Published online Jun 6, 2024. doi: 10.12998/wjcc.v12.i16.2856
Revised: April 4, 2024
Accepted: April 19, 2024
Published online: June 6, 2024
Processing time: 149 Days and 5.3 Hours
Varicocele embolization, a minimally invasive treatment for symptomatic varicoceles, carries a rare risk of complications like ureteral obstruction and hydronephrosis. This case report documents such a case to raise awareness of these potential complications and showcase minimally invasive surgical mana
A 35-year-old male presented with flank pain and hematuria following varicocele embolization. Imaging confirmed left ureteral obstruction and hydronephrosis. Laparoscopic ureterolysis successfully removed the embolization coil and re
Minimally invasive surgery offers an effective treatment option for rare complications like ureteral obstruction arising from varicocele embolization.
Core Tip: Varicocele embolization is a minimally invasive procedure that is generally considered safe, but complications can occur, such as ureteral obstruction and hydronephrosis. It is important to be aware of the potential complications of varicocele embolization, even though they are rare. Minimally invasive surgery can be used to successfully treat the complications of varicocele embolization. If a patient develops flank pain and hematuria following varicocele embolization, imaging studies should be performed to rule out ureteral obstruction and hydronephrosis. If the ureteral obstruction is diagnosed, minimally invasive surgery can be performed to remove the obstructing coil and repair the ureter.
- Citation: Alamri A. Migration of varicocele coil leading to ureteral obstruction and hydronephrosis: A case report. World J Clin Cases 2024; 12(16): 2856-2861
- URL: https://www.wjgnet.com/2307-8960/full/v12/i16/2856.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i16.2856
In order to treat symptomatic varicoceles, a well-proven treatment called varicocele embolization is employed. It entails the percutaneous insertion of embolic material into the varicocele's dilated veins, such as coils or sclerosants[1,2]. A new generation of hydrogel-coated platinum coils has been developed as a result of recent technical developments in interventional neuroradiology embolization. The coil may grow up to three times its initial volume because to its hydrogel covering A very stable and long-lasting platform for blood stasis and thrombus development is provided by the combination of a platinum coil and an expanding hydrogel polymer[3]. Despite being regarded as a safe technique, a number of issues, such as embolic material migration, have been recorded. Here, we present a case of ureteral blockage brought on by a migrating varicocele coil that led to hydronephrosis.
A 35-year-old male patient presented with progressive left-sided flank pain for several years. The pain was mild, lasting only a few minutes and non-radiating. It was not associated with any voiding symptoms or gastrointestinal complaints. The patient also reported intermittent hematuria, with periods of no blood in the urine and no accompanying pain.
The patient underwent varicocele embolization 11 years prior to presentation to alleviate testicular discomfort and swelling. His post-operative period was uneventful. However, several years later, he developed the aforementioned left-sided flank pain.
No significant past medical history was reported.
The patient denied any history of tobacco use, alcohol abuse, or recreational drug use. Family history was unremarkable for any relevant conditions.
Physical examination revealed no flank tenderness, abdominal distention, or other obvious signs of distress.
Laboratory investigations, including renal function tests and urinalysis, were unremarkable.
Kidneys, ureters and urinary bladder (KUB) (plain abdominal X-ray): Revealed bilateral refilling of the coils from the previous varicocele surgery (Figure 1).
Ultrasound imaging of the KUB abdomen: Demonstrated moderate left hydronephrosis and hydro-ureter. The ultrasound showed a dilated pelvicalcyceal system as branching, interconnected areas of decreased echogenicity in the renal collecting system (Figure 2).
