Published online Jun 6, 2024. doi: 10.12998/wjcc.v12.i16.2758
Revised: April 11, 2024
Accepted: April 19, 2024
Published online: June 6, 2024
Processing time: 99 Days and 6.5 Hours
Anesthetic drugs used in labor analgesia also paralyze the bladder muscle by blocking the sacral plexus, thereby affecting maternal postpartum spontaneous urination and increasing the risk of postpartum urinary retention (PUR).
To analyze the effect of percutaneous electrical stimulation at the Baliao point combined with biofeedback therapy for PUR prevention.
We selected 182 pregnant women who received labor analgesia in obstetrics bet
The first spontaneous urination time after delivery was more delayed (2.92 ± 1.04 h vs 3.61 ± 1.13 h, P < 0.001), with fewer initial postpartum urine (163.54 ± 24.67 mL vs 143.72 ± 23.95 mL, P < 0.001), more residual bladder urine (54.81 ± 10.78 mL vs 65.25 ± 13.52 mL, P < 0.001), more postpartum bleeding (323.15 ± 46.95 mL vs 348.12 ± 45.03 mL, P = 0.001), and longer waiting time for urination (0.94 ± 0.31 min vs 1.29 ± 0.42 min, P < 0.001), in the control group than in the combined therapy group. The control group also had higher PUR incidence (4.65% vs 15.85%, P = 0.016). Both groups had no adverse reactions, but the clinical total efficacy rate of the intervention was significantly higher in the combined therapy group than in the control group (95.35% vs 84.15%, P = 0.016).
Percutaneous electrical stimulation of the Baliao point combined with biofeedback can significantly promote postpartum micturition of parturients with labor analgesia, thereby effectively preventing PUR occurrence.
Core Tip: Epidural anesthesia is mainly used for labor analgesia. However, the pain block of anesthetics on the sacral plexus greatly reduces the sensitivity of sphincter function and bladder detrusor function, easily causing dysuria or increase of bladder residual urine volume and promoting postpartum urinary retention (PUR) occurrence. Our research focuses on the effect of percutaneous electrical stimulation of the Baliao point combined with biofeedback therapy in promoting postpartum micturition among parturients with labor analgesia. This intervention is better than biofeedback therapy alone for parturients with labor analgesia because it is more effective in preventing PUR.
- Citation: Wang XQ, Guan LS. Effect of percutaneous electrical stimulation at the Baliao point on preventing postpartum urinary retention after labor analgesia. World J Clin Cases 2024; 12(16): 2758-2764
- URL: https://www.wjgnet.com/2307-8960/full/v12/i16/2758.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i16.2758
Childbirth is a natural physiological process experienced by most women. However, severe pain during childbirth often makes this event unbearable for mothers. In recent years, with the continuous development and improvement of anesthesia technology, labor analgesia technology has been widely used in obstetrics because it effectively reduces maternal physical and mental pain, providing humane care. Labor analgesia technology mainly uses epidural anesthesia. However, anesthetics block the sacral plexus, reducing the sensitivity of sphincter function and bladder detrusor fun
Researchers are suggested to take advantage of the characteristics of traditional Chinese medicine after finding the cause of the disease, and then treat the patients according to syndrome differentiation. According to the principles of traditional Chinese medicine, PUR belongs to uroschesis and mostly results from bladder injury and adverse air movement. Therefore, stimulating the Baliao point associated with pelvic autonomic plexus in biofeedback therapy may be beneficial. Stimulating the Baliao points aids in dredging water and qi and regulating qi and blood. Hence, this study aimed to evaluate the efficacy of transcutaneous electrical stimulation of the Baliao points combined with biofeedback therapy in preventing PUR in parturients receiving labor analgesia. Its effect was observed and compared with that of simple biofeedback therapy to provide reference for the clinical prevention of PUR in this population.
