Published online Jun 6, 2024. doi: 10.12998/wjcc.v12.i16.2842
Revised: February 25, 2024
Accepted: April 8, 2024
Published online: June 6, 2024
Processing time: 163 Days and 23.8 Hours
Xanthomatosis, a metabolic disorder causing yellow growths (xanthomas), poses challenges in lipid metabolism. This case study introduces the first documented instance within China's Yi population, emphasizing the need to explore dietary habits and treatment strategies tailored to this specific community.
Xanthomatosis is a metabolic disorder where lipid metabolism goes awry, re
The first report of xanthomatosis in the Yi population in China lays a theoretical foundation for understanding Yi dietary patterns and treatment.
Core Tip: Xanthomatosis, a metabolic disorder causing yellow growths (xanthomas), poses challenges in lipid metabolism. This case study introduces the first documented instance within China's Yi population, emphasizing the need to explore dietary habits and treatment strategies tailored to this specific community.
- Citation: Ren C, Zhu L, Niu YC, Tu LY, Jin ZF, Zhang J. Eruptive xanthomas in a patient with severe hypertriglyceridemia: A case report. World J Clin Cases 2024; 12(16): 2842-2846
- URL: https://www.wjgnet.com/2307-8960/full/v12/i16/2842.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i16.2842
Xanthomatosis is a metabolic disorder where lipid metabolism goes awry, resulting in the development of yellowish growths called xanthomas.
A 47-year-old male patient of Yi in China with obesity presented to our dermatology clinic with generalized asym
The lesions had appeared on his arms two weeks earlier and had spread to his trunk, buttocks and legs. He had not taken medications around the time of rash onset. He worked as a chef and had a diet that was often oily and greasy. There were no similar cases of illness in his family members.
