Published online Jun 6, 2024. doi: 10.12998/wjcc.v12.i16.2813
Revised: February 9, 2024
Accepted: April 8, 2024
Published online: June 6, 2024
Processing time: 207 Days and 11.2 Hours
As research on diabetes continues to advance, more complex classifications of this disease have emerged, revealing the existence of special types of diabetes, and many of these patients are prone to misdiagnosis and underdiagnosis, leading to treatment delays and increased health care costs. The purpose of this study was to identify four causes of secondary diabetes.
Secondary diabetes can be caused by various factors, some of which are often overlooked. These factors include genetic defects, autoimmune disorders, and diabetes induced by tumours. This paper describes four types of secondary diabetes caused by Williams–Beuren syndrome, Prader–Willi syndrome, pituitary adenoma, and IgG4-related diseases. These cases deviate significantly from the typical progression of the disease due to their low incidence and rarity, often leading to their neglect in clinical practice. In comparison to regular diabetes patients, the four individuals described here exhibited distinct characteristics. Standard hypoglycaemic treatments failed to effectively control the disease. Subsequently, a series of examinations and follow-up history confirmed the diagnosis and underlying cause of diabetes. Upon addressing the primary condition, such as excising a pituitary adenoma, providing glucocorticoid supplementation, and implementing symptomatic treatments, all patients experienced a considerable decrease in blood glucose levels, which were subsequently main
Rare diseases causing secondary diabetes are often not considered in the diag
Core Tip: The etiology of secondary diabetes is complex, and it is often misdiagnosed as common type 2 diabetes in clinic, especially diabetes caused by some rare diseases, including Williams-Beuren syndrome, Prader-Willi syndrome, Pituitary adenoma, and IgG4-related diseases. It is difficult to confirm before some special tests, such as genetic testing, these posing a challenge for physicians. The aim of this report is to summarize the diagnosis and treatment of these four secondary diabetes patients, and to provide perspective and reference to other relevant cases.
- Citation: Song WR, Xu XH, Li J, Yu J, Li YX. Secondary diabetes due to different etiologies: Four case reports. World J Clin Cases 2024; 12(16): 2813-2821
- URL: https://www.wjgnet.com/2307-8960/full/v12/i16/2813.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i16.2813
Diabetes is a global disease that affects people worldwide, and severe complications contribute significantly to mortality rates. As diagnostic tests have advanced, secondary diabetes caused by genetic defects or antibody abnormalities has become more recognized. Some common types of secondary diabetes include pancreatic inflammatory diabetes, steroid-related diabetes, and endocrine dysfunction. This paper focuses on four different diseases that can lead to diabetes: Williams-Beuren syndrome (WBS) Prader–Willi syndrome (PWS), pituitary adenoma, and IgG4-related diseases. Since it is difficult to diagnose secondary diabetes caused by these diseases, inexperienced clinicians often overlook or misdiagnose these diseases, resulting in difficulties in disease management, poor prognosis, and high mortality rates.
Case 1: A 51-year-old female was admitted to the hospital due to elevated blood glucose for more than a year as well as dry mouth, polydipsia, and oedema for more than three months.
Case 2: A 53-year-old male patient was admitted to the hospital with intermittent yellow skin staining for 5 years, dry mouth, polydipsia, and polyuria for 3 years.
Case 3: A 13-year-old male patient was admitted for “dry mouth, polydipsia, or polyuria for 10 d”.
Case 4: A 30-year-old female was hospitalized due to intermittent dry mouth, polydipsia, polyuria for 10 years, and frequent urination for 3 d.
Case 1: One year prior, the patient had elevated blood glucose but no obvious symptoms, such as dry mouth or polydipsia. She was diagnosed with hyperglycaemia and started regular metformin treatment, which indicated type 2 diabetes mellitus. In addition to dry mouth, polydipsia, and oedema of the face and lower limbs, the patient also experienced fatigue, numbness in the hands, occipital pain, limited visual field, and other symptoms. However, she did not experience dizziness, poor appetite, nausea or vomiting, but a weight loss of approximately 10 kg was observed, as was a significant fluctuation in her blood glucose levels.
Case 2: Five years prior, the patient developed yellow skin staining of the sclera, face, and abdomen, accompanied by multiple swollen glands and yellow urine. Magnetic resonance (MR) resonance imaging of the upper abdomen revealed dilatation of the bile ducts, stenosis of the lower common bile duct, gallbladder enlargement and cholestasis. Pancreatic cancer was considered, and surgery was recommended. Three years prior, the patient developed dry mouth, polydipsia, polyuria, weight loss, and other symptoms without obvious inducement and was diagnosed with diabetes after his fasting blood glucose test reached 20 mmol/L (3.9-6.0 mmol/L) and the HbA1c level reached 16.6%. One week prior, the patient was hospitalized again with yellow skin staining on the sclera, face, abdomen, and urine.
