Published online Jun 6, 2024. doi: 10.12998/wjcc.v12.i16.2796
Revised: February 12, 2024
Accepted: April 11, 2024
Published online: June 6, 2024
Processing time: 128 Days and 1.9 Hours
As one of the most common aesthetic surgical procedures carried out today, ble
To present an overview of the surgical techniques considered for upper lid blepharoplasty and fat pad management, in addition to information on how a surgeon may approach the best treatment for his patient based on current publications in literature.
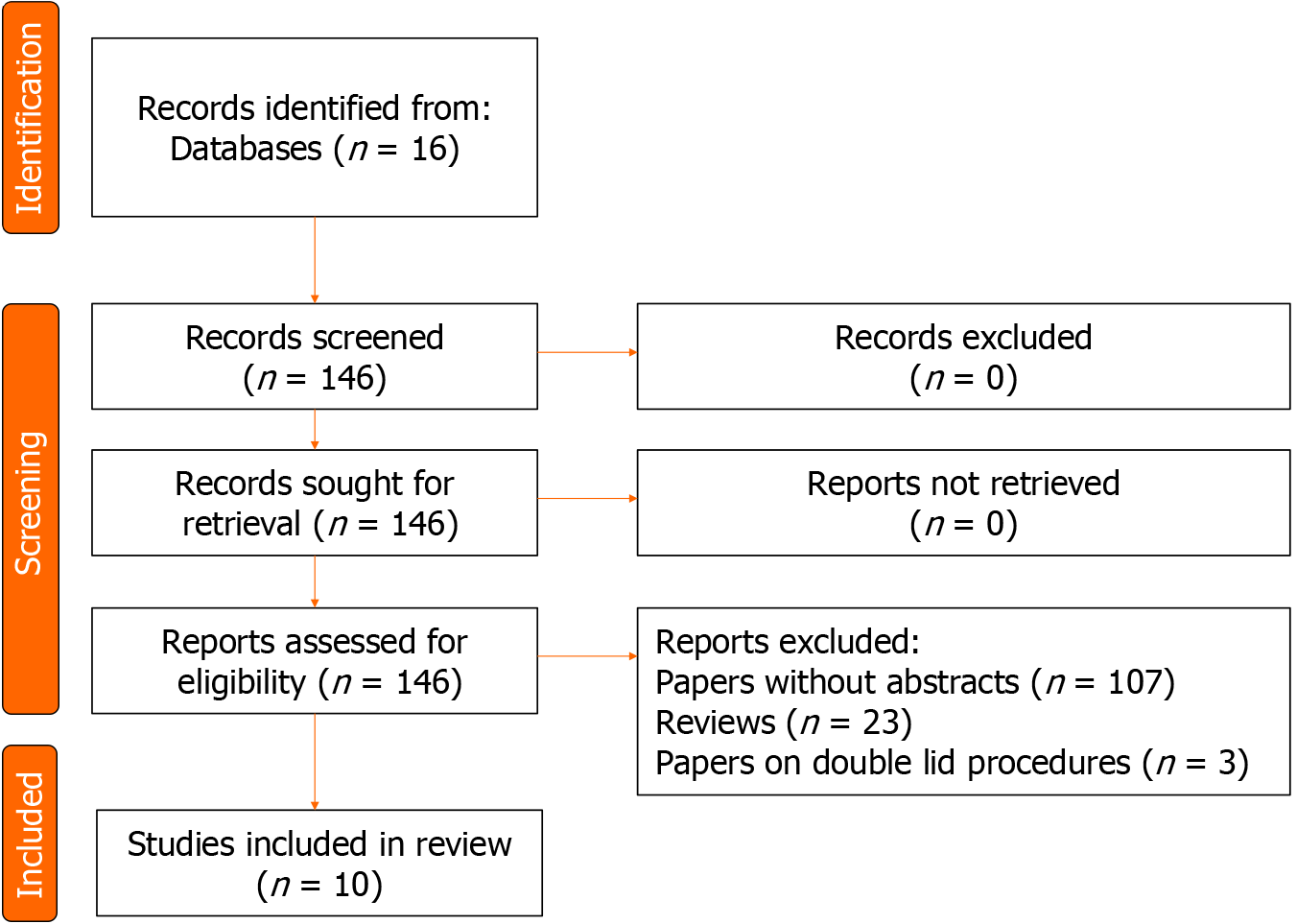
We searched the literature published between 2013, to 2023 using Medline and Reference Citation Analysis. The database was searched using the keywords “upper blepharoplasty” AND “fat”. Papers without full text/abstracts and reviews were excluded. The search strategy followed the PRISMA. The American Society of Plastic Surgeons guidelines for Therapeutic Studies checklist was used to assess all articles. Two authors individually reviewed each article and rated them for importance and relevance to the topic. A consensus was sought and the most relevant studies.