This study included pregnant women who underwent labor analgesia in the Department of Obstetrics at Suzhou Ninth People's Hospital Affiliated to Soochow University (Suzhou Ninth People's Hospital) between June 2022 and December 2023. The inclusion criteria were as follows: (1) Age ≥ 18 years, with indications for labor analgesia through epidural block anesthesia; (2) singleton pregnancy with cephalic presentation; (3) gestational age ≥ 37 wk; and (4) voluntary participation with a signed relevant informed consent form. Conversely, the exclusion criteria were the following: (1) Estimated fetal weight of > 4000 or < 2500 g before delivery; (2) concurrent urinary tract infection; (3) gestational diabetes mellitus; (4) coagulation dysfunction; (5) mental illness history; (6) PUR occurrence before delivery; (7) pelvic diseases; and (8) long-term metal instrument implantation.
The control group received biofeedback therapy using a biological stimulation feedback instrument (DS-A; Jiangsu Furui Technology Co., Ltd.) starting from the day the parturient completed the analgesic delivery. In a supine position, the parturient was advised to relax throughout their body while the vaginal electrode was slowly inserted into the vagina. Then, the current intensity was set to a low-frequency current. The maternal contraction movement was guided according to the image feedback of the instrument. Feedback and current stimulation were alternately performed within the maternal tolerance range. The intervention was performed once a day for 20 min each time for two consecutive days.
In the joint group, biofeedback therapy was combined with percutaneous electrical stimulation of the Baliao acupoint. Biofeedback therapy was the same as the control group. In percutaneous electrical stimulation of the Baliao acupoint, a computerized intermediate-frequency transcutaneous electrical stimulation therapy device (B2008-III; Beijing Benao Technology Co., Ltd.) was used. Healthcare providers performing the intervention should first learn the new version of “meridian and acupoint science”[6] to locate the Baliao points. Before treatment, the potential locations of the electrodes were disinfected routinely. Then, an electrode piece was positioned on the acupoint of the Baliao point and correctly connected with the computerized intermediate-frequency percutaneous electrical stimulation therapeutic apparatus. After the machine was switched on, the therapeutic apparatus was turned into a working state. To achieve patient acceptance without discomfort, the operator adjusted the treatment voltage amplitude according to the maternal tolerance to electrical stimulation. This intervention was conducted once a day, lasting 25 min each time for two consecutive days.
General information included participants’ age, reproductive history, gestational age during delivery, first stage labor duration, second-stage labor duration, third-stage labor duration, and neonatal weight.
Clinical indicators comprised the following: (1) The time of first spontaneous urination after delivery, the first urine volume after delivery, the residual urine volume in the bladder, and the volume of postpartum hemorrhage; (2) the waiting time before urination after the intervention; (3) PUR incidence; and (4) adverse reactions during the intervention (skin burns, blistering, etc.). According to the Guidelines for Prepregnancy and Pregnancy Health Care (2018)[7], patients were diagnosed with PUR if they had dysuria occurring within 6 h to 2 days after delivery and needed urinary catheters or other methods to assist urination.
The clinical efficacy of the two interventions was evaluated according to the relevant standards stated in the above
Statistical data were analyzed using the SPSS 26.0 software. We employed t test for comparing measurement data, which are expressed as the mean ± SD, between the two groups. Count data, which are expressed as percentage (%), were compared by χ2 test between such groups. A P value < 0.05 was considered statistically significant.
