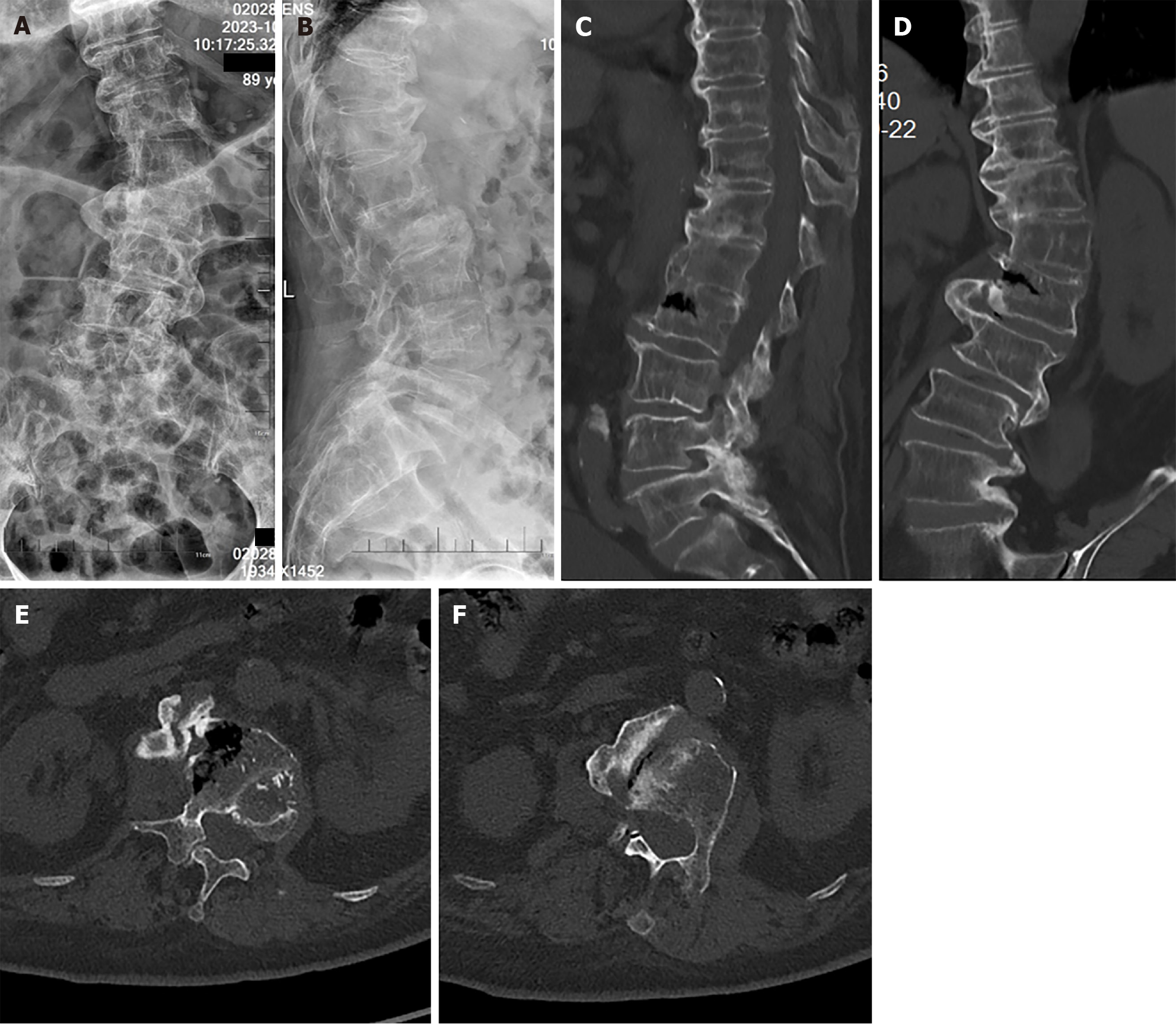
The patient’s X-ray showed lumbar scoliosis, Cobb angle 40°, L1-2 vertebral body osseous fusion, bone bridge formation between L1-2 and L2-3 vertebral bodies, and L5 vertebral body spondylolisthesis (Meyerding grade I) (Figure 1A and B). The rotation of L2 vertebra was grade II according to Nash-Moes classification. CT images showed L1-2 vertebral body osseous fusion, and L2 intravertebral vacuum clefts and sclerosis margin (Figure 1C-F).