After the application of the selection criteria used in our review, 13 publications were found to address upper lid blepharoplasty specifically. Three of these studies were reviews and three were retrospective studies. Five publications were comparative studies and a further two were clinical trials.
The tendency of modern surgery is to be conservative, by removing adipose tissue only if strictly necessary and restoring the volume of the upper eyelid in a concept of beauty that espouses a "full" sight. There is no gold standard technique to achieve younger and enhanced eyelids. Long-term prospective comparative studies are fundamental in understanding which path is the best to follow.
Core Tip: Blepharoplasty is common cosmetic and aesthetic surgical procedure carried out by plastic surgeons. There are numerous option and techniques to address the individual needs of each patient. It is of clinical importance to diagnose underlying conditions, manage and treat individuals seeking this type of surgery. Patient outcomes, prevention of complications and success of therapy depend on selecting the most suitable option and applying the correct surgical technique to address the needs of each patient.
- Citation: Miotti G, Di Filippo J, Grando M, Salati C, Parodi PC, Spadea L, Gagliano C, Musa M, Zeppieri M. Fat management in upper blepharoplasty: Addition or subtraction blepharoplasties, how and when. World J Clin Cases 2024; 12(16): 2796-2802
- URL: https://www.wjgnet.com/2307-8960/full/v12/i16/2796.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i16.2796
Blepharoplasty is a surgical procedure to repair conditions affecting the eyelids. Indications for blepharoplasty include improving the cosmetic appearance of the lids and also to correct senile changes in these structures[1]. All lid tissues can be treated and corrected with blepharoplasty, and in particular the excess epidermal tissue, saggy lids, ptosis and pseudo-ptosis, ocular septa and unwanted orbital fat[2].
The advent of advanced clinical aesthetic procedures in the field of plastic surgery to make people look younger is the prime driver for blepharoplasty[3]. The quest for facial plastic surgery has greatly ticked up among both genders in the last decade with blepharoplasty ranking among the top 10 requested procedures. While surgical techniques have largely been the mainstay of managing defects in the lids, newer non-surgical methods now also exist to correct such condition and are gaining wider acceptability[4].
The upper and lower eyelids consist of anterior, middle, and posterior lamellae[5]. The most superficial layer of the upper eyelid contains skin and orbicularis muscle; the latter plays a key role in lid closure and blinking reflex and may be divided into a pretarsal, preseptal, and orbital portion according to the structures it overlays. Going deeper we may find the orbital septum extending from the orbital rim’s periosteum to the upper edge of the superior tarsus establishing a boundary for the orbital contents. Underneath the orbital septum lie the two fat compartments of the upper eyelid: The nasal and central (or pre-aponeurotic) fat pads[6]. The deepest layer is formed by the levator palpebrae superioris muscle and aponeurosis followed by the superior tarsal muscle (or Müller’s muscle), both of which insert on the upper tarsal plate and are responsible for lid elevation. The reversal of the conjunctiva covers the deepest side of the eyelid. Orbital fat cells are less metabolically active compared to normal body fat.
