Published online May 16, 2024. doi: 10.12998/wjcc.v12.i14.2457
Revised: March 9, 2024
Accepted: April 3, 2024
Published online: May 16, 2024
Processing time: 73 Days and 7.3 Hours
Acute lower gastrointestinal bleeding (LGIB) is a common occurrence in clinical practice. However, appendiceal bleeding is an extremely rare condition that can easily be overlooked and misdiagnosed. The preoperative detection of appen
We presented a case of a 33-year-old female who complained of hematochezia that had lasted for 1 d. Colonoscopy revealed continuous bleeding in the appen
The preoperative detection of appendiceal bleeding is often challenging, colo
Core Tip: Acute lower gastrointestinal bleeding (LGIB) is common, however, appendiceal bleeding is extremely rare. The diagnosis of appendiceal bleeding is challenging because of its rarity and lack of related guidelines and consensus. Colonoscopy is extremely important, and bowel preparation is not routinely recommended for patients with acute LGIB. Laparoscopic appendectomy is the most appropriate treatment for appendiceal bleeding.
- Citation: Ma Q, Du JJ. Appendiceal bleeding caused by vascular malformation: A case report. World J Clin Cases 2024; 12(14): 2457-2462
- URL: https://www.wjgnet.com/2307-8960/full/v12/i14/2457.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i14.2457
Lower gastrointestinal bleeding (LGIB) is defined as hemorrhage originating from the gastrointestinal tract segment below the Treitz ligament[1]. Various diagnostic modalities, including digital subtraction angiography (DSA), computed tomography angiography (CTA) and colonoscopy, are used for appropriate diagnosis. However, pinpointing the source of bleeding remains a significant challenge[2]. Only a few guidelines and a consensus on LGIB, especially, no major gui
A 33-year-old female presented to our hospital with hematochezia that had lasted for 1 d.
The patient reported a prior episode of passing approximately 300 mL of bloody stool before presenting to the hospital. There were no accompanying gastrointestinal symptoms, such as nausea, vomiting, or abdominal pain. Following the administration of 4 L of polyethylene glycol (PEG)-based bowel preparation, the patient experienced another episode of bloody stool, amounting to approximately 300 mL. The patient denied any previous history of hematochezia.
