Published online May 6, 2024. doi: 10.12998/wjcc.v12.i13.2237
Peer-review started: November 26, 2023
First decision: February 5, 2024
Revised: February 17, 2024
Accepted: April 3, 2024
Article in press: May 6, 2024
Published online: May 6, 2024
Processing time: 151 Days and 1.2 Hours
Breast conservation surgery (BCS) with adjuvant radiotherapy has become a gold standard in the treatment of early-stage breast cancer, significantly reducing the risk of tumor recurrence. However, this treatment is associated with adverse effects, including the rare but aggressive radiation-induced angiosarcoma (RIAS). Despite its rarity and nonspecific initial presentation, RIAS presents a challenging diagnosis, emphasizing the importance of imaging techniques for early detection and accurate diagnosis.
We present a case of a 48-year-old post-menopausal woman who developed skin ecchymosis on the right breast seven years after receiving BCS and adjuvant radiotherapy for breast cancer. Initial mammography and ultrasound were inconclusive, showing post-treatment changes but failing to identify the under
Breast MRI is crucial for detecting RIAS, especially when mammography and ultrasound are inconclusive.
Core Tip: Radiation-induced angiosarcoma (RIAS) of the breast is extremely rare and aggressive complication of the radiotherapy. The diagnosis is difficult clinically, radiologically and even pathologically. Mammography and ultrasound findings of RIAS are nonspecific and may be occult on the initial conventional breast imaging. Breast magnetic resonance imaging can provide better morphologic characterization and extent of disease, which is critical in surgical planning and preventing delays in diagnosis.
- Citation: Wu WP, Lee CW. Magnetic resonance imaging findings of radiation-induced breast angiosarcoma: A case report. World J Clin Cases 2024; 12(13): 2237-2242
- URL: https://www.wjgnet.com/2307-8960/full/v12/i13/2237.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i13.2237
Breast conservation surgery (BCS) with adjuvant radiotherapy is becoming the gold standard treatment for patients with early breast cancer (stage I and II) over the decades[1-3]. The use of radiotherapy reduces the chance of tumor recurrence and subsequent morbidity and mortality[4,5]. However, the adverse cutaneous effects of radiotherapy include early and late reactions, including erythema, hyperpigmentation, telangiectasia, chronic radiation dermatitis and radiation-induced fibrosis[6]. However, radiotherapy has been associated with development of secondary soft-tissue sarcomas, with angiosarcoma emerging as the most common subtype, so called radiation-induced angiosarcoma (RIAS)[7-9]. RIAS is a rare and aggressive complication of radiation therapy. In patients undergoing BCS and adjuvant radiotherapy, the estimated incidence of RIAS is 0.05%–0.3%[10].
Mammography and ultrasound are reported to show mostly post-treatment changes, whereas contrast-enhanced breast magnetic resonance imaging (MRI) has been reported to be more sensitive in detecting skin enhancement of RIAS.
In this case report, we present the clinical course and MRI findings in a patient with RIAS presenting 7 years after treatment of breast cancer.
A 48-year-old post-menopausal woman presented with skin ecchymosis on her right breast, which had developed several months earlier.