Their cell structures are also smaller when compared to cells of normal body fat. Within the eyelid, the medial fat tissue is the most vascularized and has smaller lobules compared to other fat tissue in the lids. The medial fat is also more vascularized and is separated from the central fat compartment by the trochlea of the superior oblique muscle[7,8].
The search for a younger and more captivating look goes hand in hand with the surgeons' desire to find the best technique to achieve this goal. For this reason, several authors have asked themselves whether the path followed for many years was still the ideal one to achieve an aesthetic concept of a "young eye". We can see how in recent years, the concept of subtraction blepharoplasty, understood as a treatment aimed at removing adipose tissue as well as excess skin, has become old[3]. The current trend, also favored by aesthetic medicine treatments, is to seek a "full" look, obtained through an augmentation blepharoplasty[8]. What influences surgical treatment, according to the surgeons' thinking, is the possibility of determining a long-lasting result, something that non-surgical treatments are only partially able to do. In this minireview we have considered publications from the last 10 years, evaluating what has emerged in the literature on the surgical treatment of the upper eyelid.
We searched the literature published between 2013, to 2023 using Medline (https://pubmed.ncbi.nlm.nih.gov) and Reference Citation Analysis (https://www.referencecitationanalysis.com). The database was searched using the key
The American Society of Plastic Surgeons guideline for Therapeutic Studies checklist was used to assess all articles[9]. Two authors (Miotti G and Zeppieri M), individually reviewed each article and rated them for importance and relevance to the topic. A consensus was sought and the most relevant studies[8-18] are shown in Table 1.
| Ref. | Year | Type of study | Race | Conclusions |
| Tonnard et al[8] | 2013 | Retrospective study with 500 patients | All | Fat grafting and careful trimming of unwanted skin tissue were generally used in these patients. The results were the preservation of eyelid volume and also the correction of sunken eyelids by fat grafting |
| Zoumalan and Roostaeian[10] | 2016 | Review | All | The authors concluded that the standard procedure for upper eyelid surgery is the excision of skin, muscle, and fat from the eyelids. They also recommended a browlift if needed |
| Zhou et al[11] | 2014 | Clinical trial | Asians | Authors observed that a stable supratarsal fold can be achieved by excising the pretarsal orbicularis oculi muscle. This procedure coupled with stripping of submuscular soft tissue and orbital fat resulted in a tough cicatricial connection from the levator aponeurosis to the skin |
| Alghoul et al[12] | 2020 | Comparative study | All | An opinion of upper eyelid appearance in the younger population was advanced. Characteristics suggested include smooth eyelid folds which are higher laterally with a symmetric pretarsal space. Eyelid volume should be subtle and flatter medially and fuller laterally |
| Figueiredo et al[13] | 2017 | Randomized controlled trial | All | Although not in a statistically significant way, the brassiere sutures introduced by Goldberg can help to obtain an upper eyelid with harmonious proportions and a fullness of the eyebrow-eyelid transition |
| Pacella et al[14] | 2010 | Review | All | A review of the transconjunctival technique for upper eyelid blepharoplasty is primarily effective in patients with minimal skin excess. Also, they advised that this procedure only gives access to nasal fat pad |
| Massry[15] | 2011 | Retrospective study with 76 patients | All | Surgery times can be prolonged by adjusting the position of the nasal fat pads. This critical step preserves upper lid fat, supplementing appearance after surgery |
| Lee et al[16] | 2015 | Comparative study | Asians | The authors posited that advancing the upper lid pre-aponeurotic fat can mitigate unwanted lid folds, thus resulting in better cosmesis |
| Collar et al[17] | 2013 | Review | All | When there is significant hollowing and no excess skin, the patient should undergo only augmentation procedures. One of such procedure for volume restoration of the upper eyelid is fat grafting |
| Park et al[18] | 2011 | Retrospective study with 50 patients | Asians | Authors suggested that the roof fat graft can be manipulated during blepharoplasty to produce better results |
As at the time of this review, 13 publications were found to address upper lid belpharoplasty specifically. Three of these studies were reviews and three were retrospective studies. Five publications were comparative studies and a further two were clinical trials.