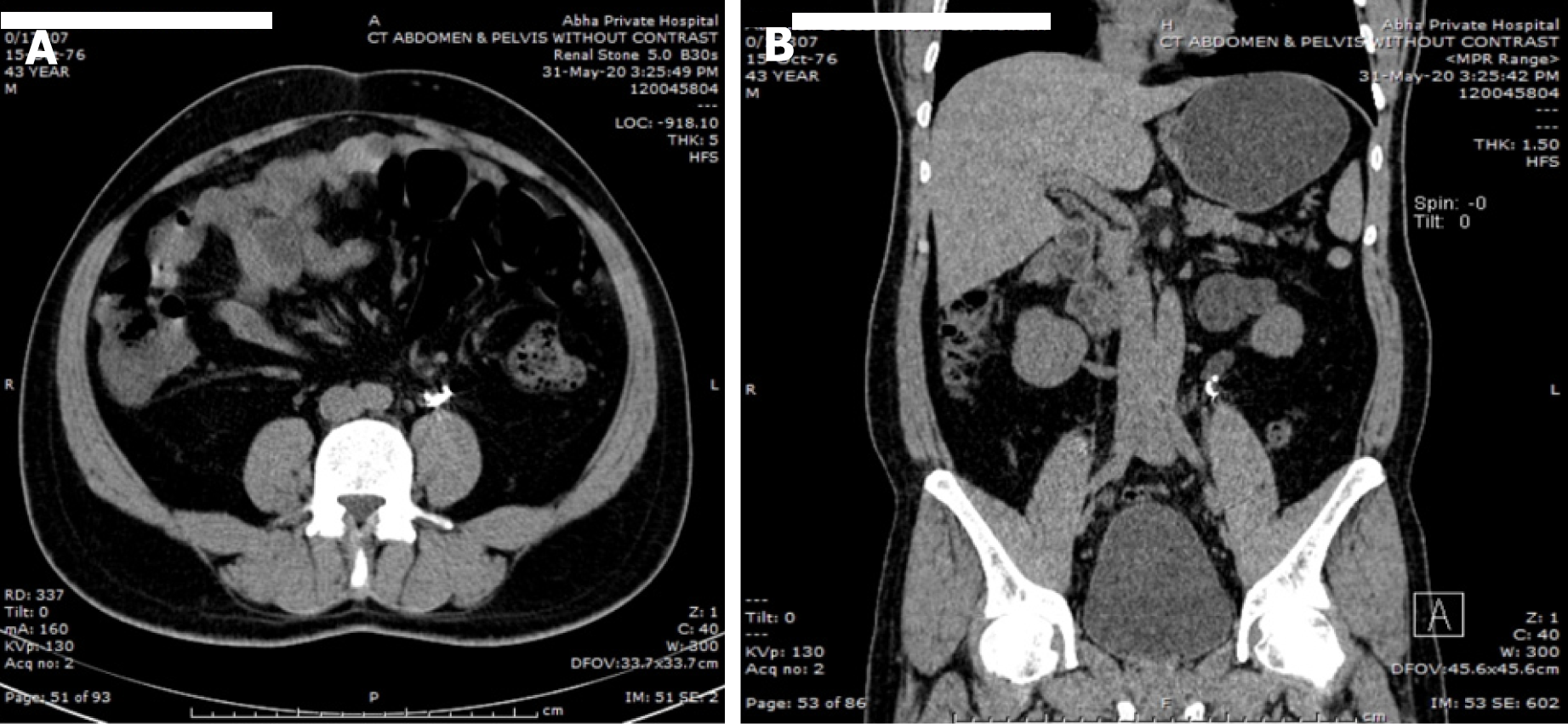
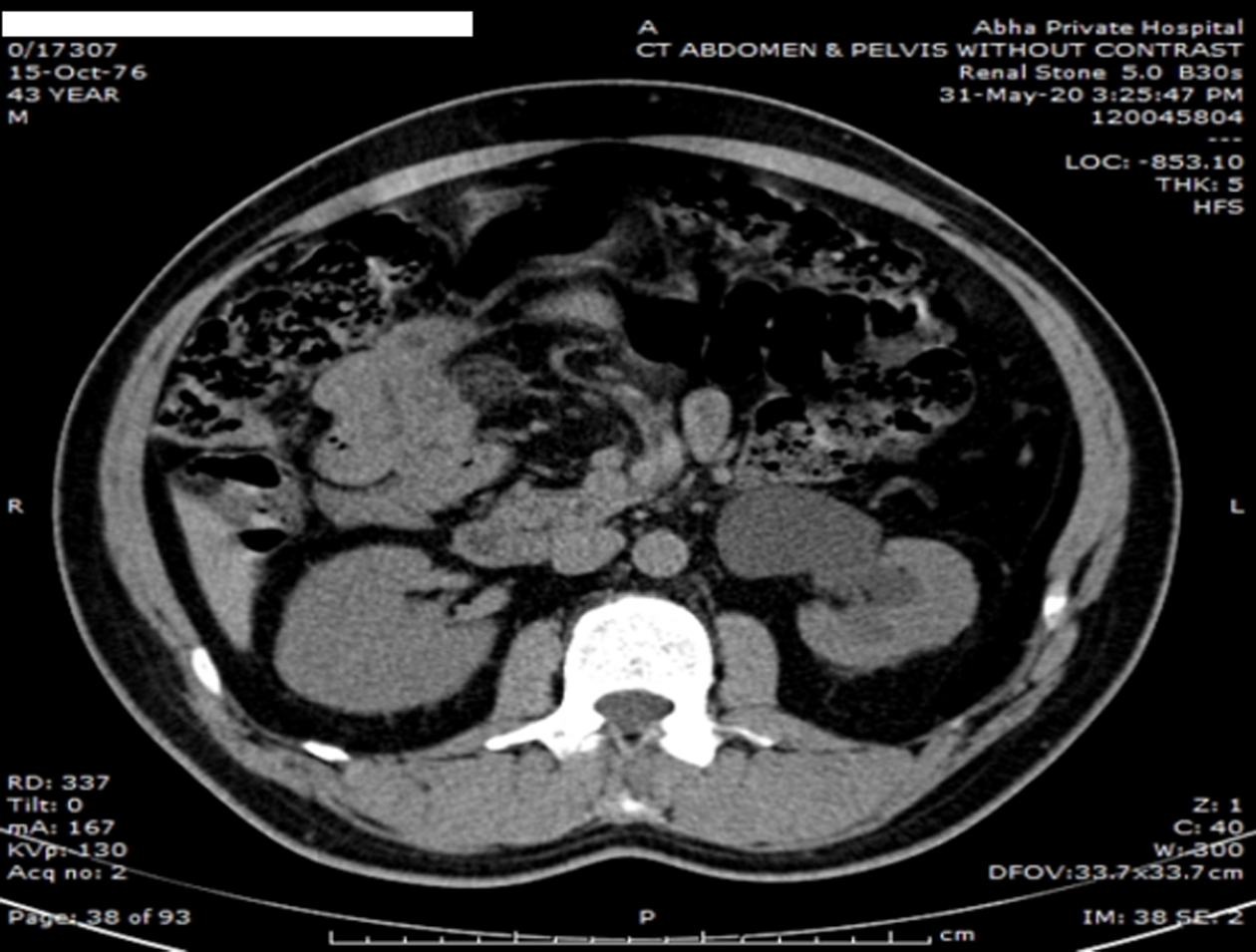
Contrast-enhanced computed tomography (CT) of the abdomen and pelvis: Revealed a migrated varicocele coil within the distal left ureter, causing luminal narrowing and subsequent hydronephrosis. No evidence of ureteral perforation or surrounding infection was observed. The proximal ureter appeared dilated, and the ipsilateral kidney showed moderate hydronephrosis (Figures 3 and 4).
In the case of migration of a varicocele coil leading to ureteral obstruction and hydronephrosis, several differential diagnoses should be considered. These include urolithiasis (kidney stone), ureteral stricture, retroperitoneal fibrosis, ureteral tumor, ureteral injury, and other causes of ureteral obstruction, blood clots, ureteral strictures, or congenital abnormalities. It is important to conduct a thorough clinical evaluation, including a detailed clinical history, physical examination, and appropriate imaging studies, to arrive at an accurate diagnosis. Collaboration with urologist would be crucial for further therapeutic management and treatment of the patient.
Migration of varicocele coil leading to left ureteral obstruction and hydronephrosis.
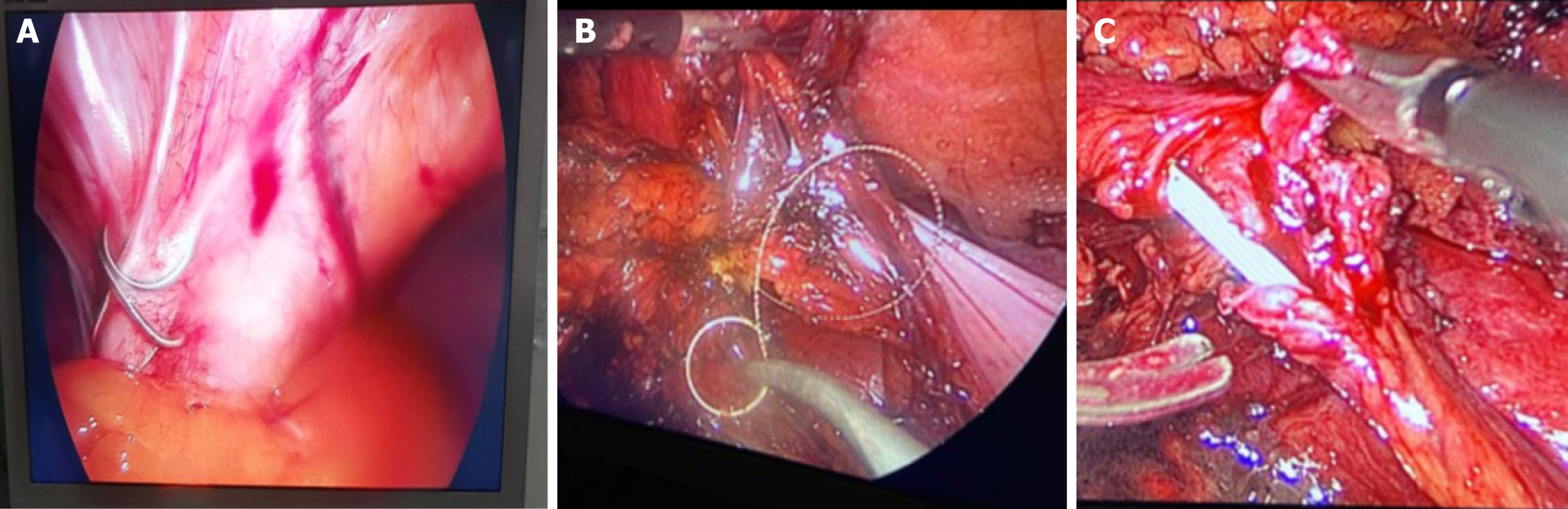
The patient was referred to urologist for further management. Given his symptoms and imaging findings, the decision was made to intervene surgically to remove the migrated coil and relieve the ureteral obstruction. Under general anaesthesia, the patient underwent a laparoscopic ureterolysis using a left retroperitoneal approach. Access to the pelvis was achieved using a 10 mm umbilical trocar for the camera, another 10 mm trocar at the mid-clavicle line for the right-hand port, a 5 mm left hand port located approximately 8 cm superior to the camera port in the same midline, and finally a 5 mm port placed laterally at the anterior axillary line for tissue traction