Case 3: Ten days prior, he developed dry mouth, polydipsia, polyuria, weight loss and other symptoms without an obvious cause. In the prior week, the patient self-measured fasting blood glucose level fluctuated between 8.3 mmol/L and 11.0 mmol/L, and his blood glucose level remained high even after diet control, leading to a diagnosis of diabetes.
Case 4: The patient had a 10-year history of diabetes, 3 d prior, she was admitted to our department due to her atypical symptoms at her age and her distinctive facial features, which led us to suspect a special type of diabetes.
Case 1: The patient had a history of hypertension for six years and was taking four different antihypertensive drugs. However, her blood pressure was not controlled, with her systolic pressure fluctuating between 160 mmHg and 170 mmHg and her diastolic pressure fluctuating between 95 mmHg and 110 mmHg.
Case 2: Seven years prior, the patient was found to have a small mass in the upper margin of the right eye after rhinitis. The mass gradually increased in size but became slightly smaller after anti-inflammatory drug administration; the size of the mass increased again, however, after the patient stayed up late and became cold, with a size of 2 cm × 0.5 cm. There was a slight sense of pressure in the right eye, accompanied by a foreign body sensation, photophobia, tearing, itching, and discomfort in the left eye.
Case 3: The patient had poor sucking ability, hypotonia, and other symptoms in infancy before 2 years of age, accompanied by lethargy, reduced movement, and crying. After the age of two, he began to have an increased appetite and gained weight by the age of three. He achieved the ability to sit at 9 months and walk independently at 2 years. He did not start speaking until he was 4 years old, and between the ages of 5 and 8, he experienced several hospitalizations for hyperthermia, pneumonia, bronchitis, and tonsillitis due to low immunity. Three years previously, the patient was diagnosed with PWS.
Case 4: She was born prematurely in the seventh month of gestation with a birth weight of 1500 g. She experienced growth retardation, spoke in single words at 2 years of age, and walked against the wall at the same age. She also had a history of mental retardation, inability to count and distinguish colours, unique personality, pixie-faced appearance. She had been diagnosed with hypertension for eight years and had been taking hypertensive tablets for several years. One year prior, she developed cerebral infarction and was treated in the hospital for dizziness, nausea, and vomiting.
Case 1: The patient’s sister had similar facial features.
Case 2: The patient denied any relevant family history.
Case 3: The patient is the only child in his family, and his mother denied any relevant family history.
Case 4: The patient has a healthy brother, and her mother suggested her great-aunt had the same facial features.
Case 1: During the physical examination, the patient had clear consciousness, acromegaly, slight eyelid oedema, slight pitted oedema of the lower limbs, and finger clubbing.
Case 2: During the physical examination, he developed yellow skin staining of the sclera, face, and abdomen, with dry mouth and weight loss.
Case 3: Physical examination revealed a height of 140 cm, weight of 56 kg, and body mass index (BMI) of 28.57 kg/m2, indicating central obesity. The patient also exhibits special features, such as a long face, narrow forehead, almond-shaped eyes, small mouth, hands and feet, full back of hands, conical fingers, and disappearance of the ulnar edge curve. Scratches were visible on his limbs. There was no breast development or vulvar pigmentation, and he had sparse pubic hair in the scrotum and no armpit hair.
Case 4: Physical examination revealed a short stature (height 148 cm, weight 56 kg), and a BMI of 26.5 kg/m2, along with mental retardation, unique personality and pixie-faced appearance.
Case 1: Laboratory tests revealed normal thyroid function and sex hormone levels. However, the insulin-like growth factor-1 level was elevated at 229.00 ng/mL (normal range: 48-209 ng/mL), and the growth hormone (GH) level was elevated at 50.00 ng/mL (normal range: 0.126-9.88 ng/mL). The ratio of urinary microalbumin/creatinine (H-ALB/UCREA) indicated diabetic nephropathy, with a value of 569.905 mg/g (normal range: under 30 mg/g). The insulin/C-peptide ratio suggested insufficient insulin secretion and a delayed peak. Her renin-aldosterone and cortisol levels were within normal limits.