Upper eyelid blepharoplasty is a surgical procedure aimed at rejuvenating the appearance of the upper eyelids by removing excess skin, fat, and muscle. This procedure is commonly sought after to address droopy or sagging eyelids, which can create a tired or aged look. During the surgery, incisions are carefully made along the natural creases of the eyelids to minimize scarring. The surgeon then removes or repositions the tissue, resulting in a more youthful and refreshed appearance. Upper eyelid blepharoplasty not only enhances the aesthetic appeal of the eyes but can also improve vision by eliminating obstruction caused by excess skin. It is a popular cosmetic procedure known for its ability to restore a more alert and youthful appearance to the eyes, ultimately boosting self-confidence and overall facial harmony.
There are relatively few manuscripts on techniques used for upper eyelid blepharoplasty. In between fat grafting, skin trimming and orbicularis muscle resection, different authors have reported success in addressing this surgical procedure[8-18].
Aging is typically associated with decreased dermal thickness, subcutaneous volume loss and reduced skin elasticity. In the upper eyelid these changes translate into greater skin laxity and droopiness of the eyelid skin, called dermatochalasis (especially in the lateral portion), subcutaneous brow fat volume loss, atrophy or herniation of the fat compartments and eventually blepharoptosis[3,7].
Complications with upper lid blepharoplasty are typically minimal, especially with volume preservation techniques which reduce the risk of upper lid hollowing. Luckily, the periorbital region shows great healing abilities and post-operative scars are usually well hidden and minimal. The surgeon should take into consideration the patient’s premorbid condition as the goal of the surgical procedure, especially for those patients needing to correct some age-related change.
As has emerged in the literature of the last two decades[3,19,20], the periocular region must be considered a single whole from the point of view of the dynamics of aging. If in the past the various areas of this region were treated individually, nowadays surgeons must consider treating multiple regions if necessary to restore a more youthful and attractive sight. For recent years, excision of skin, muscle, and fat from the eyelids together with a brow lift has been the standard pattern for blepharoplasty[10].
If brow ptosis or brow fat volume loss is contributing to an increase in dermatochalasis, the surgeon should consider combining upper blepharoplasty with brow-lift to achieve better results and avoid worsening the brow ptosis. Brow-lift may be achieved through many different techniques depending on the extent of the ptosis. Direct brow-lifts, first described by Castanares[21], are usually reserved for severe cases of ptosis and when the incisions are placed within existing fold, scars usually heal well. Lateral ptosis of the brow can cause important hooding in the lateral portion of the upper eyelid.
Upper lid skin can be easily excised to effectively remove the excess. The Orbicularis muscle can be opened or excised. It is important to preserve the pretarsal portion as it is important for the process of blinking. Excision of the orbicularis muscle, when redundant, can reduce the volume of the upper lid causing the outermost layer to adhere to the orbital septum thereby helping to create the supraorbital fold. On the other hand, muscle preservation maintains the fullness of the eyelid and reduces the risk of a hollowed appearance. The surgical procedure for upper blepharoplasty differs in the Asian race. The typical Asian eyelids are characterized by the complete lack of, or smaller supraorbital folds, laxity of pretarsal skins, increased fat volume, and a prominent epicanthal fold. The mechanism of creating a supraorbital fold consists of reconstructing the complex interconnection between the levator aponeurosis and dermis. The technique proposed by Zhou et al[11] involves a full incision into the pretarsal orbicularis oculi muscle and the submuscular portion to remove unwanted orbital fat. The result is a cicatricized adhesion between the levator aponeurosis and the skin which creates a vivid and stable supraorbital fold.
