Published online Jun 6, 2024. doi: 10.12998/wjcc.v12.i16.2911
Revised: March 2, 2024
Accepted: April 1, 2024
Published online: June 6, 2024
Processing time: 99 Days and 9.4 Hours
Transarterial chemoembolization (TACE) is a standard treatment for inter
A 42-year-old man came to our hospital with cough and expectoration for 1 month after TACE for HCC. Laboratory test results showed abnormalities of albumin, hemoglobin, prothrombin time, C-reactive protein, D-dimer, and prothrombin. Culture of both phlegm and liver pus revealed growth of Citrobacter flavescens. Computed tomography showed infection in the inferior lobe of the right lung and a low-density lesion with gas in the right liver. Liver ultrasound showed that there was a big hypoechoic liquid lesion without blood flow signal. Drainage for liver abscess by needle puncture under ultrasonic guidance was performed. After 1 month of drainage and anti-infection therapy, the abscess in the liver and the infection in the lung were reduced obviously, and the symptom of expectoration was relieved.
Clinicians should be alert to the possibility of complications of liver abscess and tracheal fistula after TACE for HCC. Drainage for liver abscess by needle puncture under ultrasonic guidance could relieve the liver abscess and tracheal fistula.
Core Tip: Transarterial chemoembolization (TACE) is commonly used for treating hepatocellular carcinoma (HCC). The complications of TACE include liver rupture, liver abscess, etc. We report a patient treated with TACE for HCC who developed liver abscess and tracheal fistula. Drainage for liver abscess by needle puncture under ultrasonic guiding could relieve the liver abscess.
- Citation: Zhang FL, Xu J, Jiang YH, Zhu YD, Wu QN, Shi Y, Zhu FY, Chen JW, Wu LX. Liver abscess and tracheal fistula induced by transcatheter arterial chemoembolization for hepatocellular carcinoma: A case report. World J Clin Cases 2024; 12(16): 2911-2916
- URL: https://www.wjgnet.com/2307-8960/full/v12/i16/2911.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i16.2911
Hepatocellular carcinoma (HCC) ranks as the world's fifth most prevalent cancer and the third leading cause of cancer-related deaths[1]. Transarterial chemoembolization (TACE) is commonly used for treating intermediate-stage HCC[2]. The complications of TACE include liver rupture, liver abscess, femoral artery pseudoaneurysm, cholecystitis, biloma, pulmonary embolism, cerebral lipiodol embolism, tumor lysis syndrome, partial intestinal obstruction, and gallbladder perforation[3]. TACE has been known to cause tracheal fistula in a few patients treated with this procedure.
A 42-year-old man presented with symptoms of cough and expectoration for 1 month.
The patient did not have any previous pulmonary diseases such as coughing.
TACE was performed for HCC 1 month ago. Two years earlier, the patient suffered from hepatitis B liver cirrhosis and was administered oral entecavir daily for antiviral treatment.
The patient had no history of high blood pressure, diabetes, or heart disease. His family was free from any cancerous conditions.
Clinical assessments revealed a diseased liver, absence of skin or sclera discoloration, clear respiratory sounds during auscultation of both lungs, no signs of dry or wet rales, a heart rate of 76 beats per minute, consistent heart rhythm, a soft abdomen, absence of tenderness or rebound pain, accessible 1 cm beneath the ribs of the right clavicular line of the liver and spleen, and no swelling in either lower extremity.
The stool and urine tests showed no abnormality. Laboratory test results showed that white blood cell count, platelet count, prothrombin time, total bilirubin, alanine aminotransferase, creatinine, alpha-fetoprotein, carcinoembryonic antigen, carbohydrate antigen 19-9, triglyceride, cholesterol, amylase, lipase, and glucose were all within normal range (Table 1). Albumin, hemoglobin, C-reactive protein, prothrombin, and D-dimer were abnormal (Table 1). Hepatitis B surface antigen was positive. Hepatitis C antibody, human immunodefciency virus antibody, syphilis antibody, and anti-nuclear antibodies were all negative.