and insertion of the double-J stent during the procedure. This was followed by ureteric resection of the compressed narrowed part (approximately 2 cm). The migrated coil was visualized intraoperatively as shown in Figure 5. Finally, an end-to-end anastomosis was performed over a stent. A drain was placed for 2 d, and the patient was discharged the following day.
The postoperative recovery was uneventful with no complications. The patient's flank pain resolved shortly after surgery. A follow-up ultrasound imaging and CT scan at three months post-surgery showed complete resolution of hydro
The umbilical trocar is used for a 10-mm camera, another 10-mm camera is located in the midclavicular line for the right-hand port, and a 5-mm left-hand port is located approximately 8 cm above the camera port in the same midline. Finally a 5-mm port was used laterally at the anterior axillary line to help for tissue traction and insertion of the double j stent during the procedure, it was followed by ureteric resection of the compressed narrowed part (about 2 cm). The coils can be seen in intra operative pictures as shown in Figure 5. Finally, end to end anastomosis was done over a stent. Drain was kept for 2 d and patient was discharged the next day.
A pampiniform venous plexus that is abnormally twisted and dilated inside the spermatic cord is known as a varicocele. In the overall male population, varicocele is thought to affect 15% of population. In males with primary infertility, its frequency rises with age and can reach 35%[4]. One of the most typical factors contributing to men's reversible infertility is varicocele. Men with varicocele are thought to have many significant therapy options, including varicocelectomy and percutaneous embolization of the gonadal vein[5]. With just minimal sedation needed, percutaneous embolization provides a less invasive, nonsurgical approach for the treatment of varicoceles. The gonadal vein and collateral venous supplies can also be identified during the surgery by using diagnostic venography[4].