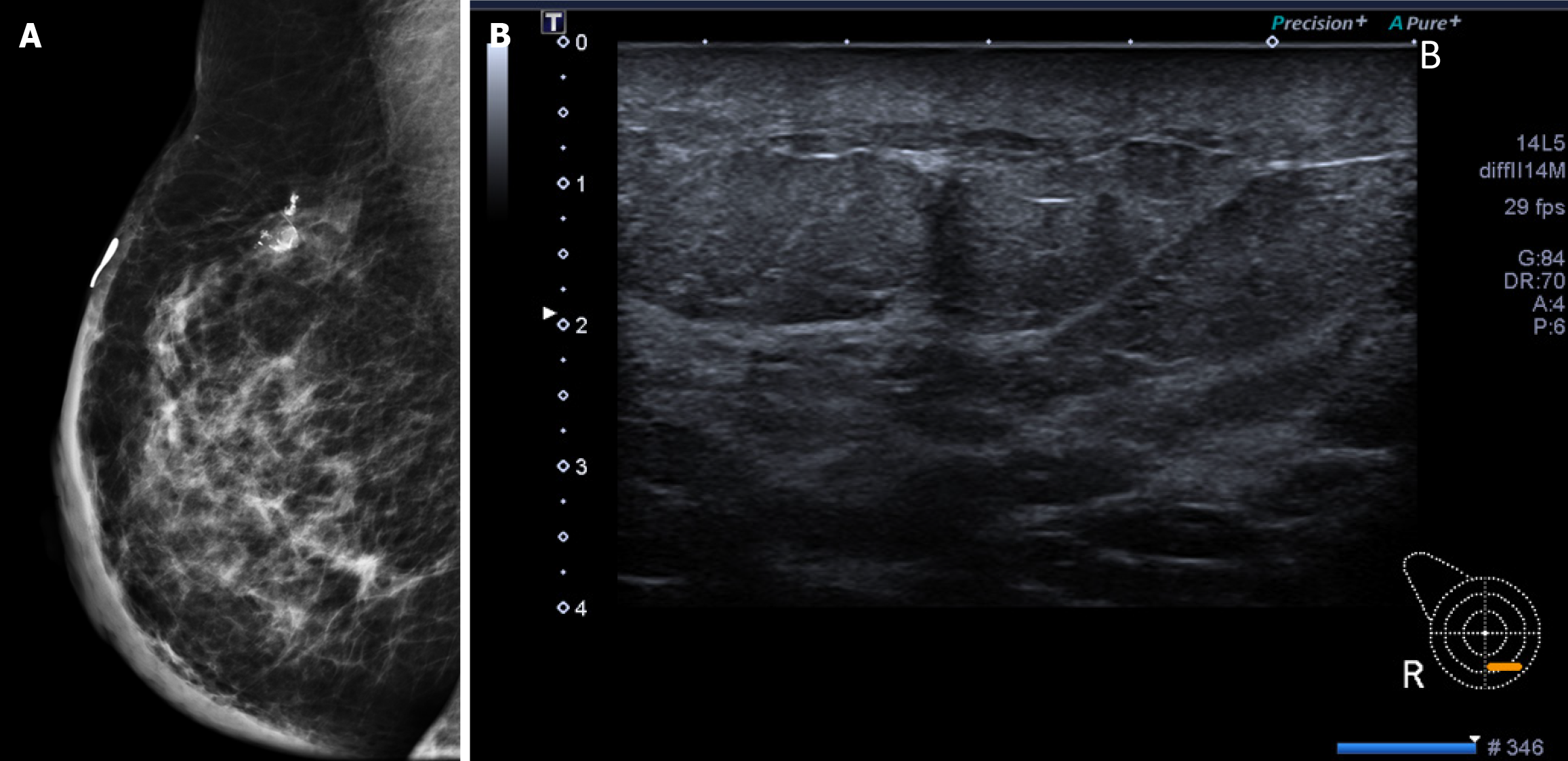
The patient noticed a non-painful skin ecchymosis around the previous surgical scar on her right breast, which had been enlarging over the past several months (Figure 1).
Seven years ago, the patient underwent BCS for breast cancer on the right breast, followed by adjuvant radiotherapy. The pathology of the tumor showed a 0.6 cm dimension, classified as ypT1bN0M0. Axillary lymph node dissection was performed with no tumor found in the lymph nodes. The patient received a total radiotherapy dose of 60 Gy over 30 fractions and was on Tamoxifen 20 mg daily for 5 years. Follow-up examinations showed no clinical evidence of recurrent tumor or upper-extremity lymphedema.
The patient had no relevant personal or family history of breast cancer or other genetic disorders.
Physical examination revealed a non-painful skin ecchymosis around the surgical scar on the right breast.