Case 2: Immunohistochemistry revealed that the ratio of IgG4/IgG was 40%, and CD38, Mum-1, and scattered Ki-67 positivity was detected. The patient serum IgG4 concentration was 19.40 g/L (0.03-2.01 g/L). Liver function tests indicated a total bilirubin (TBIL) level of 62.4 mol/L (2-20.4 mol/L), direct bilirubin (DBIL) of 45.8 mol/L (0-10 mol/L), alanine aminotransferase (ALT) of 101 U/L (5-40 U/L), aspartate aminotransferase of 43 U/L (8-40 U/L), gamma-glutamyl transpeptidase (GGT) of 225 U/L (6-50 U/L), blood amylase (AMY) of 124 U/L (25-104 U/L), and serum lipase of 254 U/L (40-150 U/L). The patient insulin/C-peptide ratio suggested a delayed peak in insulin secretion. The urinary microalbumin/creatinine ratio was 60.030 mg/g. One week prior, the liver function results were as follows: TBIL 25.5 mol/L, DBIL 19.0 mol/L, ALT 70 U/L, and GGT 523 U/L. The autoimmune antibody levels were IgG4 5.450 g/L and IgE 726.20 IU/mL, indicating the recurrence of IgG4-related disease.
Case 3: Auxiliary examination conducted 3 years ago revealed a gene deletion in chromosome 15q11-13. Hormonal tests revealed elevated testosterone levels, decreased 25-hydroxyvitamin D levels, and normal cortisol levels. Blood glucose and HbA1c levels were slightly elevated, and thyroid function was normal. One week prior, HbA1c level was 10.90%, and the ratio of urinary microalbumin/creatinine indicated diabetic nephropathy. Insulin/C peptide levels suggested insulin resistance, diabetes autoantibodies were negative, and liver and kidney function, thyroid function, electrolytes, lipids, amylase, lipase, myocardial enzyme spectrum were all normal.
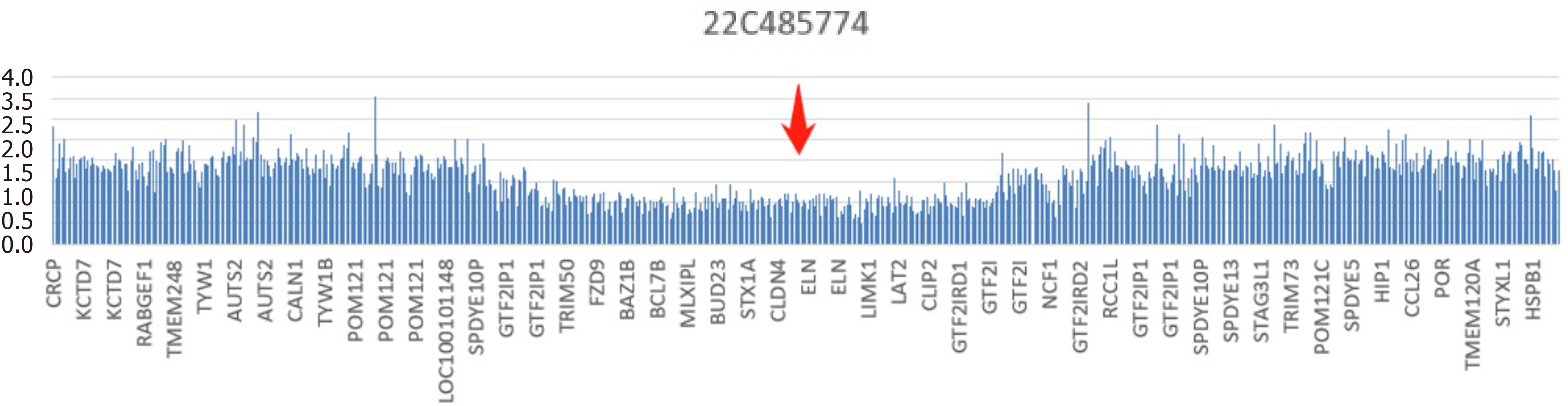
Case 4: Urinary microalbumin/creatinine (H-ALB/UCREA) was 770.639 mg/g, indicating diabetic nephropathy. Her HbA1c level was 10.00%, and routine urine test results showed protein positivity. Her sex hormone levels were normal, her serum parathyroid hormone level was 90.50 pg/mL (6-80 pg/mL), and no abnormalities were found in the aldosterone/renin system. The insulin/C peptide level suggested insufficient insulin secretion with a delayed peak. No obvious abnormalities were found in the thyroid, uterus, adnexa, heart, carotid artery, or abdominal ultrasound. An electrocardiogram showed sinus rhythm with a low T-wave. Whole-exome gene detection revealed a copy number deletion of approximately 1.49 Mb in the long arm of chromosome 7, 7q11.23 (Figure 1). The mutation locus chr7:g.72717544+AF8-74203079del was preliminarily determined to be pathogenic. This region contains a haplodose-sensitive ELN gene and 26 coding genes.