He had not taken medications around the time of rash onset.
He worked as a chef and had a diet that was often oily and greasy. There were no similar cases of illness in his family members.
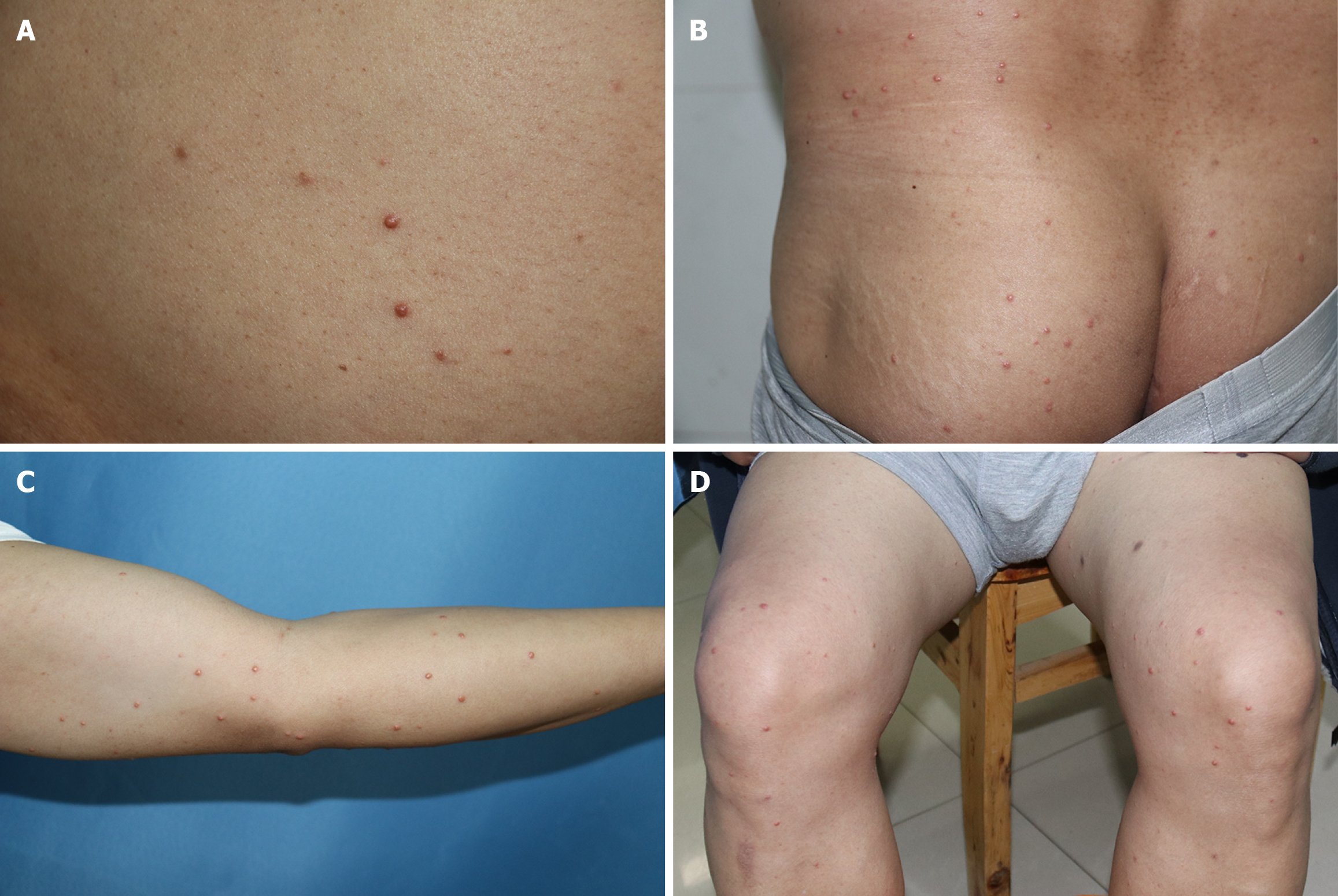
On physical examination, crops of firm reddish-yellow papules (diameter 1-3 mm) distributed on the patient’s trunk, extensor surfaces of the extremities and buttocks, suggestive of eruptive xanthomas (Figure 1).
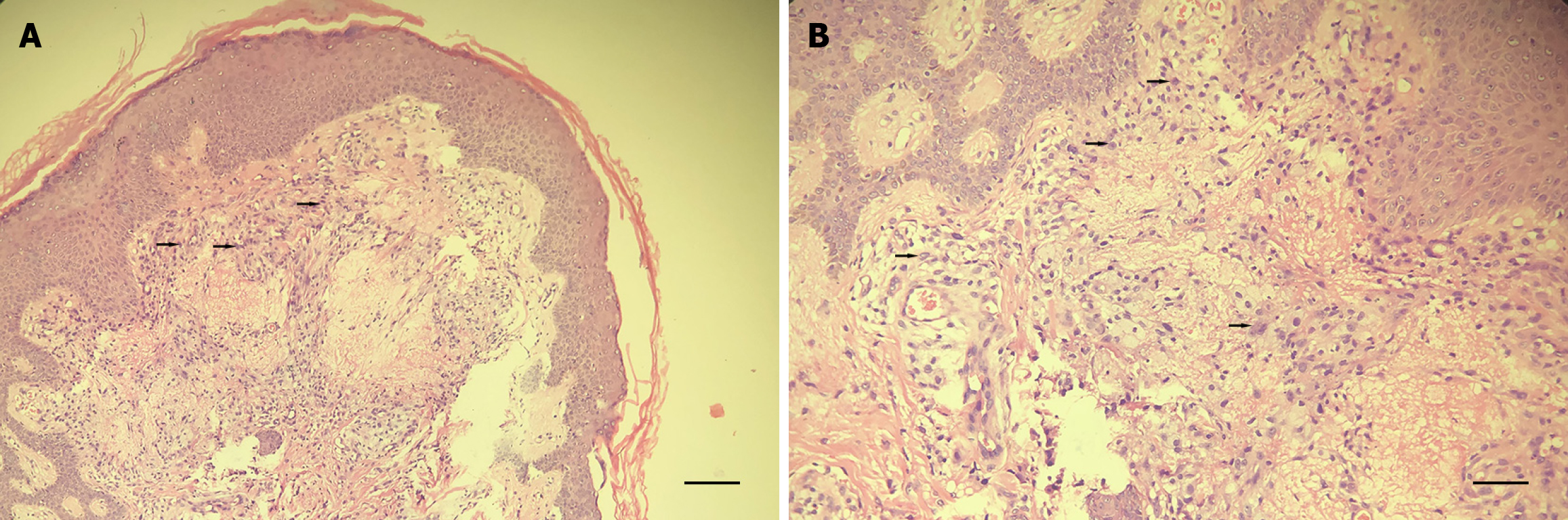
Laboratory examinations showed elevated levels of total cholesterol 11.58 mmol/L (reference range < 5.17 mmol/L), triglycerides 26.74 mmol/L (< 2.3 mmol/L), low-density lipoprotein cholesterol 4.61 mmol/L (< 3.36 mmol/L), alanine aminotransferase 47 U/L (5-40 U/L), gamma-glutamyl transferase 197 U/L (11-50 U/L) and glucose 12.35 mmol/L (3.89-6.1 mmol/L) (Table 1). Histopathological examination showed the epidermis appears mostly normal, while the dermis shows infiltration of foam cells and inflammatory cells that were consistent with an eruptive xanthomas (Figure 2).
| Test | Result | Reference |
| Total cholesterol | 11.58 mmol/L | < 5.17 mmol/L |
| Triglycerides | 26.74 mmol/L | < 2.3 mmol/L |
| Low-density lipoprotein cholesterol | 4.61 mmol/L | < 3.36 mmol/L |
| Alanine aminotransferase | 47 U/L | 5-40 U/L |
| Gamma-glutamyl transferase | 197 U/L | 11-50 U/L |
| Glucose | 12.35 mmol/L | 3.89-6.1 mmol/L |
| Height | 165 cm | |
| Weight | 87 kg | |
| BMI | 32.0 kg/m2 | 18.5-24 kg/m2 |
No special notes.
Eruptive xanthomas.
Lifestyle modifications are advised for EX patients, including a low-sugar, low-fat diet, appropriate exercise, weight control, and medication primarily focused on managing the underlying condition to restore blood lipid and blood sugar levels to normal.
The lesions resolved without any recurrence at 1-month follow-up.
