Published online Jun 16, 2024. doi: 10.12998/wjcc.v12.i17.2935
Revised: April 24, 2024
Accepted: May 11, 2024
Published online: June 16, 2024
Processing time: 92 Days and 23.5 Hours
The diagnosis of pancreatic cancer associates an appalling significance. Detection of preinvasive stage of pancreatic cancer will ameliorate the survival of this deadly disease. Premalignant lesions such as Intraductal Papillary Mucinous Neoplasms or Mucinous Cystic Neoplasms of the pancreas are detectable on ima
Core Tip: High-grade pancreatic intraepithelial neoplasia can be diagnosed by cytology of pancreatic juice before they become invasive carcinoma. Candidates to this diagnostic procedure are patients with disturbed anatomy in pancreatic imaging without evident tumor such as segmental atrophy of parenchyma, main pancreatic duct (MPD) stenosis/dilatation, focal blurred MPD or local parenchymal fatty changes.
- Citation: Morera-Ocon FJ. Early detection of pancreatic cancer. World J Clin Cases 2024; 12(17): 2935-2938
- URL: https://www.wjgnet.com/2307-8960/full/v12/i17/2935.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i17.2935
Pancreatic cancer continuous to be a dismal disease. Patients diagnosed with pancreatic ductal adenocarcinoma (PDAC) stage I resectable disease show 26-month median cancer-specific survival versus 4.8-month median survival in patients with unresectable stage IV disease[1]. Furthermore, the Japan Pancreatic Cancer Registry revealed that the 5-year survival rates of patients categorized with the Union Internationale Contre le Cancer stage 0 (in situ), and stage 1 TS1a (invasive carcinoma with tumor diameter of < 10 mm and absence of regional lymph node metastasis or distant metastasis) were 85.8%, and 80.4%, respectively[2]. Another study from Japan showed an estimated overall survival rates at 10 years after resection for stage 0, stage 1 TS1a, and stage 1 TS1b, i.e. tumor diameter 11-20 mm, of 94.7%, 93.8%, and 78.9%, respe
The recognized precursors of PDAC encompass a spectrum lesions such as pancreatic intraepithelial neoplasms (PanINs), intraductal papillary mucinous neoplasms (IPMN), intraductal tubulopapillary neoplasms, intraductal oncocytic papillary neoplasms, and mucinous cystic neoplasms (MCN)[4]. Grossly the most frequent and higher-risk for malignancy precursor lesions are PanIN high-grade (before PanIN 3), IPMN main-duct or mixed-type, and in less proportion the MCN with diameter of 4cm or larger.
Finding of PanIN or premalignant pancreatic cystic lesions constitutes an opportunity for patient management to minimize the risk of progression to invasive carcinoma.
Cystic pancreatic lesions are common incidental findings in cross-sectional imaging[5]. Diagnosis and management of these lesions has been established and revised in international guidelines[5-8]. Unlike the other precursor lesions, PanINs are lesions that cannot be detected by imaging [computed tomography (CT) or magnetic resonance imaging (MRI)] because of their microscopic identity[9] and lack of characterized associated indirect radiological signs. The PanIN lesions occur in the small pancreatic duct, are less of 5 mm in extension, and the tumor cannot be directly detected, therefore pancreatic tumors derived from PanIN lesions are seldom diagnosed by imaging modalities in stage 0 cases[3].