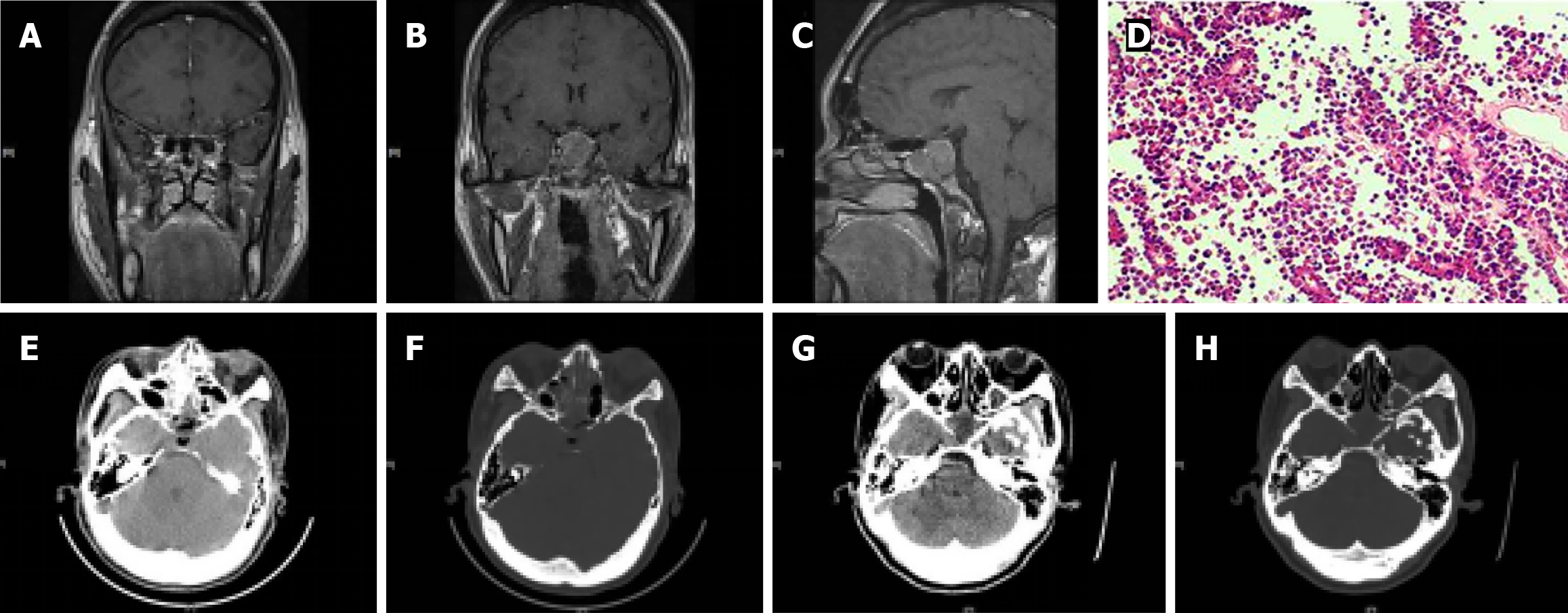
Case 1: Imaging tests revealed a thyroid nodule in the right thyroid. Carotid ultrasound revealed left carotid atherosclerotic plaque formation and thickening of the bilateral common carotid artery intima-media complex. Heart ultrasound revealed widening of the ascending aorta, enlargement of the left atrium, increased ventricular septum thickness, reduced diastolic function of the left ventricle, and pericardial effusion. Head and chest computed tomography (CT) scans showed no abnormalities, while abdominal ultrasound revealed multiple stones in both kidneys. Dynamic MR of the pituitary gland showed bilateral inferior turbinate hypertrophy (Figure 2A), and coronal (Figure 2B) and sagittal (Figure 2C) images revealed neoplastic lesions in the pituitary region, with the tumour invading the bilateral sphenoid sinuses and partially wrapping around the bilateral internal carotid artery.