The patient had no specific laboratory examinations in relation to the diagnosis of the condition.
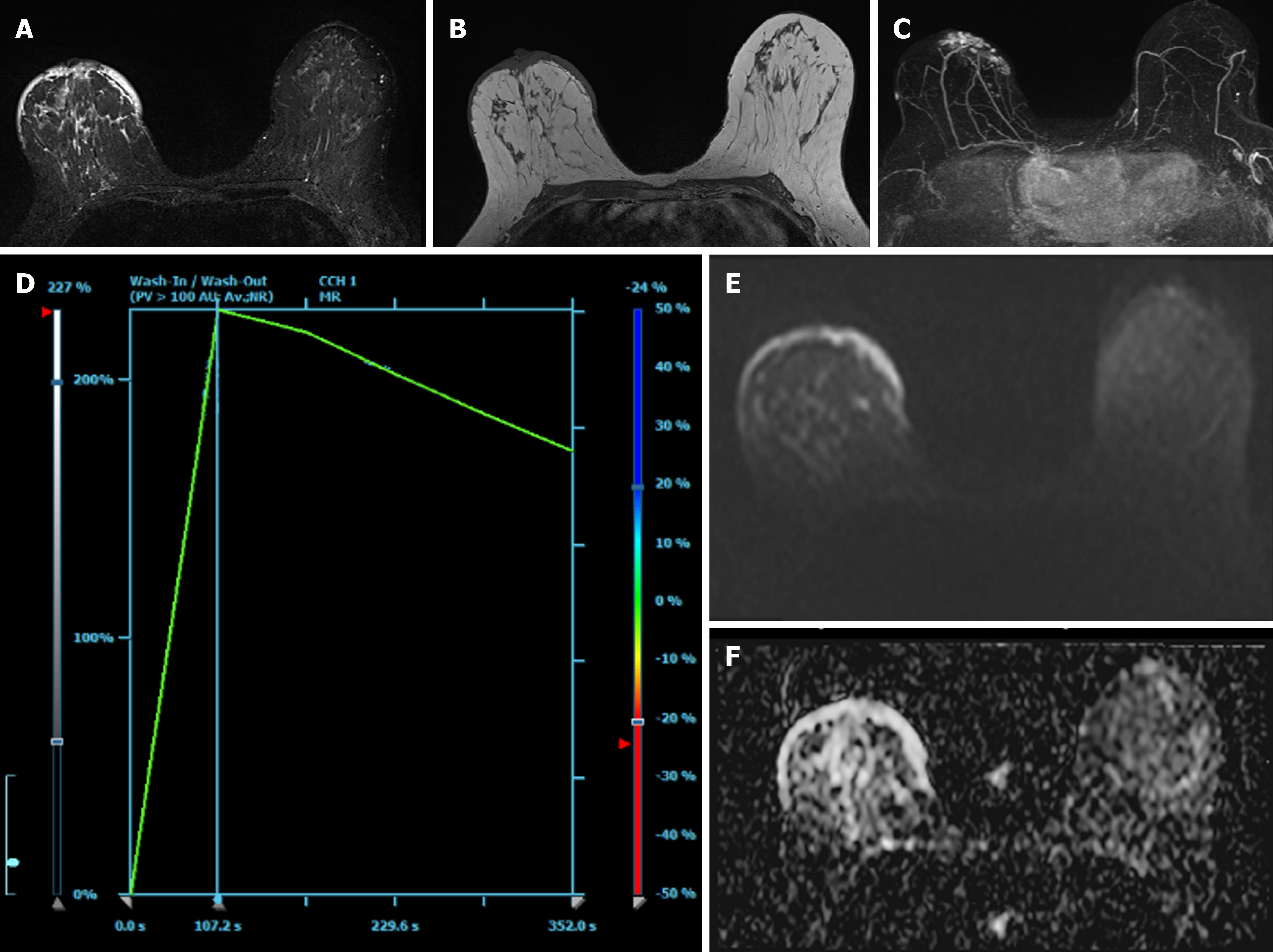
Mammography (Figure 2A) and ultrasound (Figure 2B) showed negative results for recurrent breast carcinoma but indicated post-operative changes such as skin thickening. Despite these findings, the clinician suspected the condition could be either a breast hematoma or recurrent breast carcinoma. For the problem solving, contrast-enhanced breast MRI (Figure 3) was performed and revealed diffuse skin thickening and nodularity, which showed hyperintensity on T2-weighted images and isointensity on T1-weighted images, with fast arterial enhancement on post-contrast dynamic series. The enhancement kinetics of cutaneous lesion shows rapid wash-in and wash-out (type 3 curve)[11]. No discrete intraparenchymal masses were present. Consequently, a diagnosis of radiation-induced angiosarcoma of breast or local tumor recurrence was made.