The patient had no history of acute or chronic infectious diseases, heart disease, hypertension or diabetes, or surgery.
The patient had not recently taken any medicine, such as corticosteroids or nonsteroidal anti-inflammatory drugs. There was no family history of similar cases or bleeding disorders.
There were no signs of anemia, her blood pressure was 100/54 mmHg, and her heart rate was 96 beats per minute. The patient did not have any pathological signs.
Her hemoglobin level was 134 g/L (normal range: 130-175 g/L), her leucocyte count was 15.87 × 109/L, and her per
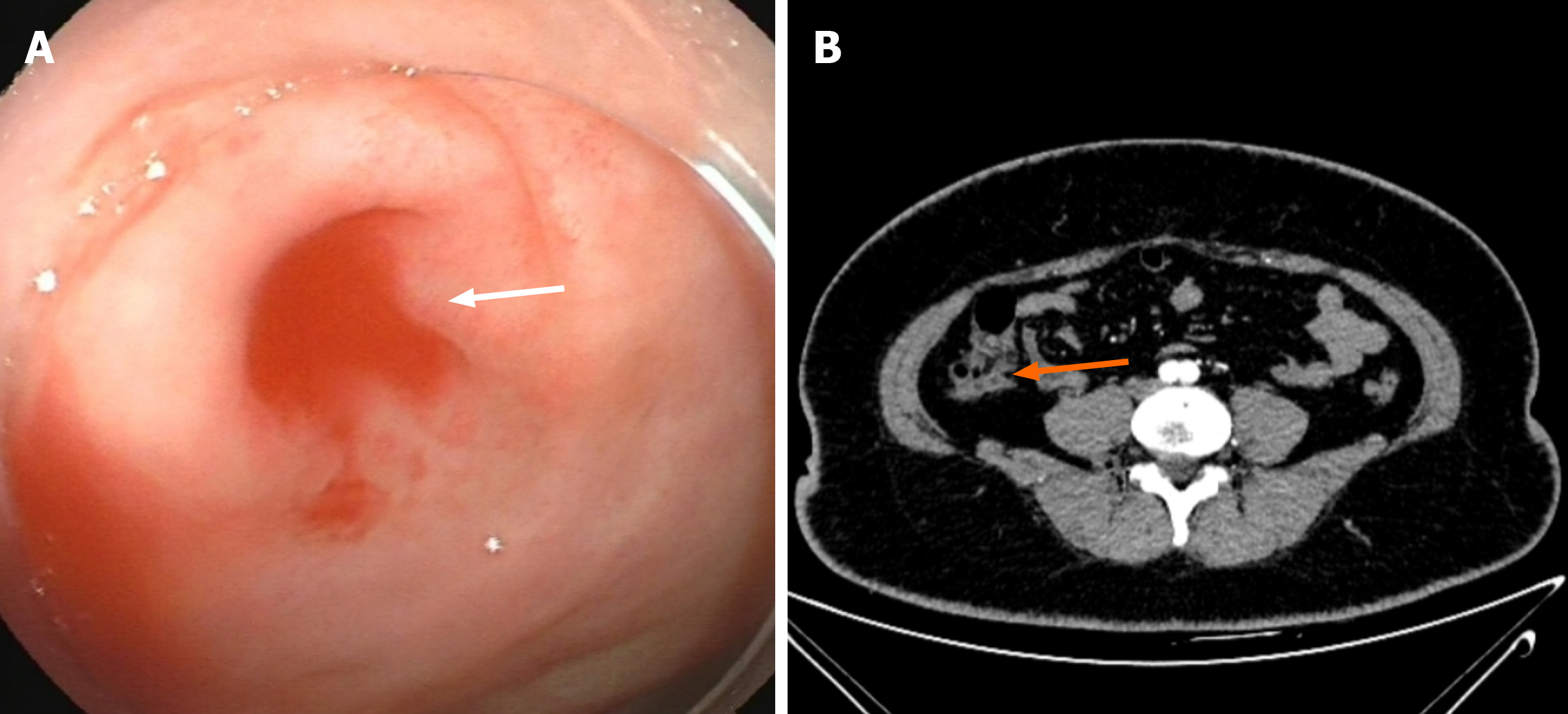
An emergency colonoscopy was performed, and the endoscope was extended to the terminal ileum. Continuous bleeding was observed at the appendiceal orifice (Figure 1A). In addition, a contrast-enhanced abdominal computed tomography scan revealed structural disorder in the ileocecal area, and the appendix was not clear (Figure 1B).
Appendiceal bleeding.
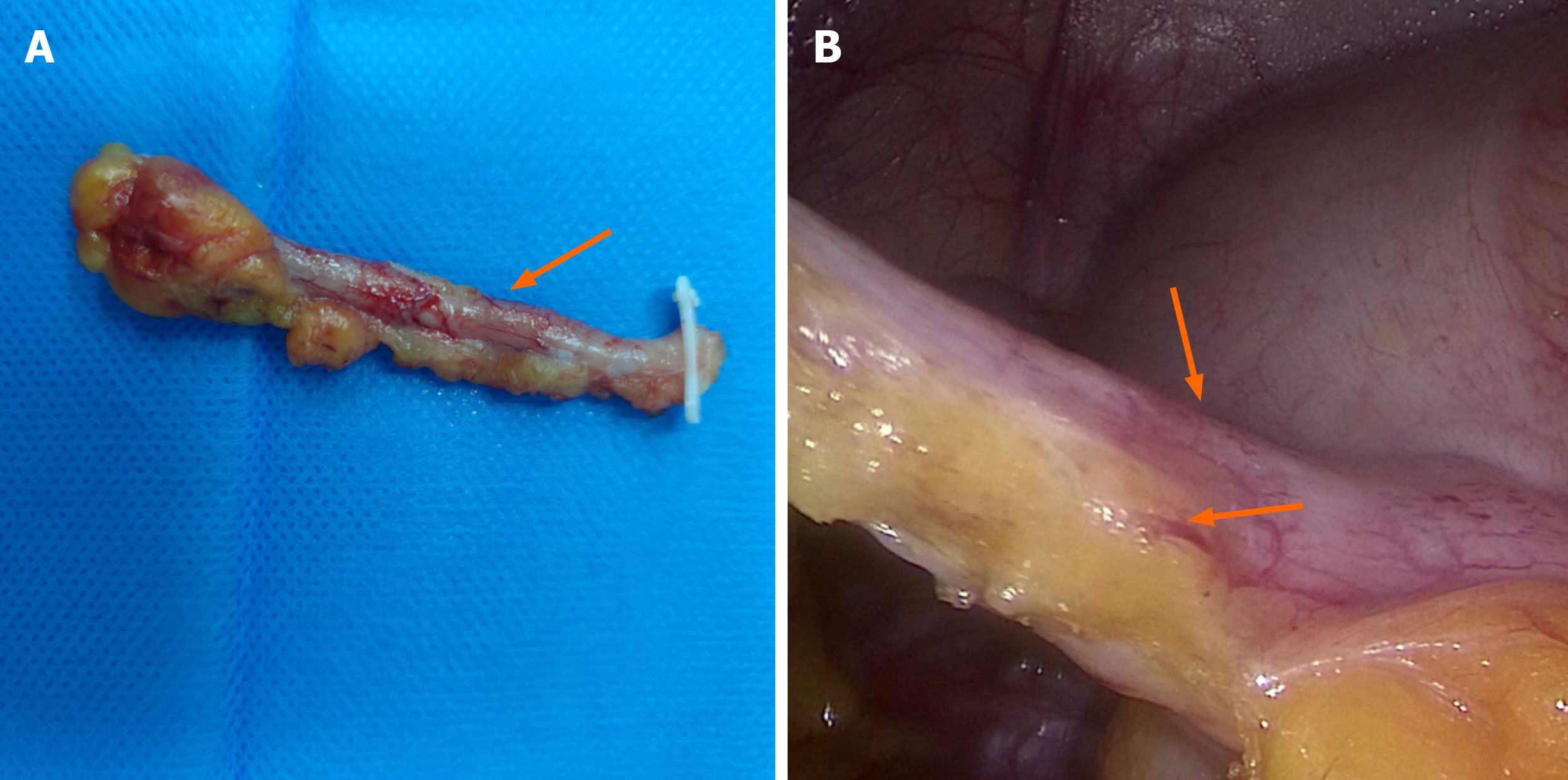
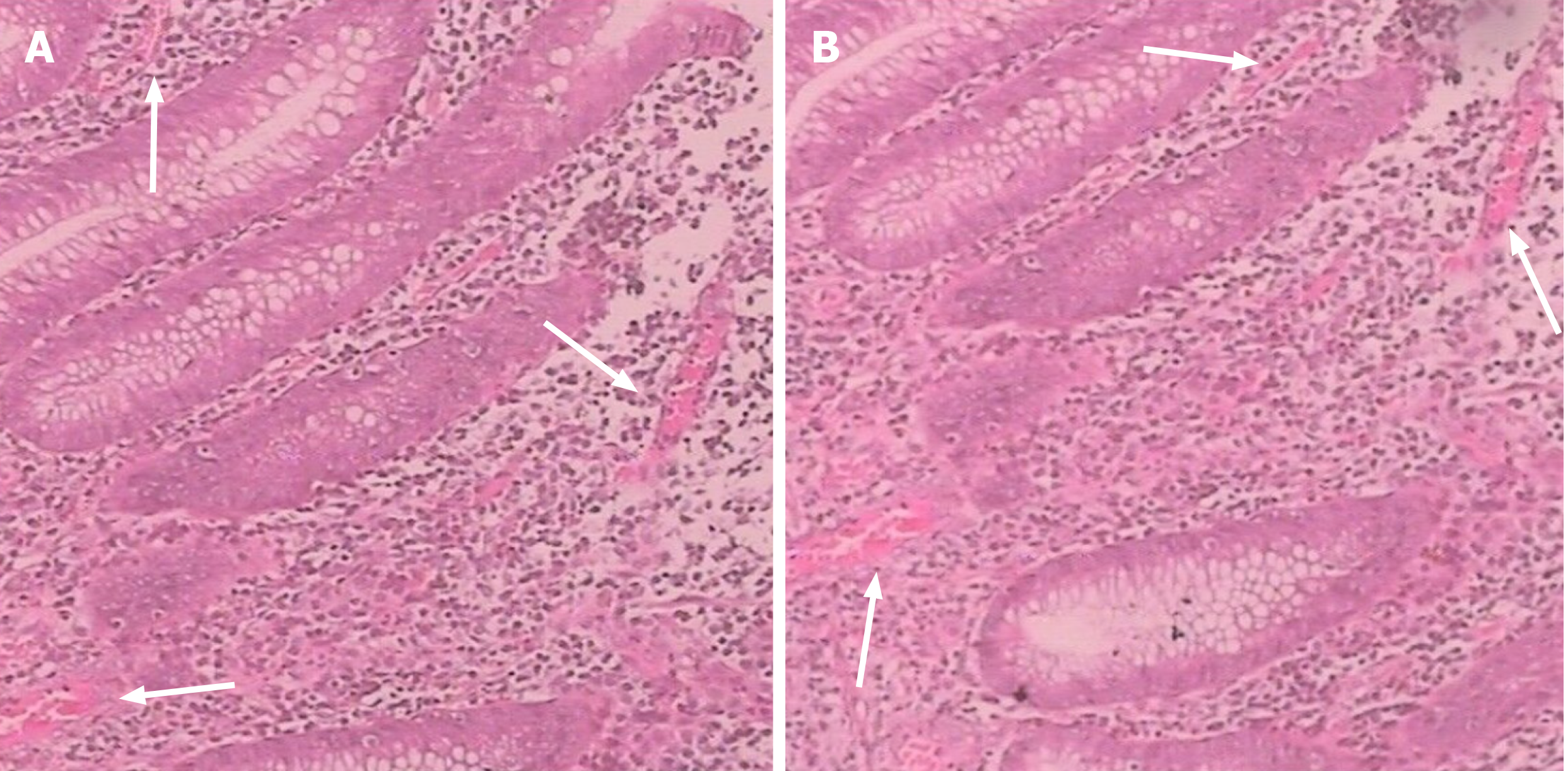
An emergency laparoscopic appendectomy was performed. During the surgery, the appendix was 90 mm × 5 mm in size and the appendix was swollen 3-5 cm from the appendicular root (Figure 2A). A pulsating blood vessel was observed in the mesangium of the appendix (Figure 2B). Active bleeding into the appendicular lumen was considered, and a large number of blood clots were observed in the lumen. Pathologically, a large number of hyperplastic vessels were observed in the appendix mucosa and capillary vessels were dilated (Figure 3).
The patient had no recurrent hematochezia or melena, and was discharged from the hospital 5 d after the surgery. One month later, no evidence of rebleeding was observed.
Acute LGIB is not an uncommon condition, with an incidence of approximately 0.02%, and it is more common in men and older people. Approximately 80% of cases are of colorectal origin, and appendiceal bleeding is extremely rare[4,5]. A search of the PubMed/MEDLINE database for literature published between 2010 and August 2023 regarding “ap