The Liangshan Yi Autonomous Prefecture is situated in the southern part of Sichuan, China, and it boasts the highest population of the Yi ethnic group in the nation[1]. The patient was a male of Yi ethnicity. He was advised to follow a low-fat, low-sugar diet, exercise regularly, maintain a healthy weight. Due to elevated blood sugar and lipid levels, further consultation with an endocrinologist was recommended, but the patient refused medication, the lesions resolved without any recurrence at 1-month follow-up.
The occurrence of xanthoma is often caused by elevated blood lipids, which are deposited locally in tissues and engulfed by tissue cells, resulting in yellow or orange nodules, plaques, or patches as the main clinical manifestations of this skin disease. Based on the morphology of the rash, the site of onset, and the number and size of the skin lesions, it can be classified into seven types: Xanthelasma, nodular xanthomas, tendon xanthomas, flat xanthomas, eruptive xanthomas, palmar xanthomas, and disseminated xanthoma disease. Eruptive xanthomas (EX) are characterized by the sudden appearance of multiple reddish-yellow papules with a diameter of less than 5 mm on the buttocks and extensor surfaces of the limbs. During the acute phase, the base of the skin lesions may have erythema, and a Kobner's Phenomenon may also be observed. The rash can resolve spontaneously or leave behind pigmented scars several weeks later. The occurrence of EX is usually associated with severe hypertriglyceridemia (mostly Fredrickson type I and type V hyperlipoproteinemia), latent diabetes, obesity, or excessive alcohol consumption[2]. EX can also occur secondary to renal insufficiency, hypothyroidism, pancreatitis, gammopathy, cholestatic liver disease, and as a side effect of medications such as isotretinoin, acitretin, glucocorticoids, and estrogens[3].