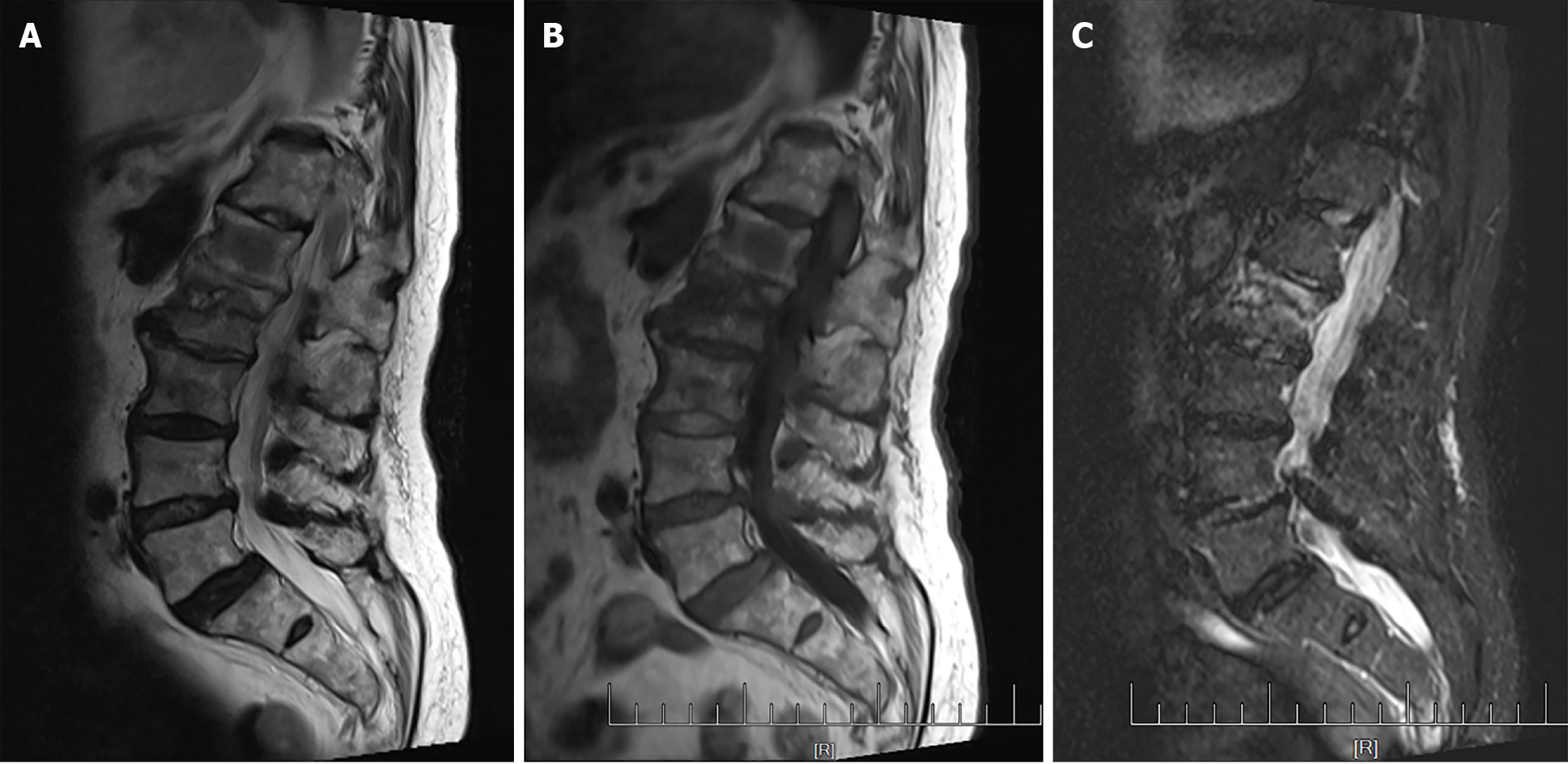
T2-weighted imaging and T1-weighted imaging magnetic resonance imaging (MRI) examinations showed bone sclerosis in L2 vertebral body cleft margins (Figure 2A and B) and short tau inversion recovery sequence shows L2 intravertebral hyper intense signals, indicating fracture nonunion (Figure 2C).
Vertebral fracture nonunion (Kümmell disease), degenerative lumbar scoliosis, vertebral fusion, osteoporosis, hypertension.