| Case | Age (yr)/sex | Techniques | Treatment | Complications | Pathology | Ref. |
| 1 | 32/male | Colonoscopy | Endoscopic appendectomy | None | Appendiceal ulcer | [2] |
| 2 | 90/male | Colonoscopy | Laparoscopic appendectomy | None | Unknown | [3] |
| 3 | 70/male | Colonoscopy | Endoscopic clipping | None | None | [4] |
| 4 | 25/male | Colonoscopy | Appendectomy | None | Appendiceal mucosal erosion | [5] |
| 5 | 54/male | Colonoscopy | Appendectomy | None | Unknown | [10] |
| 6 | 32/male | Colonoscopy | Laparoscopic appendectomy | None | Dieulafoy’s lesion | [10] |
| 7 | 72/male | Colonoscopy | Laparoscopic appendectomy and cecum wedge resection | None | Vascular malformation | [11] |
| 8 | 73/male | Colonoscopy | Appendectomy | None | Appendiceal mucosal erosion | [12] |
| 9 | 32/male | Colonoscopy | Appendectomy | None | Appendiceal ulcer | [13] |
| 10 | 72/male | Colonoscopy | Right hemicolectomy | None | Appendiceal mucinous adenocarcinoma | [14] |
| 11 | 49/male | Colonoscopy | Appendectomy with partial cecal resection | None | Acute appendicitis | [15] |
| 12 | 88/male | Colonoscopy | Appendectomy | None | Low-grade mucinous neoplasm of appendix | [16] |
| 13 | 42/male | Colonoscopy | Laparoscopic appendectomy | None | Appendiceal mucosal erosion | [17] |
| 14 | 44/male | Colonoscopy | Colonoscopic clipping | None | None | [18] |
| 15 | 34/female | Colonoscopy | Colonoscopic clipping | None | None | [19] |
| 16 | 67/male | Angiogram | Embolization the appendiceal artery | Acute appendicitis | None | [20] |
| Our case | 33/female | Colonoscopy | Laparoscopic appendectomy | None | Vascular malformation |
The diagnosis of appendiceal bleeding mainly includes CTA, DSA and colonoscopy. CTA is suitable for patients with active bleeding (bleeding rate ≥ 0.3 mL/min). Additionally, DSA is affected by the bleeding rate. When the bleeding rate is greater than 0.5 mL/min, the detection rate reaches 50%–72%, but if the bleeding rate is lower than 0.5 mL/min, the detection rate decreases significantly[6]. Colonoscopy plays an irreplaceable role for LGIB, at least to the terminal ileum[7].