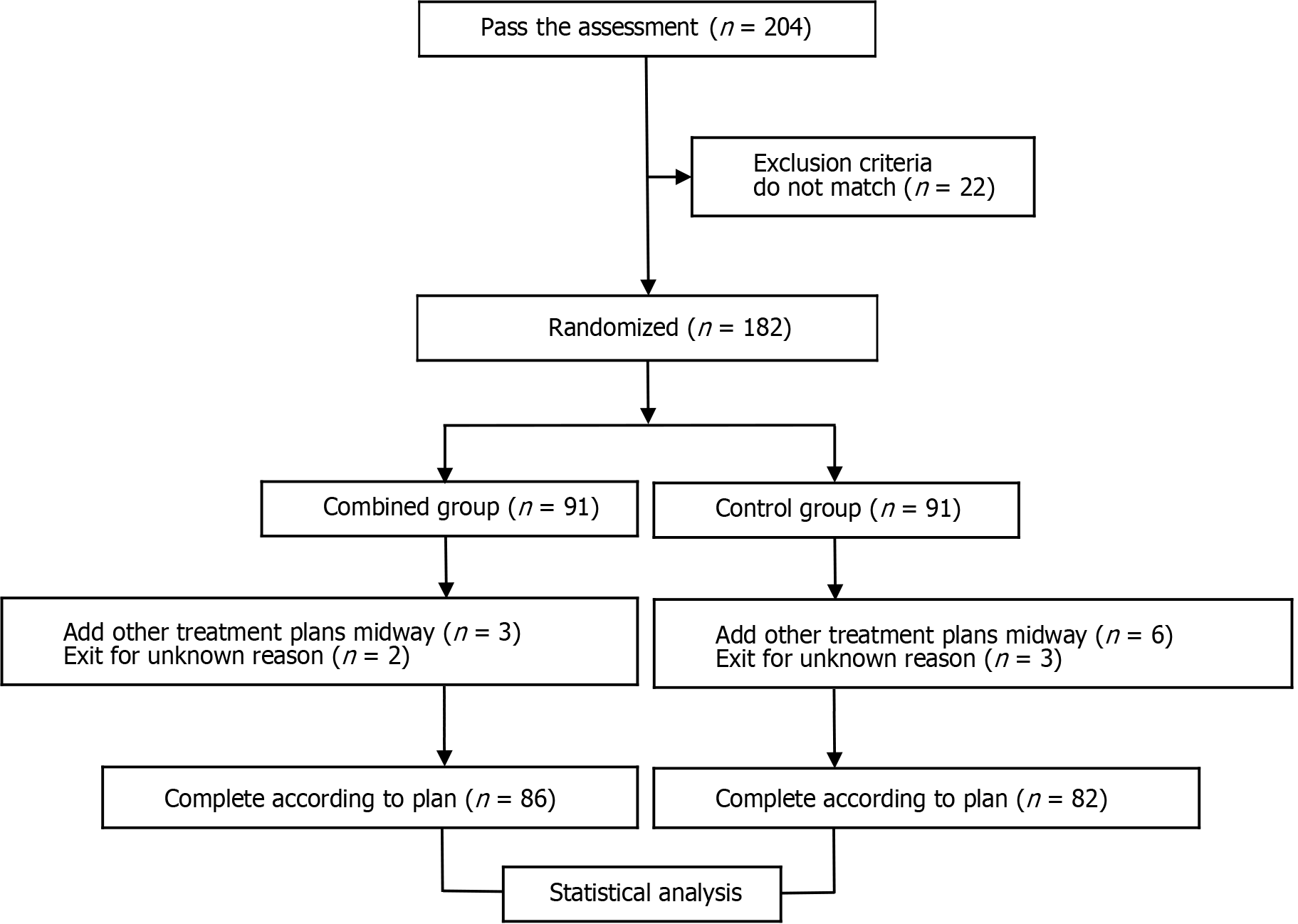
Figure 1 illustrates the research framework. Of the 204 enrolled parturients, 22 were excluded, leaving 182 participants for this study. These participants were randomly assigned to the combined therapy group (n = 91) and the control group (n = 91). During the intervention, nine participants had other treatment plans (three in the combined therapy group and six in the control group) and five withdrew for unknown reasons (two in the combined therapy group and three in the control group). As shown in Table 1, age, reproductive history, gestational age during delivery, total labor duration, first stage labor duration, second-stage labor duration, and neonatal weight did not significantly differ between the two groups (P > 0.05).