There is a close relationship between the pretarsal space and the eyelid fold which has been studied in great depth to determine where the most harmonious aspect of the upper eyelid is[12,22,23]. The upper eyelid in younger individuals has a smooth fold which increases in height going lateral, with a well-formed and symmetric pretarsal region. An attractive upper eyelid has “full” appearance with classic volume distribution that is subtle and flatter medially and fuller laterally. This behavior of the upper eyelid adipose tissue has been described in depth for example by Le Louarn et al[24]. With aging, fat content in the upper lid can increase or decrease, leading to bulging eyelid or a sunken look[12]. This concept of maintaining a "full" gaze was also similarly evaluated by Figueiredo et al[13]. In their work, they report how the brassiere sutures introduced by Goldberg and Lew[25] can help to obtain an upper eyelid with harmonious pro
Documented upper blepharoplasty evidence emerged in the early 2000s, when Tonnard et al[8] published his “aug
The traditional approach to treating herniated fat pads consisted of the removal of the entire fat pad. Although this may give an immediate improvement in the eyelid’s appearance, long-term results would give the impression of a skeletonized look with superior sulcus depression. The initial change in surgical procedure consisted simply of a more judicious removal of periorbital fat, specifically the most prominent herniations of nasal fat pads. The treatment of the fat compartments of the upper eyelid is fascinating as their behavior varies from patient to patient and achieving a balance is not as simple as one might think. In fact, many mechanisms hide behind a "trivial" fat bag. A particular approach to the upper eyelid fat compartments was described by Pacella et al[14] in which they advocated a transconjunctival approach to upper blepharoplasty. Their technique is however only useful to patients with fewer nasal and is tied to the ability to obtain the nasal fat pad.
The use of surgical procedures that increase the volumes of the upper eyelid can be reserved both to complete the classic blepharoplasty as already mentioned, but also represent a valid tool for correcting congenital or acquired defects. In fact, when there is significant hollowing and no excess skin, the patient should undergo only augmentation procedures. One such procedure for volume restoration of the upper eyelid is fat grafting[17]. Lipofilling is the most used surgical technique. Indeed, fat is autologous and after an initial resorption, it gives a relatively stable result. All precautions must be taken to avoid inhomogeneous fat resorption and cyst formation. Because of the thinness of the upper eyelid layers, it is suggested that surgeons position the fat graft in a suborbicularis plane. When a proper technique is used in both eyelids, complications are very rare.
Tonnard et al[8] systematically proposed the use of fat grafting to restore a more youthful appearance to the upper skin. He described how the amount of grafting must reproduce a slight undercorrection rather than an overcorrection. Correcting an excess of adipose tissue (by liposuction or resection) is more complex and less tolerated by patients than a second session. The same concept was also expressed by Burkat[26]. He concurred that the removal of the adipose tissue of the upper eyelid should possibly be limited to the nasal portion only to prevent the appearance of a sunken superior sulcus. In some cases, when different age-related defects are at play, a mixed approach may be undertaken by combining blepharoplasty with fat grafting as described by Park et al[18]. Both fat pads are dissected and moved inferiorly in between levator aponeurosis and orbicularis muscle.
An alternative to fat grafting may be the use of hyaluronic acid filler as reported by several authors[4,27] This type of treatment may be best reserved for patients affected by less severe hollowing and those open to repeated treatments. Degenerative changes to the upper eyelid may combine with different severities differing from patient to patient, so a thorough assessment is crucial for a personalized correction[28]. However, the generally accepted procedure in upper eyelid blepharoplasty is now aimed at preservation, repositioning, or filling of the upper lid fat. If the surgeon decides to reduce the bulk of fat in the upper eyelid, a conservative approach should be taken.
A better understanding that volume loss is one of the key components of facial and periorbital aging has led to a change of standards in lower eyelid rejuvenation techniques, with upper eyelid treatments lagging. Lately, also with regards to the upper eyelid, these authors have been transitioning from a subtractive type of surgery to similar more conservative, or restorative ones seen in lower eyelid surgery.
An excellent example is the technique described by Massry in 2011[15], as it shows how a simple modification to the upper lid blepharoplasty can help prevent postoperative hollowing. Massry redirected the prominent nasal fat pad (more resistant to resorption) towards the central upper eyelid compartment instead of removing it. It should however be noted that the nasal fat pad must be adequately freed to avoid unwanted tension.