| Laboratory result | Normal range | |
| WBC (× 109/L) | 4.54 | 3.4-9.5 |
| Hb (g/L) | 116 | 120-150 |
| Platelets (× 109/L) | 136 | 125-350 |
| PT (s) | 12.8 | 9.7-12.6 |
| D-dimer (mg/L) | 0.57 | 0.00-0.55 |
| ALT (U/L) | 18 | 9-50 |
| TB (μmol/L) | 11.27 | 3-20 |
| ALB (g/L) | 33.4 | 40-55 |
| Cr (μmol/L) | 45 | 40-80 |
| CA19-9 (kU/L) | 21 | 0-35 |
| CEA (μg/L) | 2.19 | 0-5 |
| AFP (μg/L) | 4.43 | 0-9 |
| ABP (mAU/mL) | 1522 | 10-14 |
| CRP (mg/L) | 12 | 0-10 |
| Triglyceride (mmol/L) | 0.49 | 0-1.7 |
| Cholesterol (mmol/L) | 2.9 | 2.86-5.98 |
| Amylase (U/L) | 110 | 35-135 |
| Lipase (U/L) | 89 | 0-190 |
| Glucose (mmol/L) | 5.4 | 3.0-6.1 |
| Culture of phlegm | Citrobacter flavescens | |
| Culture of liver pus | Citrobacter flavescens | |
| HbsAg | Positive | Negative |
| HIV Ab | Negative | Negative |
| Sp Ab | Negative | Negative |
| ANA | Negative | Negative |
| HC Ab | Negative | Negative |
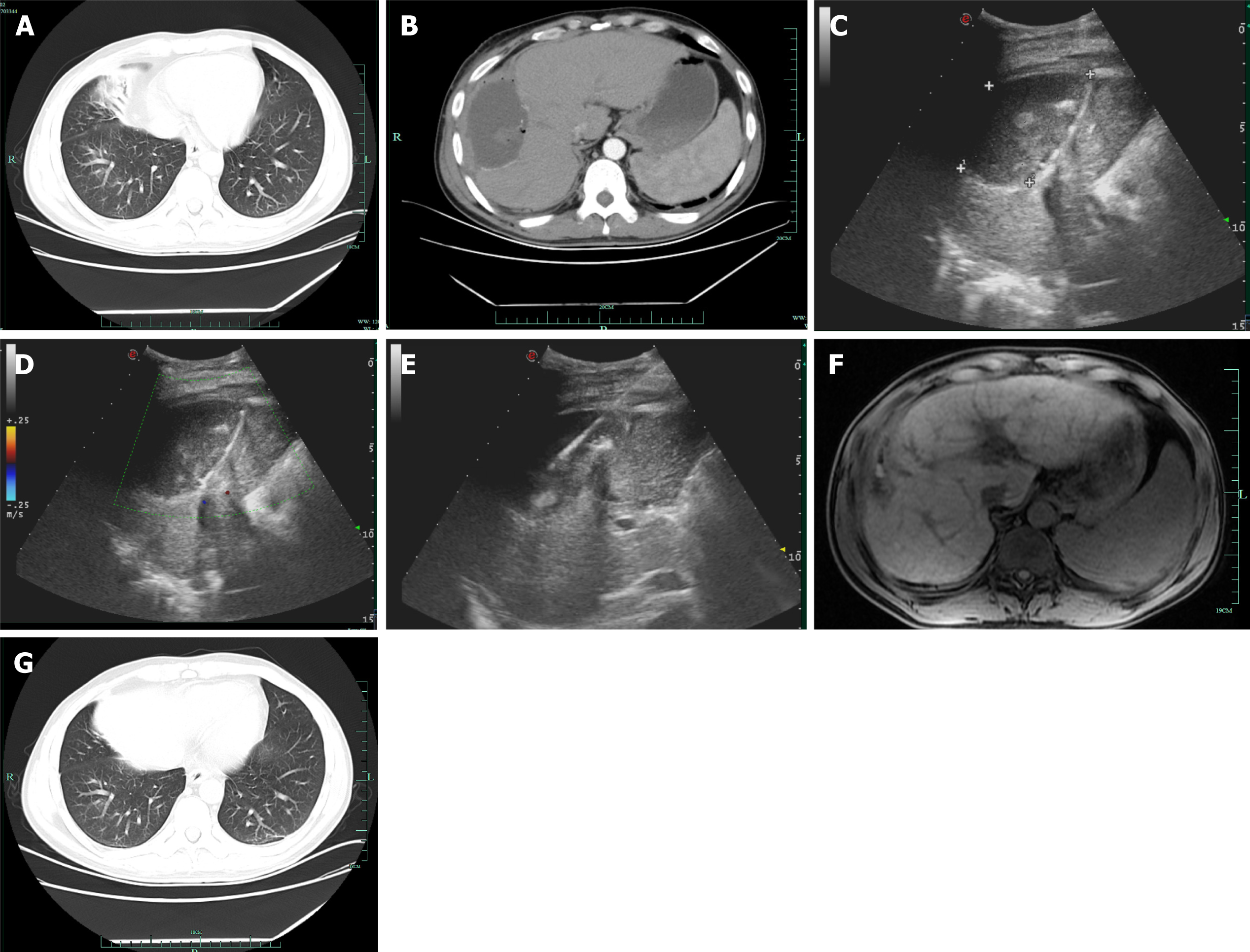
Culture of both phlegm and liver pus revealed growth of Citrobacter flavescens. Computed tomography showed infection in the inferior lobe of the right lung (Figure 1A) and a low density lesion with gas in the right liver (Figure 1B). Liver ultrasound showed that there was a big hypoechoic liquid lesion (Figure 1C) without blood flow signal (Figure 1D). Drainage for liver abscess by needle puncture under ultrasonic guidance was performed (Figure 1E). After 1 month of drainage and systemic antibiotic treatment, the abscess in the liver (Figure 1F) and the infection in the lung (Figure 1G) were reduced obviously, and the symptom of expectoration was relieved.
Liver abscess and tracheal fistula.
Drainage of the liver abscess and systemic antibiotic treatment were performed for 1 month.
The abscess in the liver (Figure 1F) and infection in the lung (Figure 1G) were reduced obviously, and the symptom of expectoration was relieved.