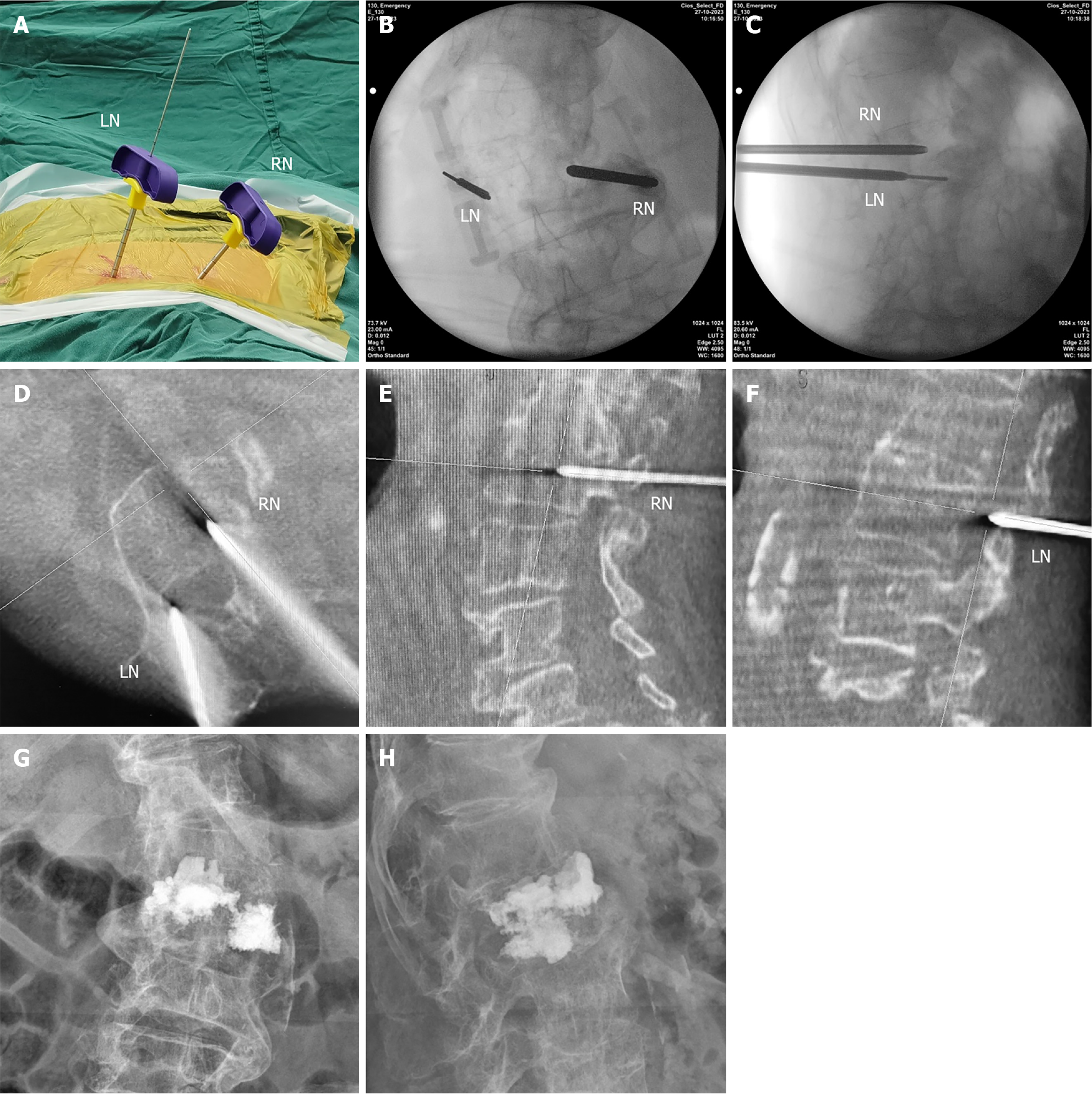
The patient underwent an O-arm-assisted lumbar vertebral PKP procedure. Due to vertebral body rotation, the medial oblique angle of the right positioning needle was greater than normal while the left positioning needle was tilted laterally (Figure 3A-C). The O-arm scan found that the right positioning needle was successfully inserted through the pedicle into the vertebral body, while the lateral oblique angle of the left positioning needle was small and penetrated the cortex of the spinal canal (Figure 3D-F). Therefore, the surgeon immediately adjusted the left needle and increased the lateral oblique angle. A guide pin was used to confirm that the working cannula was located in the pedicle. Subsequently, the bone cement was slowly injected under fluoroscopy, with 4.5 mL in the right side and 3 ml in the left side. Postoperative fluoroscopy confirmed adequate diffusion of bone cement in both sides of the vertebral body, with no significant leakage observed.