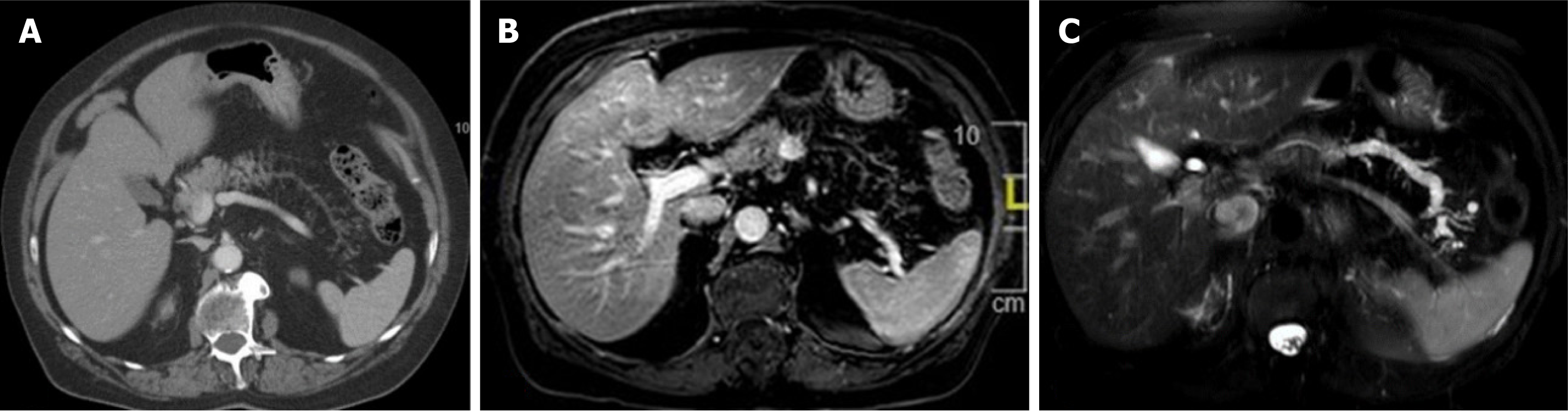
Nevertheless, main pancreatic duct strictures and dilations observed on imaging modalities (CT, MRI, and endoscopic ultrasound), additional partial pancreatic parenchymal atrophy[10] (Figure 1), and subtle or blurred parenchymal abnormalities related to secondary glandular disturbances from the PanIN can suggest the presence of early pancreatic lesions. In a retrospective multicenter study of early pancreatic cancer in Japan, Kanno et al[3] detected local fatty changes of the pancreatic parenchyma in 21/50 (42%) stage 0 and 61/146 (41.8%) stage I cases of the series.
In this editorial, we comment on another unspecific subtle abnormality report by Furuya et al[11]. The authors described a female patient with an incidental finding of pancreatic cyst. The magnetic resonance cholangiopancreatography showed signs of benign cyst but an ill-defined main pancreatic duct at the 20-mm length of the pancreatic tail without upstream dilation. Atypical cells were obtained by serial pancreatic juice aspiration cytology and distal pancreatectomy was performed and the histopathology revealed a high-grade PanIN.
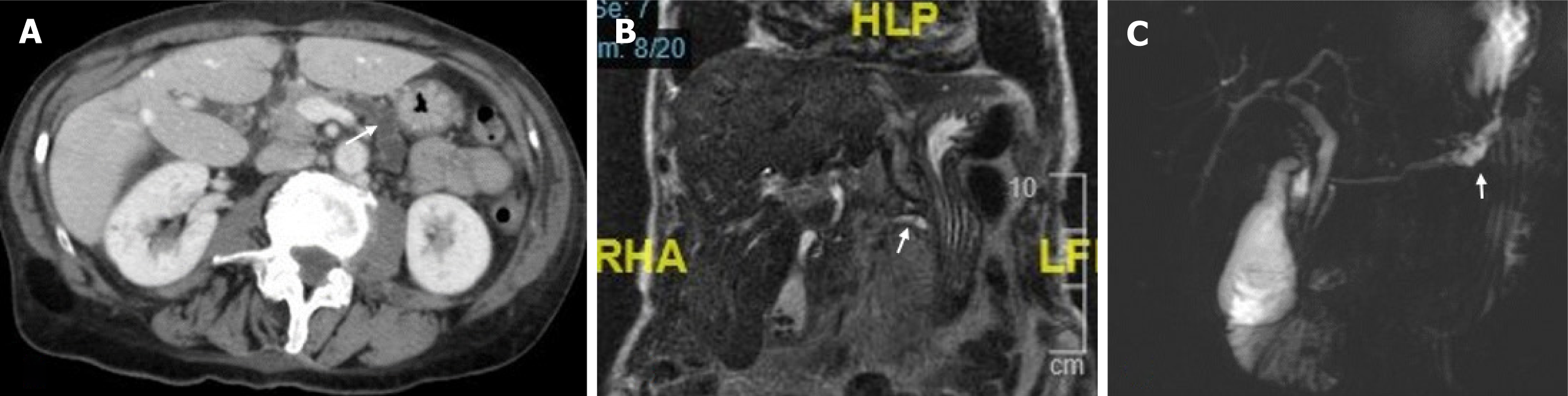
Surveillance of the patients with blurred focal distortion and unspecific signs by regular blood test and imaging exams, or pancreatic resection in patients with suspect images may lead to unnecessary burden of healthcare systems (Figure 2) and avoidable morbimortality.