Multiple complications have been linked to TACE, such as postembolization syndrome, liver failure, liver infarction, liver abscess, biliary necrosis, cholecystitis, skin injuries, and adrenal bleeding[4-6]. Of these complications, liver abscess is known to be able to lead to a severe illness, extended hospital stays, and a high risk of death[7,8]. The occurrence of liver abscesses following liver chemoembolization is uncommon, yet it has been documented in earlier research. Reed et al[9] documented that out of 227 patients, 6 (2.6%) developed liver abscesses post-chemoembolization. Liver abscesses have the potential to burst into the gastrointestinal, pericardial, and peritoneal spaces[10-12]; yet, the occurrence of fistula in the trachea is uncommon, with only a handful of hepatogastric fistula cases documented[13,14]. The combination of percutaneous catheter drainage and systemic antibiotics stands as the predominant method for treating hepatic abscesses[15,16].
In this case, after 1 month of drainage and systemic antibiotic treatment, the abscess in the liver and the infection in the lung were reduced obviously, and the symptom of expectoration was relieved. The reasons for the abscess and tracheal fistula induced by TACE may be as follow: (1) Necrosis and liquefaction of the tumor occur after TACE; (2) the normal cells in the liver were injured and accompanied with inflammatory exudation; (3) the location of TACE was near the diaphragm, and the chemoembolization may injure the diaphragm; and (4) the abscess may gradually invades the diaphragm and trachea.
Clinicians should be alert to the possibility of complications of abscess and tracheal fistula after TACE for HCC. Drainage for liver abscess by needle puncture under ultrasonic guidance could relieve the liver abscess and tracheal fistula.