The patient experienced significant alleviation of low back pain immediately post-surgery. On the second day after the operation, the patient could resume ambulatory activities normally without lower limb pain and numbness. The postoperative X-ray examination showed well-diffused bone cement (Figure 3G and H). The patient got a follow up of 3 months and had no low back pain during the follow-up.
Kümmell disease refers to fracture nonunion caused by avascular necrosis after vertebral fractures and was first reported by Hermann Kümmell in 1895[3]. The diagnosis of Kümmell disease relies on a combination of medical history, clinical presentation, and radiologic examination. The patients usually lack a history of significant trauma and develop refractory low back pain after an asymptomatic period lasting several weeks to months[1]. Disease progression often leads to vertebral body height loss and kyphosis of the spine. Radiological findings, including intravertebral clefts, marginal sclerosis and pseudo joint formation revealed by X-ray and CT scans, and intravertebral fluid signals with clear boundaries revealed by MRI, aid in diagnosis[4]. Kümmell disease predominantly affects elderly osteoporosis patients and its onset often attributed to combined effects of multiple mechanisms. Vertebral body compression fractures usually occur in the anterior vertebral body, where blood supply is relatively poor, leading to ischemia and avascular necrosis of the vertebral body[5]. Loss of trophic supply to the vertebral body contributes to its atrophy. In osteoporosis patients, even mild external forces can cause microfractures in the intravertebral trabecular bone, which gradually progresses to symptomatic vertebral fractures over time. Given the vertebral body’s role as a load-bearing structure, repeated external force stimulation exacerbates microfractures progression, eventually resulting in vertebral body collapse, fracture nonunion, and pseudo joint formation[6].
Elderly scoliosis patients often experience disruptions in the coronal and sagittal balance of the spine, leading to vertebral instability. This heightened instability renders them more susceptible to vertebral fractures and fractures nonunion. In this patient, the L2 vertebral body depression formed a significant cleft and marginal sclerosis. We speculate that this may be attributed to the L1-2 vertebrae serving as the apex vertebrae of scoliosis, where mechanical loading intersects, and its concave side bears greater compressive stress.
The effects of conservative treatment are poor in Kümmell disease. This is because conservative treatment for vertebral fractures is mainly bed rest, which accelerates bone loss and hampers fracture healing[7]. Therefore, Kümmell disease usually requires surgical intervention. Currently, vertebral augmentation procedures include PVP and PKP, which are effective for treating OVCF and vertebral tumors, have showed good efficacy in treating Kümmell disease[8,9]. Balloon expansion in PKP can partially restore vertebral body height, and intravertebral injection of bone cement can increase vertebral body stability and alleviate pain[10].
In scoliosis patients, the presence of vertebral body deformities and rotation introduces additional complexities, making the surgical procedures more challenging. PKP relies on X-ray fluoroscopy to determine the pedicle channel and establish a working cannula. Various strategies can be used to enhance the safety in these cases. Preoperative planning is extremely important, with preoperative CT scan providing valuable measurements of the vertebral body rotation angle and pedicle oblique angle, adding in cannula placement during the operation. In the surgery, it is necessary to adjust the anteroposterior X-ray projection angle of the spine to ensure that the spinous process is in the middle of vertebra, facilitating the determination of the actual medial oblique angle of the positioning needle. The needle insertion angle must be adjusted according to vertebral body rotation. Usually, the positioning needle should have a suitable medial oblique angle to enter the pedicle. In this patient, the left positioning needle exhibited an oblique angle incline to the lateral side of the vertebra due to vertebral body rotation. The intraoperative O-arm scan showed that this positioning needle was still medial oblique relatively to the vertebral body. Therefore, it is imperative to perform a working cannula examination using the O-arm, as it improves surgical safety and decreases the probability of intraoperative nerve damage, bone cement leakage into the spinal canal, and other catastrophic complications.