| General information | Combined therapy group (n = 86) | Control group (n = 82) | t/χ2 value | P value |
| Age (yr) | 29.43 ± 3.54 | 29.19 ± 3.81 | 0.423 | 0.673 |
| Reproductive history, n (%) | 0.151 | 0.697 | ||
| Primipara | 57 (66.28) | 52 (63.41) | ||
| Multipara | 29 (33.72) | 30 (36.59) | ||
| Gestational age at delivery (wk) | 38.98 ± 1.35 | 38.76 ± 1.28 | 1.083 | 0.280 |
| First stage labor duration (min) | 505.54 ± 163.08 | 508.67 ± 161.23 | 0.125 | 0.901 |
| Second-stage labor duration (min) | 83.75 ± 23.14 | 84.59 ± 22.76 | 0.237 | 0.813 |
| Third-stage labor duration (min) | 9.18 ± 3.23 | 9.34 ± 3.08 | 0.328 | 0.743 |
| Neonatal weight (kg) | 3.25 ± 0.87 | 3.29 ± 0.92 | 0.138 | 0.772 |
As shown in Table 2, the time of the first spontaneous urination and the waiting time for urination were significantly earlier and shorter in the combined therapy group than in the control group (P < 0.05). In addition, the combined therapy group had a significantly higher volume of the first postpartum urine (P < 0.05) and significantly lesser volumes of bladder residual urine and postpartum hemorrhage (P < 0.05) than the control group. Finally, PUR developed in four participants from the combined therapy group and thirteen from the control group (incidence rates: 4.65% and 15.85%, respectively). Thus, the incidence of PUR in the combined therapy group was significantly lower than that in the control group (χ2 = 5.792, P = 0.016). Meanwhile, both groups reported no adverse reactions.
| Clinical indicators | Combined therapy group (n = 86) | Control group (n = 82) | t/χ2 value | P value |
| Time of first spontaneous urination after delivery (h) | 2.92 ± 1.04 | 3.61 ± 1.13 | 4.121 | < 0.001 |
| First postpartum urine volume (mL) | 163.54 ± 24.67 | 143.72 ± 23.95 | 5.280 | < 0.001 |
| Bladder residual urine volume (mL) | 54.81 ± 10.78 | 65.25 ± 13.52 | 5.547 | < 0.001 |
| Postpartum hemorrhage volume (mL) | 323.15 ± 46.95 | 348.12 ± 45.03 | 3.515 | 0.001 |
| Waiting time for urination (min) | 0.94 ± 0.31 | 1.29 ± 0.42 | 6.165 | < 0.001 |
| PUR occurrence | 4 (4.65) | 13 (15.85) | 5.792 | 0.016 |
Table 3 shows that the total efficacy rate of the combined therapy group was 95.35%, which was significantly higher than that of the control group (84.15%) (P < 0.05).
| Group | Number | Remarkable result | In force | Null and void | Total efficacy rates |
| Combined therapy group | 86 | 59 (68.60) | 23 (26.75) | 4 (4.65) | 82 (95.35) |
| Control group | 82 | 34 (41.46) | 35 (42.69) | 13 (15.85) | 69 (84.15) |
| χ2 value | 5.792 | ||||
| P value | 0.016 |
The ideal method of childbirth analgesia should not only include the alleviation of labor pain but also encourage mothers to actively participate in the delivery process, reduce the impact of childbirth on the fetus, and improve the natural childbirth rate. Labor analgesia aims to reduce the pain threshold during delivery through various methods. During the first stage of labor, the puerpera should rest to gain enough physical strength to complete the delivery process. Epidural block is a commonly used analgesic method for vaginal delivery and has shown to have a good analgesic effect[8]. However, epidural block also blocks the sensitivity of the sacral nerve, directly affecting the function of the bladder detrusor muscle and consequently increasing the risk of postpartum voiding difficulty as well as PUR. PUR can affect uterine contractions and increase vaginal bleeding volume; it can even cause urinary system infections, which can lead to permanent urinary system damage; hence, PUR has a great impact on maternal health[9]. Therefore, effective measures must be explored to prevent postpartum PUR in parturients who received labor analgesia.