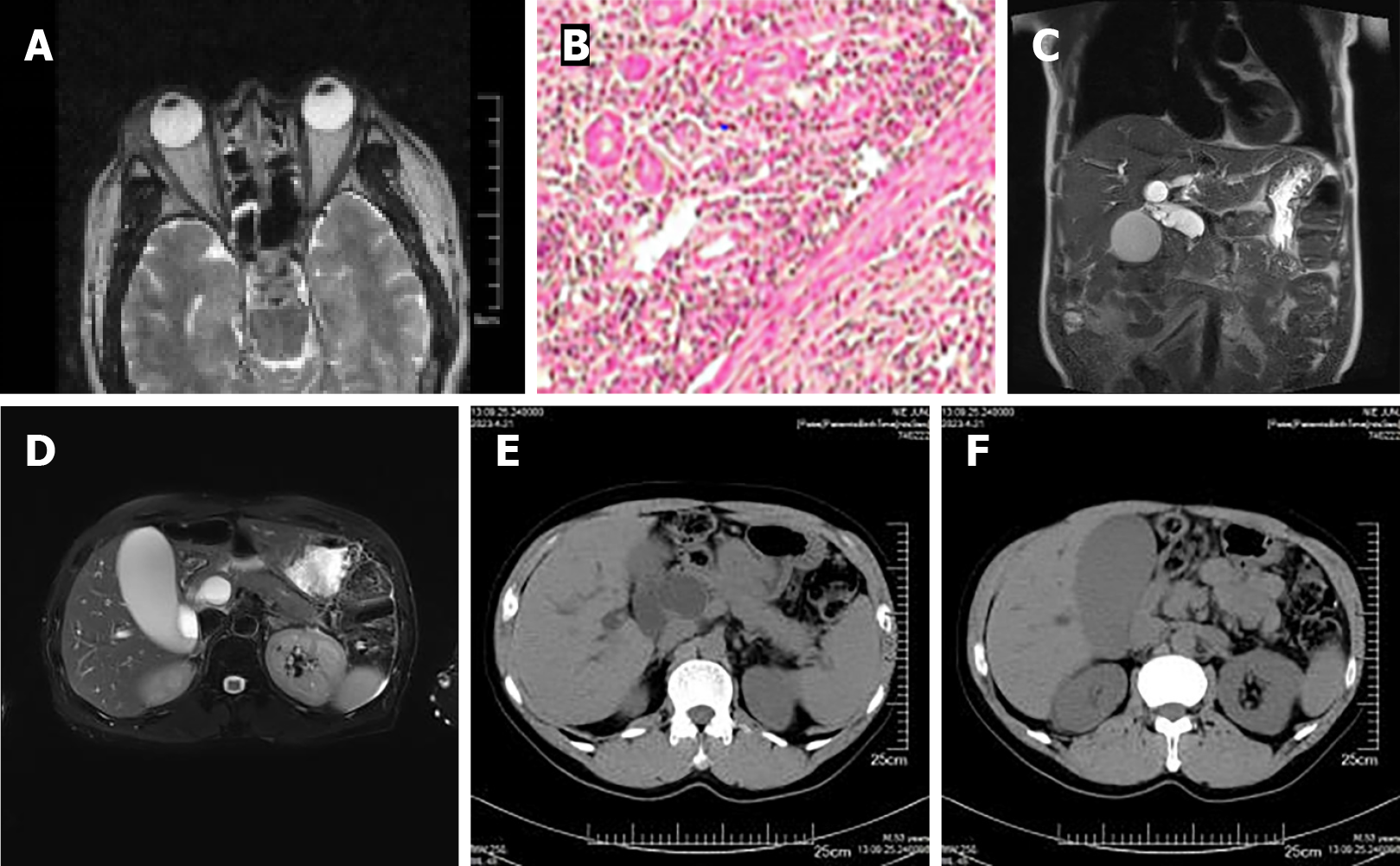
Case 2: An MR scan of the orbit showed infectious nodules in the outer upper margin of the eyeballs on both sides as well as an occupying lesion in the right lacrimal gland space (Figure 3A). Pathological examination of the right orbital mass indicated an inflammatory pseudotumour in the lacrimal gland (Figure 3B). Ultrasonography of the submandibular gland indicated multiple substantive lesions in the bilateral submandibular glands, and pathology of the lymph node in the right mandible showed chronic submandibular adenitis. Head and chest CT showed no significant substantive lesions. Epigastric MR indicated dilatation of the common bile duct (Figure 3C), a decreased pancreatic T1WI signal, and an enlarged pancreatic head, coupled with enlargement of the gallbladder and cholestasis (Figure 3D). High-resolution chest CT showed micronodules in the lower lobes of both lungs. Epigastric ultrasonography revealed no space-occupying pancreatic lesions. One week prior, a CT scan of the entire abdomen showed obvious dilatation of the bile ducts (Figure 3E), enlargement of the gallbladder and cholestasis (Figure 3F).
Case 3: Ultrasound and CT revealed mild to moderate fatty liver, mild mitral regurgitation, and an enlarged cardiac shadow.
Case 4: CT tomography revealed a low-density lesion in the right frontal lobe, indicating fatty liver and kidney stones. Gastroscopy revealed chronic superficial gastritis with bile reflux. Cranial magnetic resonance imaging (MRI) showed a cerebral infarction in the right frontal parietal lobe. Diffusion-weighted imaging of the head indicated acute infarction in the right frontal parietal lobe and centre of the semicovale. Cranial MR angiography suggested multiple stenoses in the left middle cerebral artery.
The patient was diagnosed with a pituitary GH tumour that caused secondary diabetes.
The patient was diagnosed as IgG4-related disease that caused secondary diabetes.