Endoscopic ultrasound-fine needle aspiration is not useful for the preoperative diagnosis of malignancy in stage 0 cases. Nevertheless, stage 0 patients can be diagnosed using pancreatic juice cytology obtained by endoscopic nasopancreatic drainage (ENPD), as it has been comment early before in the case by Furuya et al[11]. Moreover, it was shown in the study by Iiboshi et al[12] were 7 of 15 patients presenting with focal stenosis and distal dilatation of the main pancreatic duct and included in the ENPD placement group were diagnosed with carcinoma in situ. The cytology of pancreatic juice is a procedure which has attracted the attention in the eastern groups, particularly in Japan centers[13-15], however its practice is not extended in the western countries. Only one study from a western institution has been published focusing in the DNA methylation analysis in isolated but non-multiple samples of pancreatic juice obtained in intraoperative pancreatic resections or by ERCP intubation in non-operated on patients[16], still it only has reached a research interest and has not been expanded in clinical practice.
In conclusion, the detection of pancreatic adenocarcinoma before it has reached an invasive stage (i.e. high-grade PanIN before PDAC) will provide a survival rate far superior to the overall survival associated with patients diagnosed with this deadly disease. This detection can be achieved using the analysis of cytology of pancreatic juice, a technique employed in eastern countries but not extended in western groups.
| 1. | Katz MH, Hu CY, Fleming JB, Pisters PW, Lee JE, Chang GJ. Clinical calculator of conditional survival estimates for resected and unresected survivors of pancreatic cancer. Arch Surg. 2012;147:513-519. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 48] [Article Influence: 3.7] [Reference Citation Analysis (35)] |
| 2. | Egawa S, Toma H, Ohigashi H, Okusaka T, Nakao A, Hatori T, Maguchi H, Yanagisawa A, Tanaka M. Japan Pancreatic Cancer Registry; 30th year anniversary: Japan Pancreas Society. Pancreas. 2012;41:985-992. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 257] [Cited by in RCA: 307] [Article Influence: 23.6] [Reference Citation Analysis (0)] |
| 3. | Kanno A, Masamune A, Hanada K, Maguchi H, Shimizu Y, Ueki T, Hasebe O, Ohtsuka T, Nakamura M, Takenaka M, Kitano M, Kikuyama M, Gabata T, Yoshida K, Sasaki T, Serikawa M, Furukawa T, Yanagisawa A, Shimosegawa T; Japan Study Group on the Early Detection of Pancreatic Cancer (JEDPAC). Multicenter study of early pancreatic cancer in Japan. Pancreatology. 2018;18:61-67. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 150] [Cited by in RCA: 169] [Article Influence: 24.1] [Reference Citation Analysis (0)] |
| 4. | Kim JY, Hong SM. Precursor Lesions of Pancreatic Cancer. Oncol Res Treat. 2018;41:603-610. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 22] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 5. | Tanaka M, Fernández-Del Castillo C, Kamisawa T, Jang JY, Levy P, Ohtsuka T, Salvia R, Shimizu Y, Tada M, Wolfgang CL. Revisions of international consensus Fukuoka guidelines for the management of IPMN of the pancreas. Pancreatology. 2017;17:738-753. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 868] [Cited by in RCA: 1157] [Article Influence: 144.6] [Reference Citation Analysis (1)] |
| 6. | Ohtsuka T, Fernandez-Del Castillo C, Furukawa T, Hijioka S, Jang JY, Lennon AM, Miyasaka Y, Ohno E, Salvia R, Wolfgang CL, Wood LD. International evidence-based Kyoto guidelines for the management of intraductal papillary mucinous neoplasm of the pancreas. Pancreatology. 2024;24:255-270. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 74] [Cited by in RCA: 140] [Article Influence: 140.0] [Reference Citation Analysis (1)] |
| 7. | European Study Group on Cystic Tumours of the Pancreas. European evidence-based guidelines on pancreatic cystic neoplasms. Gut. 2018;67:789-804. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1006] [Cited by in RCA: 896] [Article Influence: 128.0] [Reference Citation Analysis (1)] |