No consensus exists regarding on bowel preparation before emergency colonoscopy for LGIB. Some scholars believe that adequate bowel preparation and clear exposure under the scope are the basis for discovering and treating all lesions, and recommend 4-6 L of PEG-based bowel preparation; in addition, split-dose preparation and/or the use of low-volume preparations can also be considered[8]. However, some scholars believe that oral laxatives can aggravate gastrointestinal bleeding and shock[9]. According to our case, the patient experienced massive hematocheia again after receiving oral laxatives. We believe that bowel preparation is not routinely recommended for patients with acute LGIB or that only low-dose bowel preparation is recommended for the following reasons: (1) Aggravation of gastrointestinal bleeding; (2) The equipment used for colonoscopy is more advanced, and which can be observed while washing, therefore, it is helpful to find and treat the lesion site; and (3) The blood in the intestinal lumen itself has a cathartic effect.
No standard treatment is available for appendiceal bleeding, and it has been reported that local spraying of hemostatic drugs can successfully stop bleeding. Hemostasis can also be achieved by endoscopic clamping of part of the appendiceal orifice or appendiceal artery embolization[4,10,11]. The choice for most scholars is appendectomy[3]. In our case, the site of bleeding in the patient's appendix was approximately 3 cm from the orifice, and the appendix was slender. The he
The number of reports on appendiceal bleeding is limited, and there is a lack of corresponding guidelines and con
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Mori H, Belgium S-Editor: Zheng XM L-Editor: A P-Editor: Xu ZH
| 1. | Barnert J, Messmann H. Diagnosis and management of lower gastrointestinal bleeding. Nat Rev Gastroenterol Hepatol. 2009;6:637-646. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 115] [Cited by in RCA: 105] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 2. | Dung LT, Hung ND, Phuong LTH, Khuong NH, Thien LQ, Duy NQ, Nhu TN, Duc NM. Appendiceal hemorrhage: An uncommon cause of lower gastrointestinal tract bleeding and intraluminal contrast extravasation. Radiol Case Rep. 2023;18:2232-2236. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Reference Citation Analysis (0)] |