The patient in this case is overweight, with a diet that is typically high in oily and greasy foods. The course of the illness is short, with a rapid onset of skin rash. Blood lipid and blood sugar levels are significantly elevated. Combining the presentation of skin lesions and pathological biopsy, a diagnosis of EX can be confirmed. The patient declined medication treatment and was advised to follow a low-sugar, low-fat diet, exercise regularly, and control their weight. After approximately one month, most of the skin lesions had subsided. The diagnosis of EX is not difficult, with the key being to determine the presence of any associated underlying damage. When suspecting this condition, a detailed inquiry should be made regarding dietary preferences, smoking and alcohol habits, as well as blood lipid and biochemical tests. If necessary, a pathological biopsy should be performed to confirm the diagnosis. In clinical practice, this condition needs to be differentiated from the following diseases: (1) Nodular xanthoma, which predominantly affects the joints of the limbs in an extended position. It presents as yellowish nodules of varying sizes, with a firm texture that can merge into plaques. It may be accompanied by atherosclerosis and abnormalities in cholesterol and triglyceride levels; (2) Xanthoma disseminatum, which primarily affects infants and young children. It manifests as single or multiple yellow-brown papules or nodules, with a tendency for self-resolution and generally not affecting overall health; (3) Disseminated xanthoma, characterized by yellow or brown papules and nodules. It commonly affects the flexural areas of the body, such as the groin and elbow creases, and may involve ocular or mucosal lesions. Blood lipid levels are normal, but 40% of patients also experience diabetes insipidus; (4) Plane xanthoma, presenting as dome-shaped papules and nodules with a waxy appearance. They often have a central umbilication and can be scattered or clustered, typically without fusion. Squeezing the top may release a cheeselike substance; and (5) Generalized eruptive histiocytoma, featuring 3-10 mm reddish-brown papules that occur in batches. They are scattered in a symmetrical distribution on the trunk and proximal limbs, tend to self-resolve, but can recur intermittently, lasting from months to years.
For patients with EX, lipid profile, blood sugar, biochemical markers, immunoglobulin levels, and thyroid function tests should be conducted to rule out systemic diseases such as liver, kidney, and thyroid disorders. The progression of EX can increase the risk of metabolic disorders, cardiovascular diseases, and malignant lymphomas. Literature reports have shown a significantly increased incidence of complications such as acute pancreatitis when triglyceride levels exceed 20 mmol/L. In this case, the patient has not yet experienced abdominal pain or other discomfort, but the possibility of complications should still be considered. Lifestyle modifications are advised for EX patients, including a low-sugar, low-fat diet, appropriate exercise, weight control, and medication primarily focused on managing the underlying condition to restore blood lipid and blood sugar levels to normal.
Currently, statins are the primary treatment for hyperlipidemia. In cases of severe or complex disease, hyperlipidemia can be managed by combining statins with other lipid-regulating agents like niacin, bile acid sequestrants, fibrates, and ezetimibe[4]. In general, skin lesions will naturally fade after a few weeks, but laser treatment or surgical excision may be necessary for more stubborn lesions.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Dermatology
Country/Territory of origin: China
Peer-review report’s classification
Scientific Quality: Grade D
Novelty: Grade B
Creativity or Innovation: Grade C
Scientific Significance: Grade C
P-Reviewer: Sunil V, India S-Editor: Liu JH L-Editor: A P-Editor: Zhao S
| 1. | Dezhi C, Meili L, Yingjian H, Yiping H, Yu T, Weibo L. Population genetics of 27 Y-STRs for the Yi population from Liangshan Yi Autonomous Prefecture, China. Int J Legal Med. 2021;135:441-442. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 2. | Kim SM, Lee H, Kim YC. Eruptive Xanthoma With Dermal Mucin Deposition. Am J Dermatopathol. 2021;43:583-584. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 3. | Ladizinski B, Lee KC. Eruptive xanthomas in a patient with severe hypertriglyceridemia and type 2 diabetes. CMAJ. 2013;185:1600. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 9] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 4. | Karr S. Epidemiology and management of hyperlipidemia. Am J Manag Care. 2017;23:S139-S148. [PubMed] |