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): 0
Grade D (Fair): D, D, D, D
Grade E (Poor): 0
| 1. | Livraghi T, Mäkisalo H, Line PD. Treatment options in hepatocellular carcinoma today. Scand J Surg. 2011;100:22-29. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 76] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 2. | Tan J, Fan W, Liu T, Zhu B, Liu Y, Wang S, Wu J, Liu J, Zou F, Wei J, Liu L, Zhang X, Zhuang J, Wang Y, Lin H, Huang X, Chen S, Kuang M, Li J. TREM2(+) macrophages suppress CD8(+) T-cell infiltration after transarterial chemoembolisation in hepatocellular carcinoma. J Hepatol. 2023;79:126-140. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 87] [Article Influence: 43.5] [Reference Citation Analysis (0)] |
| 3. | Tu J, Jia Z, Ying X, Zhang D, Li S, Tian F, Jiang G. The incidence and outcome of major complication following conventional TAE/TACE for hepatocellular carcinoma. Medicine (Baltimore). 2016;95:e5606. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 48] [Cited by in RCA: 65] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 4. | Chung JW, Park JH, Han JK, Choi BI, Han MC, Lee HS, Kim CY. Hepatic tumors: predisposing factors for complications of transcatheter oily chemoembolization. Radiology. 1996;198:33-40. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 256] [Cited by in RCA: 259] [Article Influence: 8.9] [Reference Citation Analysis (0)] |
| 5. | Farinati F, De Maria N, Marafin C, Herszènyi L, Del Prato S, Rinaldi M, Perini L, Cardin R, Naccarato R. Unresectable hepatocellular carcinoma in cirrhosis: survival, prognostic factors, and unexpected side effects after transcatheter arterial chemoembolization. Dig Dis Sci. 1996;41:2332-2339. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 55] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 6. | Gates J, Hartnell GG, Stuart KE, Clouse ME. Chemoembolization of hepatic neoplasms: safety, complications, and when to worry. Radiographics. 1999;19:399-414. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 92] [Cited by in RCA: 83] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 7. | de Baère T, Roche A, Amenabar JM, Lagrange C, Ducreux M, Rougier P, Elias D, Lasser P, Patriarche C. Liver abscess formation after local treatment of liver tumors. Hepatology. 1996;23:1436-1440. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 83] [Cited by in RCA: 66] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 8. | Hashimoto T, Mitani T, Nakamura H, Hori S, Kozuka T, Kobayashi Y, Nakata A, Tsujimura T. Fatal septic complication of transcatheter chemoembolization for hepatocellular carcinoma. Cardiovasc Intervent Radiol. 1993;16:325-327. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 19] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 9. | Reed RA, Teitelbaum GP, Daniels JR, Pentecost MJ, Katz MD. Prevalence of infection following hepatic chemoembolization with cross-linked collagen with administration of prophylactic antibiotics. J Vasc Interv Radiol. 1994;5:367-371. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 36] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 10. | Hsu CY, Liu JH, Su CW. Hepatogastric fistula in one patient with liver abscess. Gastroenterology. 2009;137:e7-e8. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 11. | Chan KS, Chen CM, Cheng KC, Hou CC, Lin HJ, Yu WL. Pyogenic liver abscess: a retrospective analysis of 107 patients during a 3-year period. Jpn J Infect Dis. 2005;58:366-368. [PubMed] |
| 12. | Monge-Fresse AS, Siriez JY, Bricaire F. Spontaneous fistulisation of a liver abscess into the stomach. Neth J Med. 2007;65:456-457. [PubMed] |
| 13. | Dai H, Cui D, Li D, Zhai BO, Zhang J. Hepatic abscess with hepatobronchial fistula following percutaneous radiofrequency ablation for hepatocellular carcinoma: A case report. Oncol Lett. 2015;9:2289-2292. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 14. | Kim DH, Choi DW, Choi SH, Heo JS, Jeong J, Rhu J. Surgical treatment of bronchobiliary fistula due to radiofrequency ablation for recurrent hepatocellular carcinoma. Korean J Hepatobiliary Pancreat Surg. 2013;17:135-138. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 12] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 15. | Lambiase RE, Deyoe L, Cronan JJ, Dorfman GS. Percutaneous drainage of 335 consecutive abscesses: results of primary drainage with 1-year follow-up. Radiology. 1992;184:167-179. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 151] [Cited by in RCA: 117] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 16. | Bamberger DM. Outcome of medical treatment of bacterial abscesses without therapeutic drainage: review of cases reported in the literature. Clin Infect Dis. 1996;23:592-603. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 63] [Article Influence: 2.2] [Reference Citation Analysis (0)] |