| 3. | Maeda Y, Saito S, Ohuchi M, Tamaoki Y, Nasu J, Baba H. Appendiceal bleeding in an elderly male: a case report and a review of the literature. Surg Case Rep. 2021;7:147. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 5] [Article Influence: 1.3] [Reference Citation Analysis (1)] |
| 4. | Chung IH, Kim KH. A case of successful colonoscopic treatment of acute appendiceal bleeding by endoclips. J Korean Soc Coloproctol. 2011;27:329-332. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 5. | Chiang CC, Tu CW, Liao CS, Shieh MC, Sung TC. Appendiceal hemorrhage -- an uncommon cause of lower gastrointestinal bleeding. J Chin Med Assoc. 2011;74:277-279. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 6. | Xiao X, Palihati S, Zhou M, Zeng Y, Yang JL. [Lower Gastrointestinal Bleeding: Current State of Diagnosis and Treatment and Interpretation of the Clinical Guidelines]. Sichuan Da Xue Xue Bao Yi Xue Ban. 2022;53:367-374. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 7. | Strate LL, Gralnek IM. ACG Clinical Guideline: Management of Patients With Acute Lower Gastrointestinal Bleeding. Am J Gastroenterol. 2016;111:459-474. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 262] [Cited by in RCA: 300] [Article Influence: 33.3] [Reference Citation Analysis (2)] |
| 8. | Triantafyllou K, Gkolfakis P, Gralnek IM, Oakland K, Manes G, Radaelli F, Awadie H, Camus Duboc M, Christodoulou D, Fedorov E, Guy RJ, Hollenbach M, Ibrahim M, Neeman Z, Regge D, Rodriguez de Santiago E, Tham TC, Thelin-Schmidt P, van Hooft JE. Diagnosis and management of acute lower gastrointestinal bleeding: European Society of Gastrointestinal Endoscopy (ESGE) Guideline. Endoscopy. 2021;53:850-868. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 133] [Cited by in RCA: 112] [Article Influence: 28.0] [Reference Citation Analysis (0)] |
| 9. | Green BT, Rockey DC. Lower gastrointestinal bleeding--management. Gastroenterol Clin North Am. 2005;34:665-678. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 19] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 10. | Park I, Kwon CI, Ko KH, Hong SP, Park PW. Colonoscopic clipping as a treatment for appendiceal bleeding. Gut Liver. 2010;4:411-414. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 11. | Smith EJ, Coventry C, Taylor J, De'ath H, Haque A. A case of endovascular management to gain control of a lower gastrointestinal haemorrhage caused by appendiceal artery bleeding. J Surg Case Rep. 2021;2021:rjab204. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 12. | Murakami D, Harada H, Amano Y. An unexpected cause of lower gastrointestinal bleeding. Clin Case Rep. 2021;9:586-587. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |
| 13. | Zhou SY, Guo MD, Ye XH. Appendiceal bleeding: A case report. World J Clin Cases. 2022;10:6314-6318. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 14. | Choi JM, Lee SH, Ahn BK, Baek SU. Hematochezia due to Angiodysplasia of the Appendix. Ann Coloproctol. 2016;32:117-119. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 7] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 15. | Chung KS, Gao JP. Massive lower gastrointestinal bleeding from the appendix. Gut Liver. 2011;5:234-237. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 16. | Liu Z, Hou R, Bai X. The culprit of turbulent lower gastrointestinal bleeding: The appendiceal ulcer. Asian J Surg. 2022;45:2761-2762. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 17. | Wijayaratne HWTD, Fernando KJA, Matheeshan T. A Case Report on Life-Threatening Lower Gastrointestinal Bleeding: A Rare Presentation of Mucinous Adenocarcinoma of the Appendix. Case Rep Surg. 2021;2021:2349737. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 18. | Kim DH, Lee JH, Kim D, Hwang S, Kang K, Koo JS. [Acute Suppurative Appendicitis Diagnosed by Acute Lower Gastrointestinal Hemorrhage]. Korean J Gastroenterol. 2019;73:45-49. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 19. | Karatas M, Simsek C, Gunay S, Zengel B, Okut G, Yıldırım AM, Vardar E, Uslu A. Acute lower gastrointestinal bleeding due to low-grade mucinous neoplasm of appendix. Acta Chir Belg. 2022;122:357-360. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Reference Citation Analysis (0)] |
| 20. | Baek SK, Kim YH, Kim SP. Acute lower gastrointestinal bleeding due to appendiceal mucosal erosion. Surg Laparosc Endosc Percutan Tech. 2010;20:e110-e113. [PubMed] |