Varicocele embolization is a frequently used procedure with a low risk of complications. Hydronephrosis and ureteral obstruction can result from embolic material migration, a rare but potentially serious side effect[6,7]. The two major treatments for males with varicocele are surgical ligation and percutaneous embolization of the internal spermatic vein[8]. Percutaneous embolization is less expensive and less intrusive than surgical ligation; it just needs local anesthesiology and provides visibility of the interior spermatic vein and any potential collaterals[9,10]. Several embolic materials have been utilized, with coils being the most popular and glue becoming a more popular substitute[11,12].
Varicocele coil migration is a rather uncommon complication, with few occurrences having been documented in the literature[13]. As observed in our example, coil migration might happen right away following the embolization treatment or months later. The precise cause of migration is unknown, however it is believed to be connected to the coil's design, the anatomy of the patient, or technical aspects of the embolization technique[14].
This case report demonstrates how important is to closely follow patients who have had varicocele embolization and to assess them as soon as any new or worsening symptoms appear. For obtaining an accurate diagnosis and creating a treatment plan, ultrasound and CT imaging modalities are essential. When migrating coils restrict the ureter because of the obstruction the coils produce, surgery can be required.
The unhindered ureter's subsequent alterations in cytokine/chemokine and lymphocyte levels point to the existence of crosstalk caused by a systemic immune response. It may be crucial to stop obstruction-induced ureteral remodeling to avoid long-term problems[14].