Biofeedback therapy is a commonly used pelvic floor rehabilitation therapy that helps improve postpartum pelvic floor muscle coordination disorder[10]. Its principle is to convert the biological signal that the patient cannot directly feel into a signal that the patient can directly perceive through the instrument; it helps patients feel bladder pressure change more accurately, corrects the wrong urination training, assists the improvement of pelvic floor muscle training, and improves and restores bladder function. Chen et al[11] found that pelvic floor electrical stimulation biofeedback therapy can promote postpartum bladder function sensitivity in parturients, thereby beneficial for preventing postpartum PUR. Therefore, pelvic floor biofeedback therapy combined with pelvic floor muscle electrical stimulation may promote passive contraction of the pelvic floor muscle, achieving the purpose of training patients’ detrusor muscle ability[12,13]. This combined therapy has a certain effect on preventing postpartum PUR. According to traditional Chinese medicine, PUR belongs to the category of “urinary incontinence.” The pathogenesis involves poor bladder gasification and obstructed water channels. The Baliao acupoint is located physiologically and anatomically in the 1st–4th posterior sacral foramen. A posterior branch of the 1st–4th sacral nerve runs inside the foramen; thus, acupuncture may be applied to stimulate sacral nerve conduction. Nerve impulses can be transmitted to the upper urinary center by dredging the meridians to promote the normal contraction and relaxation of bladder sphincter and detrusor[14]. Liu et al[15] emphasized that electrical stimulation of the Baliao acupoint can increase urination and improve bladder residual urine volume, similar to the results of the current study. Electrical stimulation therapy is a traditional acupuncture treatment scheme derived from traditional Chinese medicine. Its mechanism is similar to that of electroacupuncture. It combines percutaneous nerve stimulation therapy and meridian theory, changing mechanical stimulation to physical therapy with quantifiable current stimulation to trigger systemic reflex mechanism. The current study showed that the time of the first spontaneous urination and the waiting time for urination in the combined therapy group were significantly earlier and shorter than those in the control group. The combined therapy group also had significantly more postpartum urine at first instance and significantly lesser bladder residual urine than the control group. These results indicate that transcutaneous electroacupuncture at the Baliao points can effectively improve further the sphincter function and bladder detrusor function of postpartum women with labor analgesia; it can also promote the recovery of postpartum bladder function and urethral function, thereby reducing the detrusor contraction disorder and improving the complex symptoms of maximum bladder capacity reduction. Likewise, Zhu et al[16] inferred that electroacupuncture stimulation of the Baliao points improves the urinary flow rate, bladder urine volume, and residual urine volume.
If the postpartum maternal urine is excessive and cannot be excreted in time, the bladder will be distended, causing the blood sinus on the placental stripping surface to open, thereby increasing the volume of postpartum hemorrhage[17]. Stimulating the relevant acupoints has been reported to be beneficial in promoting early spontaneous urination and improving the first urine volume after delivery, the bladder residual urine volume, and the postpartum hemorrhage volume[18]. This previous finding is similar to our study results, i.e., stimulating the Baliao point can reduce the volume of postpartum hemorrhage in parturients with labor analgesia. This outcome may be explained by the ability of transcutaneous electrical stimulation of the Baliao point to improve bladder gasification function. This technology also helps speed up maternal self-urination and shorten the waiting time for urination; hence, the urine can be excreted in time, thereby preventing the increase of postpartum hemorrhage caused by bladder expansion. Moreover, transcutaneous electrical stimulation of the Baliao point can dredge postpartum local blood stasis and repair damaged meridians, also resulting in the reduction of postpartum hemorrhage.