The patient was diagnosed as PWS that caused secondary diabetes.
The patient was diagnosed as WBS that caused secondary diabetes.
The pituitary tumour was successfully removed using a transsphenoidal approach via a neuroendoscope, and pathology confirmed the presence of a pituitary adenoma (Figure 2D). After surgery, the patient’s GH concentration decreased to 4.270 ng/mL. A postoperative pituitary CT scan showed enlargement of the sellar region, with no residual tumour tissue observed, and visible filling of the liquid signal was observed (Figure 2E and F). On the 9th postoperative day, a small amount of gas was observed in the soft tissue window of the pituitary CT (Figure 2G), and the bone window (Figure 2H) revealed further enlargement of the sellar region. Unexpectedly, the patient’s blood pressure was well controlled with a low dose of hypertensive drugs. Additionally, 50 mg of acarbose tablets helped stabilize her glucose levels. Overall, both hypertension and diabetes in this patient were considered secondary to the pituitary adenoma.
After long-term oral prednisone, calcium tablets, and liver-protecting tablets, the patient’s symptoms improved significantly. He was administered mealtime insulin combined with basal insulin as a hypoglycaemic program and prednisone 10 mg daily, and his condition remained stable. After relapse, 40 mg prednisone was administered daily, insulin aspart and basal insulin were used for hypoglycaemia, and the patient’s condition is currently stable.
PWS is a rare disease for which there is no specific treatment. Symptomatic and supportive treatment is generally recommended. We advised the patient’s mother to control his diet, encourage increased exercise, and provide necessary psychological counselling to prevent weight gain, delay diabetes complications, and improve prognosis. The patient was administered a hypoglycaemic program with premixed insulin (aspartame 30) and metformin, and his glucose levels were well controlled with a decreasing insulin dose.
WBS is a genetic defect disease, and currently, there is no specific treatment for this disease. However, various interventions can be used to improve quality of life and reduce symptoms. For example, psychotherapy can help regulate emotions and improve social and learning abilities; physical therapy can improve muscle tension and balance abilities; drug therapy, such as anti-anxiety, depression, and attention-deficit medications, can also improve symptoms; and family care is crucial for patient recovery and quality of life, and targeted training can help them maximize their ability to live independently. Ultimately, she was administered insulin 30R with acarbose for hypoglycaemia, and her blood glucose level and overall condition remained stable, with a certain degree of self-care ability.
The patient’s condition improved significantly after the operation, and she remained stable during the 2-year follow-up.
The patient’s condition improved significantly after standardized treatment, and he remained stable during the 2-year follow-up.
The patient remained stable during the 2-year follow-up.
The patient remained stable during the 2-year follow-up.
The incidence of type 2 diabetes is increasing, with 638 million people projected to be living with the disease by 2021. This number is expected to increase to 693 million by 2045[1]. Treatment for diabetes primarily involves lifestyle interventions such as adjusting one’s diet, engaging in regular exercise, and maintaining a healthy weight[2]. Drug therapy options include oral hypoglycaemic agents, insulin injections, and GLP-1 receptor agonists[3]. Surgery has also become a significant consideration in recent years. Various factors can contribute to secondary diabetes, with pancreatic diseases such as pancreatitis and pancreatic resection being the most common causes[4]. Other factors include the long-term use of corticosteroids, immunosuppressants, and diuretics. Endocrine diseases such as pituitary tumours and hypothyroidism can also lead to secondary diabetes. Additionally, genetic conditions such as familial hypercholesterolemia and polycystic ovary syndrome have been reported as causes. T1DM and T2DM account for approximately 90% of diabetes cases, while atypical forms may make up approximately 10% of cases[5]. Rare causes include gene defects and autoimmune diseases.
With the development of genetic testing technologies, numerous genetic and hereditary diseases have been identified. In this paper, two patients presented with genetic diseases. When patients exhibit typical signs and changes in appearance, genetic testing should be considered to screen for possible variant genes and establish a foundation for disease diagnosis. When disease progression does not align with age, the underlying cause should be investigated. In the case of the patient with WBS mentioned in this paper, the onset of hypertension and diabetes occurred during adolescence, and there was even a history of cerebral infarction. This metabolic syndrome was inconsistent with their age, necessitating an investigation into its cause. WBS was diagnosed through whole-exon gene detection. This disease is characterized by a copy number deletion of approximately 1.49 Mb in the long arm of chromosome 7, 7q11.23[6]. The mutation site in this patient, chr7:g.72717544_74203079del, was identified for the first time without a similar record in GenBank.