Intravertebral clefts and vertebral wall destruction increase the risk of bone cement leakage during PKP procedures[11]. To mitigate this risk, several techniques can be used. Bone cement should be injected at the end phase of its solidification. When the bone cement reaches the intravertebral cleft, cement injection can be paused for 1-2 min to allow for accelerated solidification via body temperature, sealing the cleft and reducing the risk of leakage. After that, the surgeon can reprepare bone cement and inject in a low viscosity state, to facilitate optimal anchoring of bone cement within the hardened bone in the vertebral body, leading to a more stable fixation[12]. In conclusion, PKP more complex than it may appear, and it is necessary that the procedure performed by an experienced surgeon, particularly in cases involving patients with scoliosis and Kümmell disease.
PKP demonstrates good efficacy in treating Kümmell disease. However, surgical risks are elevated in scoliosis patients with Kümmell disease due to the abnormal anatomical structure of the spine. O-arm assisted operations play a crucial role in decreasing surgical risks.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s classification
Scientific Quality: Grade D
Novelty: Grade B
Creativity or Innovation: Grade C
Scientific Significance: Grade D
P-Reviewer: Zacharia B, India S-Editor: Zheng XM L-Editor: A P-Editor: Li X
| 1. | Yang H, Pan J, Wang G. A review of osteoporotic vertebral fracture nonunion management. Spine (Phila Pa 1976). 2014;39:B4-B6. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 40] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 2. | Tsujio T, Nakamura H, Terai H, Hoshino M, Namikawa T, Matsumura A, Kato M, Suzuki A, Takayama K, Fukushima W, Kondo K, Hirota Y, Takaoka K. Characteristic radiographic or magnetic resonance images of fresh osteoporotic vertebral fractures predicting potential risk for nonunion: a prospective multicenter study. Spine (Phila Pa 1976). 2011;36:1229-1235. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 109] [Cited by in RCA: 125] [Article Influence: 8.9] [Reference Citation Analysis (0)] |
| 3. | Young WF, Brown D, Kendler A, Clements D. Delayed post-traumatic osteonecrosis of a vertebral body (Kummell's disease). Acta Orthop Belg. 2002;68:13-19. [PubMed] |
| 4. | Ito Y, Hasegawa Y, Toda K, Nakahara S. Pathogenesis and diagnosis of delayed vertebral collapse resulting from osteoporotic spinal fracture. Spine J. 2002;2:101-106. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 88] [Cited by in RCA: 97] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 5. | Chou LH, Knight RQ. Idiopathic avascular necrosis of a vertebral body. Case report and literature review. Spine (Phila Pa 1976). 1997;22:1928-1932. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 62] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 6. | Ranjan M, Mahadevan A, Prasad C, Sommana S, Susarla Krishna S. Kümmell's disease - uncommon or underreported disease: A clinicopathological account of a case and review of literature. J Neurosci Rural Pract. 2013;4:439-442. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 7. | Krølner B, Toft B. Vertebral bone loss: an unheeded side effect of therapeutic bed rest. Clin Sci (Lond). 1983;64:537-540. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 266] [Cited by in RCA: 216] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 8. | Sanli I, van Kuijk SMJ, de Bie RA, van Rhijn LW, Willems PC. Percutaneous cement augmentation in the treatment of osteoporotic vertebral fractures (OVFs) in the elderly: a systematic review. Eur Spine J. 2020;29:1553-1572. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 12] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 9. | Kong LD, Wang P, Wang LF, Shen Y, Shang ZK, Meng LC. Comparison of vertebroplasty and kyphoplasty in the treatment of osteoporotic vertebral compression fractures with intravertebral clefts. Eur J Orthop Surg Traumatol. 2014;24 Suppl 1:S201-S208. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 27] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 10. | He Z, Zhai Q, Hu M, Cao C, Wang J, Yang H, Li B. Bone cements for percutaneous vertebroplasty and balloon kyphoplasty: Current status and future developments. J Orthop Translat. 2015;3:1-11. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 59] [Cited by in RCA: 53] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 11. | Tomas C, Jensen A, Ahmed F, Ho CK, Jesse MK. Minding the Gap in Vertebroplasty: Vertebral Body Fracture Clefts and Cement Nonunion. Pain Physician. 2021;24:E221-E230. [PubMed] |
| 12. | Yang H, Liu H, Wang S, Wu K, Meng B, Liu T. Review of Percutaneous Kyphoplasty in China. Spine (Phila Pa 1976). 2016;41 Suppl 19:B52-B58. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 52] [Article Influence: 5.8] [Reference Citation Analysis (0)] |