Pregnant women with labor analgesia are prone to postpartum urination disorders, including postpartum PUR, which is not conducive to the recovery of a postpartum body[19,20]. Our study results revealed that the combined therapy group had a significantly higher total clinical efficacy rate and significantly lower postpartum PUR incidence than the control (biofeedback therapy alone) group. These outcomes indicate that the scheme of transcutaneous electroacupuncture at the Baliao points can further improve postpartum urination disorders and aids in preventing postpartum PUR in parturients with labor analgesia. In conventional pelvic floor muscle biofeedback therapy, low-frequency electrodes are inserted slowly into the vagina to stimulate the pelvic floor muscle. This approach can help the parturient correctly locate the anal sphincter, contract the local muscles, exercise the pelvic floor muscle function, and promote the growth of local pelvic floor muscle strength, thereby beneficial for enhancing bladder function sensitivity[21]. However, merely stimulating the contraction of the pelvic floor muscles through the vagina cannot achieve the targeted point-to-point treatment. Therefore, the effect is slow. Percutaneous electrical stimulation of the Baliao acupoint is a reflexive mechanism therapy combined with meridian theory. Baliao (“caves”) resides in the lumbosacral region and belongs to the acupoints on the bladder meridian. Baliao acupoint stimulation can regulate the circulation of qi and blood in the organs and restore bladder opening and closing function, achieving a solid and anti-urinary effect. Moreover, modern medicine believes that the 1st–4th posterior branches of the sacral nerve pass through the posterior sacral foramen of the Baliao acupoint[22]. Therefore, transcutaneous electrical stimulation of the Baliao acupoint will have the same stimulating effect on the 1st–4th sacral nerve, thereby effectively regulating the contraction amplitude of the detrusor and other urinary muscles, promoting urinary reflex production, shortening the waiting time for urination, and reducing the bladder residual urine volume. In addition, pelvic floor muscle biofeedback electrical stimulation can activate the reflex pathway of the nonautonomous nervous system, inducing the involuntary contraction of the pelvic floor muscles through the anal scintillation reflex. Therefore, when transcutaneous electrical stimulation of the Baliao acupoint is combined with pelvic floor muscle biofeedback electrical stimulation, the contraction force of the anal sphincter and detrusor muscles is synergistically enhanced via different mechanisms of action, leading to improved coordination of the urinary muscles, further enhancement of the effectiveness of clinical interventions, and prevention of postpartum PUR in parturients undergoing labor analgesia.
Our study has some limitations. First, it is a single-center study with a small sample size. More samples are needed in future studies to confirm the value of the results. Second, labor analgesia in each patient may have different pain properties and accompanying symptoms, which may affect the tolerance of parturients to electrical stimulation and voltage amplitude regulation. Therefore, further exploring the changes in electromyographic evaluation of the combined therapy on parturients is necessary. The application value of this combined therapy in postpartum analgesia should also be further elucidated.
Percutaneous electrical stimulation of the Baliao acupoint combined with biofeedback can effectively improve the first self-urination time, first postpartum urine output, residual bladder urine output, and postpartum hemorrhage, reduce PUR occurrence, and improve the overall effectiveness of clinical intervention in postpartum mothers who received labor analgesia.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Peer-review report’s classification
Scientific Quality: Grade C
Novelty: Grade C
Creativity or Innovation: Grade B
Scientific Significance: Grade B
P-Reviewer: George TJ, United States S-Editor: Liu JH L-Editor: A P-Editor: Zhao S
| 1. | Mevorach Zussman N, Gonen N, Kovo M, Miremberg H, Bar J, Condrea A, Ginath S. Protracted postpartum urinary retention-a long-term problem or a transient condition? Int Urogynecol J. 2020;31:513-519. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 2. | Mohr S, Raio L, Gobrecht-Keller U, Imboden S, Mueller MD, Kuhn A. Postpartum urinary retention: what are the sequelae? A long-term study and review of the literature. Int Urogynecol J. 2022;33:1601-1608. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 18] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 3. | Long Q, Li J, Wen Y, He B, Li YZ, Yue CC, Du WL, Wan C. [Effect of electroacupuncture preconditioning combined with induced urination on urinary retention after milligan-morgan hemorrhoidectomy]. Zhongguo Zhen Jiu. 2019;39:821-824. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 4. | Wang XM, Gong J, Li SC, Han M. Acupuncture Compared with Intramuscular Injection of Neostigmine for Postpartum Urinary Retention: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Evid Based Complement Alternat Med. 2018;2018:2072091. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 5. | Liu Z, Liu Y, Liu B. Acupuncture for Stress Urinary Incontinence-Reply. JAMA. 2017;318:1500. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 6. | Chen XJ. Discussion on the Contents of the New Edition of "Meridians and Acupoints". Zhongguo Zhenjiu. 2014;34:1242-1244. [DOI] [Full Text] |