In addition, patients with PWS exhibit typical growth retardation in infancy, obesity, and low immunity in childhood. Therefore, it is crucial to conduct relevant examinations as early as possible to facilitate early detection and treatment. PWS is a rare inherited metabolic disease[7] characterized mainly by low intelligence, obesity, abnormal facial features, and eye problems. It is caused by the deletion of the q11-13 region of chromosome 15[8] and is inherited from the paternal line. Currently, there is no cure for this syndrome, but symptoms can be managed and treated through nutritional management, ophthalmic treatment, and rehabilitation[9]. In this case, the patient with PWS developed diabetes or even diabetic nephropathy 3 years after the genetic defect was identified, leading to a poor prognosis. Therefore, early recognition and diagnosis of the primary disease are crucial for improving patient prognosis and outcomes.
Special types of disease should be considered when a patient’s clinical manifestations do not match the expected progression of the disease. The IgG4-related diseases described in this paper are autoimmune diseases[10]. They are characterized by plasma cell infiltration of IgG4 and can affect various organs, including the pancreas, bile ducts, thyroid, lymph nodes, and lungs[11]. In this case, the patient had a short history of diabetes but rapidly developed diabetic nephropathy and had difficulty controlling blood glucose levels. This progression is inconsistent with the typical development of type 2 diabetes and suggests that other factors may be involved. IgG4-associated diseases are known to cause tissue swelling, fibrosis, and infiltration of lymphocytes and plasma cells[12]. Furthermore, the patient had a history of a lacrimal gland occupying the right eye, which was not detected until five years prior when obvious yellow staining symptoms appeared. This ultimately led to the diagnosis of IgG4-associated disease. The diagnosis of these diseases relies on histopathological and immunohistochemical tests, such as evaluating the number of IgG4-positive cells and the IgG4/IgG ratio. Currently, there is no specific treatment for IgG4-associated diseases. However, immunosuppressants such as glucocorticoids are often used as first-line treatments[13]. Importantly, long-term use of oral prednisone tablets can lead to increased blood glucose levels. Therefore, controlling the primary disease is crucial, and blood glucose levels can be effectively managed only after the disease is stable.
Additionally, patients with acromegaly in this study exhibited noticeable facial changes and a restricted visual field, which is not consistent with diabetic retinopathy[14]. It is crucial to determine the cause and rule out cranial nerve compression and pituitary diseases. In this case, the patient was diagnosed with a GH pituitary tumour[15] through dynamic MRI of the pituitary region, and histological analysis of the tumour indicated an adenoma (Figure 2D). After surgery, the patient’s visual field was restored, and there was a significant improvement in blood glucose and blood pressure levels.
If certain clinical manifestations and signs do not align with the occurrence and progression of the disease, further examination is necessary to identify the possible cause. Only a definitive diagnosis, cause, and pathogenic mechanism can lead to improved treatment of the disease, resulting in improved therapeutic effects and improved prognosis and truly reflecting the principles of individualized treatment. After identifying the aetiology of the four types of secondary diabetes in this study, the disease was effectively controlled, and the follow-up results were satisfactory. This study provides valuable experience and a reference for clinicians in diagnosing and treating rare diseases.
Secondary diabetes is often overlooked. As the clinical signs and laboratory results of patients are nonspecific, it is necessary for the clinicians having sufficient experience to identify the primary disease. Thus, providing reliable interventions and treatments for the patients to improve their prognosis and quality of life and extend their life span.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s classification
Scientific Quality: Grade B, Grade C
Novelty: Grade B, Grade B
Creativity or Innovation: Grade B, Grade B
Scientific Significance: Grade B, Grade B
P-Reviewer: Kute VB, India; Tavan H, Iran S-Editor: Che XX L-Editor: A P-Editor: Zhao S
| 1. | Cho NH, Shaw JE, Karuranga S, Huang Y, da Rocha Fernandes JD, Ohlrogge AW, Malanda B. IDF Diabetes Atlas: Global estimates of diabetes prevalence for 2017 and projections for 2045. Diabetes Res Clin Pract. 2018;138:271-281. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3709] [Cited by in RCA: 4364] [Article Influence: 623.4] [Reference Citation Analysis (0)] |