The final diagnosis was radiation-induced angiosarcoma of the breast, confirmed by excision biopsy findings.
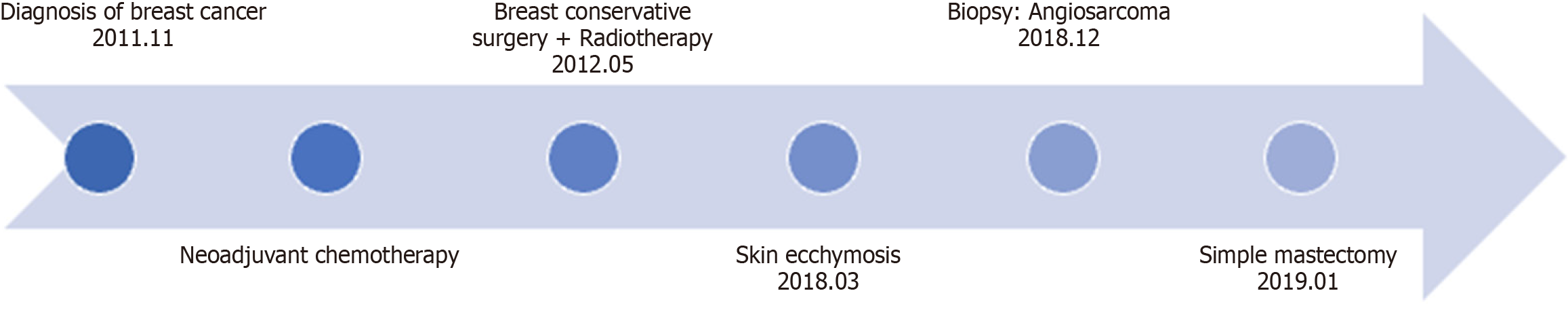
Given the MRI findings indicative of diffuse involvement of the right breast with angiosarcoma and the natural course of the disease, the patient elected to undergo right simple mastectomy. The timeline of this case report was illustrated as Figure 4.
The mastectomy procedure was successful, with a gross examination revealing an irregular firm tumor measuring 12.1 cm in the greatest dimension. All margins were tumor-free. There was no mention of distant metastases on subsequent positron emission tomography/computed tomography scans. No recurrence or metastases observed during follow-up.
Angiosarcoma of the breast is a rare, highly aggressive malignant tumor of the vascular endothelium by the World Health Organization[12]. It accounts for 0.05% of all reported breast cancers, making them the rarest in that category[7,13,14]. It can be either primary or secondary. Primary angiosarcoma occurs in young women, with a median age of onset of 40 years. Secondary angiosarcoma occurs in older women with a history of BCS and radiotherapy[15], or chronic lymphedema, so called Stewart-Treves angiosarcomas[16].
The clinical differential diagnosis of angiosarcoma may include recurrent breast carcinoma, radiation-related morphea, and malignant melanoma. Results of mammography and ultrasound are not diagnostic for angiosarcoma and are typically negative in early disease. Clinical suspicion is the key to making an early diagnosis. Diagnosis prior to surgery, either by core needle biopsy or fine needle aspiration, is difficult. Chen et al[17] reported that a false negative result of core needle biopsy can achieve 37%. In this situation, a full-thickness incisional or excisional biopsy is required to ensure adequate sampling of the lesion.