This case report of varicocele coil migration causing ureteral blockage and hydronephrosis is unique. Only few similar case reports were noted.
Retrieving the migrated coil and alleviating ureteral obstruction are required for the management of varicocele coil migration. There are several methods that can be used, such as surgical intervention, endourological methods, or cystoscopic retrieval. The position of the migrated coil, patient characteristics, and surgeon experience all influence the therapeutic option.
It is an uncommon but potentially dangerous consequence when varicocele embolization coils migrate, causing ureteral blockage and hydronephrosis. This illness can be effectively managed with prompt diagnosis and proper care, including surgical interventions. When examining patients who have persistent or getting worse symptoms after varicocele embolization, clinician should be aware of this possible consequence and take it into consideration in the differential diagnosis. In order to reduce the risk of coil migration and improve patient outcomes, more research is required.
| 1. | Wadhwa V, Kashanian JA, Schiffman M, McClure TD. Varicocele Embolization: Patient Selection: Preprocedure Workup, and Technical Considerations. Semin Intervent Radiol. 2021;38:176-181. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 2. | Bilreiro C, Donato P, Costa JF, Agostinho A, Carvalheiro V, Caseiro-Alves F. Varicocele embolization with glue and coils: A single center experience. Diagn Interv Imaging. 2017;98:529-534. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 16] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 3. | Ding YH, Dai D, Lewis DA, Cloft HJ, Kallmes DF. Angiographic and histologic analysis of experimental aneurysms embolized with platinum coils, Matrix, and HydroCoil. AJNR Am J Neuroradiol. 2005;26:1757-1763. [PubMed] |
| 4. | Alsaikhan B, Alrabeeah K, Delouya G, Zini A. Epidemiology of varicocele. Asian J Androl. 2016;18:179-181. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 193] [Cited by in RCA: 160] [Article Influence: 17.8] [Reference Citation Analysis (0)] |
| 5. | Agarwal A, Deepinder F, Cocuzza M, Agarwal R, Short RA, Sabanegh E, Marmar JL. Efficacy of varicocelectomy in improving semen parameters: new meta-analytical approach. Urology. 2007;70:532-538. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 237] [Cited by in RCA: 211] [Article Influence: 11.7] [Reference Citation Analysis (0)] |
| 6. | Varicocele embolization. Chelsea and Westminster Hospital NHS Foundation Trust. Available from: https://www.chelwest.nhs.uk/your-visit/patient-leaflets/imaging/varicocele-embolisation. |
| 7. | Pauroso S, Di Leo N, Fulle I, Di Segni M, Alessi S, Maggini E. Varicocele: Ultrasonographic assessment in daily clinical practice. J Ultrasound. 2011;14:199-204. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 21] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 8. | Urbano J, Cabrera M, Alonso-Burgos A. Sclerosis and varicocele embolization with N-butyl cyanoacrylate: experience in 41 patients. Acta Radiol. 2014;55:179-185. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 24] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 9. | Iaccarino V, Venetucci P. Interventional radiology of male varicocele: current status. Cardiovasc Intervent Radiol. 2012;35:1263-1280. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 29] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 10. | Favard N, Moulin M, Fauque P, Bertaut A, Favelier S, Estivalet L, Michel F, Cormier L, Sagot P, Loffroy R. Comparison of three different embolic materials for varicocele embolization: retrospective study of tolerance, radiation and recurrence rate. Quant Imaging Med Surg. 2015;5:806-814. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 10] [Reference Citation Analysis (0)] |
| 11. | Pietura R, Toborek M, Dudek A, Boćkowska A, Janicka J, Piekarski P. Endovascular embolization of varicoceles using n-butyl cyanoacrylate (NBCA) glue. Pol J Radiol. 2013;78:26-30. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 10] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 12. | Karia N, Balmforth D, Lall K, Gupta S, Bhattacharyya S. Migration of a Varicocele Coil to the Right Heart. JACC Case Rep. 2020;2:2312-2317. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 4] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 13. | Perdikakis E, Fezoulidis I, Tzortzis V, Rountas C. Varicocele embolization: Anatomical variations of the left internal spermatic vein and endovascular treatment with different types of coils. Diagn Interv Imaging. 2018;99:599-607. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 14. | Reicherz A, Eltit F, Almutairi K, Mojtahedzadeh B, Herout R, Chew B, Cox M, Lange D. Ureteral Obstruction Promotes Ureteral Inflammation and Fibrosis. Eur Urol Focus. 2023;9:371-380. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 7] [Reference Citation Analysis (0)] |