| 2. | Tahrani AA, Bailey CJ, Del Prato S, Barnett AH. Management of type 2 diabetes: new and future developments in treatment. Lancet. 2011;378:182-197. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 419] [Cited by in RCA: 383] [Article Influence: 27.4] [Reference Citation Analysis (0)] |
| 3. | Scheen AJ. Dual GIP/GLP-1 receptor agonists: New advances for treating type-2 diabetes. Ann Endocrinol (Paris). 2023;84:316-321. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 21] [Reference Citation Analysis (0)] |
| 4. | Hart PA, Bellin MD, Andersen DK, Bradley D, Cruz-Monserrate Z, Forsmark CE, Goodarzi MO, Habtezion A, Korc M, Kudva YC, Pandol SJ, Yadav D, Chari ST; Consortium for the Study of Chronic Pancreatitis, Diabetes, and Pancreatic Cancer(CPDPC). Type 3c (pancreatogenic) diabetes mellitus secondary to chronic pancreatitis and pancreatic cancer. Lancet Gastroenterol Hepatol. 2016;1:226-237. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 220] [Cited by in RCA: 321] [Article Influence: 35.7] [Reference Citation Analysis (0)] |
| 5. | Steenkamp DW, Alexanian SM, Sternthal E. Approach to the patient with atypical diabetes. CMAJ. 2014;186:678-684. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 12] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 6. | Pober BR. Williams-Beuren syndrome. N Engl J Med. 2010;362:239-252. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 584] [Cited by in RCA: 568] [Article Influence: 37.9] [Reference Citation Analysis (0)] |
| 7. | Butler MG. Prader-Willi Syndrome and Chromosome 15q11.2 BP1-BP2 Region: A Review. Int J Mol Sci. 2023;24. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 24] [Reference Citation Analysis (0)] |
| 8. | Butler MG, Hartin SN, Hossain WA, Manzardo AM, Kimonis V, Dykens E, Gold JA, Kim SJ, Weisensel N, Tamura R, Miller JL, Driscoll DJ. Molecular genetic classification in Prader-Willi syndrome: a multisite cohort study. J Med Genet. 2019;56:149-153. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 112] [Article Influence: 16.0] [Reference Citation Analysis (0)] |
| 9. | Calcaterra V, Magenes VC, Destro F, Baldassarre P, Silvestro GS, Tricella C, Visioli A, Verduci E, Pelizzo G, Zuccotti G. Prader-Willi Syndrome and Weight Gain Control: From Prevention to Surgery-A Narrative Review. Children (Basel). 2023;10. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 10. | Bateman AC, Culver EL. Challenges and pitfalls in the diagnosis of IgG4-related disease. Semin Diagn Pathol. 2024;41:45-53. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 8] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 11. | Wallace ZS, Naden RP, Chari S, Choi H, Della-Torre E, Dicaire JF, Hart PA, Inoue D, Kawano M, Khosroshahi A, Kubota K, Lanzillotta M, Okazaki K, Perugino CA, Sharma A, Saeki T, Sekiguchi H, Schleinitz N, Stone JR, Takahashi N, Umehara H, Webster G, Zen Y, Stone JH; American College of Rheumatology/European League Against Rheumatism IgG4-Related Disease Classification Criteria Working Group. The 2019 American College of Rheumatology/European League Against Rheumatism Classification Criteria for IgG4-Related Disease. Arthritis Rheumatol. 2020;72:7-19. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 142] [Cited by in RCA: 354] [Article Influence: 59.0] [Reference Citation Analysis (0)] |
| 12. | Peyronel F, Fenaroli P, Maritati F, Schleinitz N, Vaglio A. IgG4-related disease: advances in pathophysiology and treatment. Expert Rev Clin Immunol. 2023;19:537-547. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 7] [Reference Citation Analysis (0)] |
| 13. | Khosroshahi A, Wallace ZS, Crowe JL, Akamizu T, Azumi A, Carruthers MN, Chari ST, Della-Torre E, Frulloni L, Goto H, Hart PA, Kamisawa T, Kawa S, Kawano M, Kim MH, Kodama Y, Kubota K, Lerch MM, Löhr M, Masaki Y, Matsui S, Mimori T, Nakamura S, Nakazawa T, Ohara H, Okazaki K, Ryu JH, Saeki T, Schleinitz N, Shimatsu A, Shimosegawa T, Takahashi H, Takahira M, Tanaka A, Topazian M, Umehara H, Webster GJ, Witzig TE, Yamamoto M, Zhang W, Chiba T, Stone JH; Second International Symposium on IgG4-Related Disease. International Consensus Guidance Statement on the Management and Treatment of IgG4-Related Disease. Arthritis Rheumatol. 2015;67:1688-1699. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 573] [Cited by in RCA: 672] [Article Influence: 67.2] [Reference Citation Analysis (0)] |
| 14. | Lin KY, Hsih WH, Lin YB, Wen CY, Chang TJ. Update in the epidemiology, risk factors, screening, and treatment of diabetic retinopathy. J Diabetes Investig. 2021;12:1322-1325. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 181] [Cited by in RCA: 214] [Article Influence: 53.5] [Reference Citation Analysis (0)] |
| 15. | Fleseriu M, Langlois F, Lim DST, Varlamov EV, Melmed S. Acromegaly: pathogenesis, diagnosis, and management. Lancet Diabetes Endocrinol. 2022;10:804-826. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 118] [Article Influence: 39.3] [Reference Citation Analysis (0)] |