Because the rarity and seeming harmless presentation, physicians and patients may frequently neglect initial symptoms and clinical findings with consequent diagnostic delay[18-20]. Chikarmane et al[21] reported that over half of the patients with RIAS have skin thickenings with post-radiation and lumpectomy changes on mammogram and ultrasound. Only one-quarter of RIAS were observed to involve intraparenchymal regions, presenting as irregular masses. Due to post-radiation alterations such as skin thickening, identifying predominantly cutaneous lesions on mammography and ultrasound may pose particular challenges.
The important role of breast MRI plays in the diagnosis and determination of disease extent. Salminen et al[7] reported that the spectrum of RIAS imaging findings was broad, but the majority of patients (63%) had enhancing skin thickening or discrete plaque-like enhancing in the skin. In our case, the cutaneous lesion demonstrated rapid arterial enhancement and washout on the dynamic series. Associated diffuse skin thickenings were hyperintense on T2-weighted images and isointense on T1-weighted images. Sanders et al[22] hypothesized in his study that the T2 hyperintense skin thickening with persistent enhancement could be related to post-radiation inflammatory changes, and foci with rapid early arterial enhancement and washout could represent tumor foci. Our case has the same findings on the breast MRI. In the patient with RIAS, contrast-enhanced breast MRI study could have important diagnostic potential to evaluate the true extent of disease.
We present this case to emphasize that, due to the nonspecific findings on mammography or ultrasound, breast MRI offers superior morphological characterization and assessment of disease extent. This is crucial for surgical planning and avoiding diagnostic delays. If an enhancing cutaneous lesion is detected on contrast-enhanced breast MRI at a postoperative and irradiated site, clinicians should consider the possibility of cutaneous angiosarcoma.
This case emphasizes the importance of considering radiation-induced angiosarcoma in patients presenting with skin changes post-radiotherapy for breast cancer. MRI plays a critical role in diagnosing and assessing the extent of the disease, especially when other imaging modalities are inconclusive. Early diagnosis and appropriate surgical intervention are crucial for managing this rare but aggressive complication.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Oncology
Country/Territory of origin: Taiwan
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Singh R, India S-Editor: Liu JH L-Editor: A P-Editor: Zhao S
| 1. | Franceschini G, Martin Sanchez A, Di Leone A, Magno S, Moschella F, Accetta C, Masetti R. New trends in breast cancer surgery: a therapeutic approach increasingly efficacy and respectful of the patient. G Chir. 2015;36:145-152. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 15] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 2. | Fisher B, Anderson S, Bryant J, Margolese RG, Deutsch M, Fisher ER, Jeong JH, Wolmark N. Twenty-year follow-up of a randomized trial comparing total mastectomy, lumpectomy, and lumpectomy plus irradiation for the treatment of invasive breast cancer. N Engl J Med. 2002;347:1233-1241. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4341] [Cited by in RCA: 4259] [Article Influence: 185.2] [Reference Citation Analysis (0)] |
| 3. | Veronesi U, Cascinelli N, Mariani L, Greco M, Saccozzi R, Luini A, Aguilar M, Marubini E. Twenty-year follow-up of a randomized study comparing breast-conserving surgery with radical mastectomy for early breast cancer. N Engl J Med. 2002;347:1227-1232. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3029] [Cited by in RCA: 2935] [Article Influence: 127.6] [Reference Citation Analysis (0)] |