Previously, Shorr et al[29] and Sozer et al[30], showed us how by transposing part of the central fat pad of the upper eyelid a greater fullness could be achieved, thus giving the periorbital region a more juvenile appearance. However, since the central fat pad is subject to most age-related atrophy this approach may risk deepening the central sulcus. The use of the pre-aponeurotic fat pad was subsequently considered in reconstructive surgery by Lee et al[16]. In this case, he proposed the advancement of the pre-aponeurotic fat in the treatment of upper eyelid retraction to prevent unintended multiple lid creases and provide satisfactory cosmetic outcomes.
Two aspects emerge from this brief review of related literature. The first aspect is the tendency of today's surgery to be conservative, removing adipose tissue only if strictly necessary and restoring the volume of the upper eyelid in a concept of beauty that espouses a "full" sight. The second aspect, however, is the proliferation of aesthetic medicine articles in literature, highlighting how these procedures are challenging surgery in becoming the first technique for upper eyelid rejuvenation. For the time being there is no well-defined common line of thought to achieve the goal of a younger and more fascinating sight, but long-term results will be fundamental in understanding which path is the best to follow.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: Italy
Peer-review report’s classification
Scientific Quality: Grade C
Novelty: Grade B
Creativity or Innovation: Grade B
Scientific Significance: Grade B
P-Reviewer: Oley MH, Indonesia S-Editor: Liu H L-Editor: A P-Editor: Zhao S
| 1. | Patel BC, Malhotra R. Upper Eyelid Blepharoplasty. 2023 Jul 24. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. [PubMed] |
| 2. | Rebowe RE, Runyan C. Blepharoplasty. 2023 Jul 24. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. [PubMed] |
| 3. | De Biasio F, Miotti G, Zingaretti N, Castriotta L, Parodi PC. Study on the Aging Dynamics of the Periorbital Region: From Observation to Knowledge of Physiopathology. Ophthalmic Plast Reconstr Surg. 2019;35:333-341. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 17] [Article Influence: 2.8] [Reference Citation Analysis (1)] |
| 4. | Miotti G, Zeppieri M, Pederzani G, Salati C, Parodi PC. Modern blepharoplasty: From bench to bedside. World J Clin Cases. 2023;11:1719-1729. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 6] [Reference Citation Analysis (2)] |
| 5. | Sand JP, Zhu BZ, Desai SC. Surgical Anatomy of the Eyelids. Facial Plast Surg Clin North Am. 2016;24:89-95. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 29] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 6. | Kakizaki H, Malhotra R, Selva D. Upper eyelid anatomy: an update. Ann Plast Surg. 2009;63:336-343. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 75] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 7. | Lambros V. Observations on periorbital and midface aging. Plast Reconstr Surg. 2007;120:1367-1376. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 270] [Cited by in RCA: 264] [Article Influence: 14.7] [Reference Citation Analysis (0)] |
| 8. | Tonnard PL, Verpaele AM, Zeltzer AA. Augmentation blepharoplasty: a review of 500 consecutive patients. Aesthet Surg J. 2013;33:341-352. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 53] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 9. | DePalma JA. Evidence-based clinical practice guidelines. Semin Perioper Nurs. 2000;9:115-120. [PubMed] |
| 10. | Zoumalan CI, Roostaeian J. Simplifying Blepharoplasty. Plast Reconstr Surg. 2016;137:196e-213e. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 44] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 11. | Zhou JH, Xu HF, Wu LH, Chen SS, Fan XL. Three mini-incision double-eyelid blepharoplasty. Ann Plast Surg. 2014;72:141-144. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 17] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 12. | Alghoul MS, Bricker JT, Venkatesh V, Gupta AR, Vaca EE, Sinno S, Ellis MF, Mustoe TA. Rethinking Upper Blepharoplasty: The Impact of Pretarsal Show. Plast Reconstr Surg. 2020;146:1239-1247. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 13. | Figueiredo MN, Tao J, Akaishi P, Limongi RM. Tarsal platform show after upper eyelid blepharoplasty with or without brassiere sutures. Arq Bras Oftalmol. 2017;80:345-349. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 14. | Pacella SJ, Nahai FR, Nahai F. Transconjunctival blepharoplasty for upper and lower eyelids. Plast Reconstr Surg. 2010;125:384-392. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 32] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 15. | Massry GG. Nasal fat preservation in upper eyelid blepharoplasty. Ophthalmic Plast Reconstr Surg. 2011;27:352-355. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 40] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 16. | Lee JH, Kim YD, Woo KI, Johnson ON 3rd. Preaponeurotic fat advancement in levator recession for treatment of upper eyelid retraction. Plast Reconstr Surg. 2015;135:680e-690e. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 17. | Collar RM, Boahene KD, Byrne PJ. Adjunctive fat grafting to the upper lid and brow. Clin Plast Surg. 2013;40:191-199. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 10] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 18. | Park S, Kim B, Shin Y. Correction of superior sulcus deformity with orbital fat anatomic repositioning and fat graft applied to retro-orbicularis oculi fat for Asian eyelids. Aesthetic Plast Surg. 2011;35:162-170. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 61] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 19. | Bruneau S, Foletti JM, Muller S, Vercasson C, Lauwers F, Guyot L. Does the Eyebrow Sag with Aging? An Anthopometric Study of 95 Caucasians from 20 to 79 Years of Age. Plast Reconstr Surg. 2016;137:305e-312e. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 20. | Camirand A, Doucet J, Harris J. Eyelid aging: the historical evolution of its management. Aesthetic Plast Surg. 2005;29:65-73. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 22] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 21. | Castañares S. Forehead wrinkles, glabellar frown and ptosis of the eyebrows. Plast Reconstr Surg. 1964;34:406-13. [RCA] [DOI] [Full Text] [Cited by in Crossref: 78] [Cited by in RCA: 77] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 22. | Fezza JP. The sigmoid upper eyelid blepharoplasty: redefining beauty. Ophthalmic Plast Reconstr Surg. 2012;28:446-451. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 14] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 23. | Vaca EE, Bricker JT, Helenowski I, Park ED, Alghoul MS. Identifying Aesthetically Appealing Upper Eyelid Topographic Proportions. Aesthet Surg J. 2019;39:824-834. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 30] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 24. | Le Louarn C, Buthiau D, Buis J. Structural aging: the facial recurve concept. Aesthetic Plast Surg. 2007;31:213-218. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 63] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 25. | Goldberg RA, Lew H. Cosmetic outcome of posterior approach ptosis surgery (an American Ophthalmological Society thesis). Trans Am Ophthalmol Soc. 2011;109:157-167. [PubMed] |
| 26. | Burkat CN. Fat preservation and other tips for upper lid blepharoplasty. Pearls Pitfalls Cosmet Oculoplast Surg. 2008;. [DOI] [Full Text] |
| 27. | Lambros V. Volumizing the brow with hyaluronic acid fillers. Aesthet Surg J. 2009;29:174-179. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 41] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 28. | Fagien S. Advanced rejuvenative upper blepharoplasty: enhancing aesthetics of the upper periorbita. Plast Reconstr Surg. 2002;110:278-91; discussion 292. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 90] [Cited by in RCA: 76] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 29. | Shorr N, Hoenig JA, Goldberg RA, Perry JD, Shorr JK. Fat preservation to rejuvenate the lower eyelid. Arch Facial Plast Surg. 1999;1:38-39. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 30. | Sozer SO, Agullo FJ, Palladino H, Payne PE, Banerji S. Pedicled fat flap to increase lateral fullness in upper blepharoplasty. Aesthet Surg J. 2010;30:161-165. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 24] [Article Influence: 1.6] [Reference Citation Analysis (0)] |