| 8. | Vege SS, Ziring B, Jain R, Moayyedi P; Clinical Guidelines Committee; American Gastroenterology Association. American gastroenterological association institute guideline on the diagnosis and management of asymptomatic neoplastic pancreatic cysts. Gastroenterology. 2015;148:819-22; quize12. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 629] [Cited by in RCA: 759] [Article Influence: 75.9] [Reference Citation Analysis (1)] |
| 9. | Basturk O, Hong SM, Wood LD, Adsay NV, Albores-Saavedra J, Biankin AV, Brosens LA, Fukushima N, Goggins M, Hruban RH, Kato Y, Klimstra DS, Klöppel G, Krasinskas A, Longnecker DS, Matthaei H, Offerhaus GJ, Shimizu M, Takaori K, Terris B, Yachida S, Esposito I, Furukawa T; Baltimore Consensus Meeting. A Revised Classification System and Recommendations From the Baltimore Consensus Meeting for Neoplastic Precursor Lesions in the Pancreas. Am J Surg Pathol. 2015;39:1730-1741. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 582] [Cited by in RCA: 578] [Article Influence: 57.8] [Reference Citation Analysis (0)] |
| 10. | Yamao K, Takenaka M, Ishikawa R, Okamoto A, Yamazaki T, Nakai A, Omoto S, Kamata K, Minaga K, Matsumoto I, Takeyama Y, Numoto I, Tsurusaki M, Chikugo T, Chiba Y, Watanabe T, Kudo M. Partial Pancreatic Parenchymal Atrophy Is a New Specific Finding to Diagnose Small Pancreatic Cancer (≤10 mm) Including Carcinoma in Situ: Comparison with Localized Benign Main Pancreatic Duct Stenosis Patients. Diagnostics (Basel). 2020;10. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 29] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 11. | Furuya N, Yamaguchi A, Kato N, Sugata S, Hamada T, Mizumoto T, Tamaru Y, Kusunoki R, Kuwai T, Kouno H, Kuraoka K, Shibata Y, Tazuma S, Sudo T, Kohno H, Oka S. High-grade pancreatic intraepithelial neoplasia diagnosed based on changes in magnetic resonance cholangiopancreatography findings: A case report. World J Clin Cases. 2024;12:1487-1496. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 5] [Reference Citation Analysis (1)] |
| 12. | Iiboshi T, Hanada K, Fukuda T, Yonehara S, Sasaki T, Chayama K. Value of cytodiagnosis using endoscopic nasopancreatic drainage for early diagnosis of pancreatic cancer: establishing a new method for the early detection of pancreatic carcinoma in situ. Pancreas. 2012;41:523-529. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 87] [Cited by in RCA: 93] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 13. | Nakamura S, Ishii Y, Serikawa M, Hanada K, Eguchi N, Sasaki T, Fujimoto Y, Yamaguchi A, Sugiyama S, Noma B, Kamigaki M, Minami T, Okazaki A, Yukutake M, Mouri T, Tatsukawa Y, Ikemoto J, Arihiro K, Oka S. Diagnostic Ability and Safety of Repeated Pancreatic Juice Cytology Using an Endoscopic Nasopancreatic Drainage Catheter for Pancreatic Ductal Adenocarcinoma: A Multicenter Prospective Study. Diagnostics (Basel). 2023;13. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 14. | Kawada N, Uehara H, Nagata S, Tomita Y, Nakamura H. Pancreatic juice cytology as sensitive test for detecting pancreatic malignancy in intraductal papillary mucinous neoplasm of the pancreas without mural nodule. Pancreatology. 2016;16:853-858. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 15. | Kato S, Zakimi M, Yamada K, Chinen K, Kubota T, Arashiro M, Kikuchi K, Murakami T, Kunishima F. Efficacy of repeated cytology of pancreatic juice obtained by endoscopic nasopancreatic drainage tube for early diagnosis of pancreatic cancer: a case series including a case of carcinoma in situ. Clin J Gastroenterol. 2015;8:240-246. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 16. | Matsubayashi H, Canto M, Sato N, Klein A, Abe T, Yamashita K, Yeo CJ, Kalloo A, Hruban R, Goggins M. DNA methylation alterations in the pancreatic juice of patients with suspected pancreatic disease. Cancer Res. 2006;66:1208-1217. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 150] [Cited by in RCA: 159] [Article Influence: 8.4] [Reference Citation Analysis (0)] |