| 7. | Obstetrics and Gynecology Group of the Obstetrics and Gynecology Branch of the Chinese Medical Association. Guidelines for Prepregnancy and Pregnancy Health Care (2018). Zhonghua Fuchanke Zazhi. 2018;53:7-13. [RCA] [DOI] [Full Text] [Cited by in RCA: 21] [Reference Citation Analysis (0)] |
| 8. | Kawasoe I, Kataoka Y. Prevalence and risk factors for postpartum urinary retention after vaginal delivery in Japan: A case-control study. Jpn J Nurs Sci. 2020;17:e12293. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 9. | Nutaitis AC, Meckes NA, Madsen AM, Toal CT, Menhaji K, Carter-Brooks CM, Propst KA, Hickman LC. Postpartum urinary retention: an expert review. Am J Obstet Gynecol. 2023;228:14-21. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 14] [Reference Citation Analysis (0)] |
| 10. | Cadeddu F, Salis F, De Luca E, Ciangola I, Milito G. Efficacy of biofeedback plus transanal stimulation in the management of pelvic floor dyssynergia: a randomized trial. Tech Coloproctol. 2015;19:333-338. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 21] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 11. | Chen L, Wu YQ. Clinical efficacy of electrical stimulation biofeedback combined with pelvic floor muscle training in improving postpartum urinary retention. Linchuang Yu Binglixue Zazhi. 2021;41:2371-2376. [DOI] [Full Text] |
| 12. | Artymuk NV, Khapacheva SY. Device-assisted pelvic floor muscle postpartum exercise programme for the management of pelvic floor dysfunction after delivery. J Matern Fetal Neonatal Med. 2022;35:481-485. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 13. | Wallace SL, Miller LD, Mishra K. Pelvic floor physical therapy in the treatment of pelvic floor dysfunction in women. Curr Opin Obstet Gynecol. 2019;31:485-493. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 109] [Article Influence: 21.8] [Reference Citation Analysis (0)] |
| 14. | Liu H, Zhang J. [Analysis of ancient literature on baliao points for pelvic floor diseases]. Zhongguo Zhen Jiu. 2016;36:1327-1330. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 15. | Liu JT, Ding TH, Zhang RN, Liang FJ, Zhang RR, Shen YF. Electroacupuncture at Baliao point combined with acupoint injection for the treatment of neurogenic bladder dysfunction and its effect on urinary function reconstruction in patients. Shaanxi Zhongyi. 2022;43:653-657. [DOI] [Full Text] |
| 16. | Zhu JM, Sun ZR, Cui Y, Yin HN. Clinical observation of electroacupuncture at Baliao point in the treatment of neurogenic bladder after spinal cord injury. Guangzhou Zhongyiyao Daxue Xuebao. 2022;39:328-333. [DOI] [Full Text] |
| 17. | Neron M, Allègre L, Huberlant S, Mousty E, de Tayrac R, Fatton B, Letouzey V. Impact of systematic urinary catheterization protocol in delivery room on covert postpartum urinary retention: a before-after study. Sci Rep. 2017;7:17720. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 18. | Pan CY, Yang YY, Zheng JJ. The preventive effect of acupoint hot ironing of Ai Yanbao combined with pelvic floor muscle training on urinary retention after painless delivery of primipara. Zhongguo Yiyao Daobao. 2023;20:80-83. [DOI] [Full Text] |
| 19. | Cui G, Zhang Y, Liu Z, Li X, Sha M. Effect of Predictive Nursing Combined with Early Drinking Water Therapy on Patients with Urinary Retention after Vaginal Delivery. Comput Math Methods Med. 2022;2022:4204762. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 20. | Yoshida A, Yoshida M, Kawajiri M, Takeishi Y, Nakamura Y, Yoshizawa T. Prevalence of urinary retention after vaginal delivery: a systematic review and meta- analysis. Int Urogynecol J. 2022;33:3307-3323. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 21. | Alouini S, Memic S, Couillandre A. Pelvic Floor Muscle Training for Urinary Incontinence with or without Biofeedback or Electrostimulation in Women: A Systematic Review. Int J Environ Res Public Health. 2022;19. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 36] [Article Influence: 12.0] [Reference Citation Analysis (0)] |
| 22. | Athwal BS, Berkley KJ, Hussain I, Brennan A, Craggs M, Sakakibara R, Frackowiak RS, Fowler CJ. Brain responses to changes in bladder volume and urge to void in healthy men. Brain. 2001;124:369-377. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 260] [Cited by in RCA: 237] [Article Influence: 9.9] [Reference Citation Analysis (0)] |