| 4. | Overgaard M, Hansen PS, Overgaard J, Rose C, Andersson M, Bach F, Kjaer M, Gadeberg CC, Mouridsen HT, Jensen MB, Zedeler K. Postoperative radiotherapy in high-risk premenopausal women with breast cancer who receive adjuvant chemotherapy. Danish Breast Cancer Cooperative Group 82b Trial. N Engl J Med. 1997;337:949-955. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1975] [Cited by in RCA: 1876] [Article Influence: 67.0] [Reference Citation Analysis (0)] |
| 5. | Ragaz J, Jackson SM, Le N, Plenderleith IH, Spinelli JJ, Basco VE, Wilson KS, Knowling MA, Coppin CM, Paradis M, Coldman AJ, Olivotto IA. Adjuvant radiotherapy and chemotherapy in node-positive premenopausal women with breast cancer. N Engl J Med. 1997;337:956-962. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1348] [Cited by in RCA: 1268] [Article Influence: 45.3] [Reference Citation Analysis (0)] |
| 6. | Bray FN, Simmons BJ, Wolfson AH, Nouri K. Acute and Chronic Cutaneous Reactions to Ionizing Radiation Therapy. Dermatol Ther (Heidelb). 2016;6:185-206. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 155] [Cited by in RCA: 238] [Article Influence: 26.4] [Reference Citation Analysis (0)] |
| 7. | Salminen SH, Sampo MM, Böhling TO, Salo J, Tarkkanen M, Blomqvist CP, Hukkinen K. Radiation-associated angiosarcoma of the breast: analysis of diagnostic tools in a registry-based population. Acta Radiol. 2022;63:22-27. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 9] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 8. | Billings SD, McKenney JK, Folpe AL, Hardacre MC, Weiss SW. Cutaneous angiosarcoma following breast-conserving surgery and radiation: an analysis of 27 cases. Am J Surg Pathol. 2004;28:781-788. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 188] [Cited by in RCA: 158] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 9. | Rubino C, Shamsaldin A, Lê MG, Labbé M, Guinebretière JM, Chavaudra J, de Vathaire F. Radiation dose and risk of soft tissue and bone sarcoma after breast cancer treatment. Breast Cancer Res Treat. 2005;89:277-288. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 114] [Cited by in RCA: 117] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 10. | Cohen-Hallaleh RB, Smith HG, Smith RC, Stamp GF, Al-Muderis O, Thway K, Miah A, Khabra K, Judson I, Jones R, Benson C, Hayes AJ. Radiation induced angiosarcoma of the breast: outcomes from a retrospective case series. Clin Sarcoma Res. 2017;7:15. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 23] [Cited by in RCA: 38] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 11. | Mercado CL. BI-RADS update. Radiol Clin North Am. 2014;52:481-487. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 100] [Cited by in RCA: 152] [Article Influence: 13.8] [Reference Citation Analysis (0)] |
| 12. | Tan PH, Ellis I, Allison K, Brogi E, Fox SB, Lakhani S, Lazar AJ, Morris EA, Sahin A, Salgado R, Sapino A, Sasano H, Schnitt S, Sotiriou C, van Diest P, White VA, Lokuhetty D, Cree IA; WHO Classification of Tumours Editorial Board. The 2019 World Health Organization classification of tumours of the breast. Histopathology. 2020;77:181-185. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 362] [Cited by in RCA: 473] [Article Influence: 94.6] [Reference Citation Analysis (0)] |
| 13. | Iacoponi S, Calleja J, Hernandez G, Sainz de la Cuesta R. Primary breast angiosarcoma in a young woman. Int J Surg Case Rep. 2016;24:101-103. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 12] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 14. | Russo D, Campanino MR, Cepurnaite R, Gencarelli A, De Rosa F, Corvino A, Menkulazi M, Tammaro V, Fuggi M, Insabato L. Primary High-Grade Angiosarcoma of the Breast in a Young Woman With Breast Implants: A Rare Case and a Review of Literature. Int J Surg Pathol. 2020;28:906-912. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 3] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 15. | Buatti JM, Harari PM, Leigh BR, Cassady JR. Radiation-induced angiosarcoma of the breast. Case report and review of the literature. Am J Clin Oncol. 1994;17:444-447. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 40] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 16. | STEWART FW, TREVES N. Lymphangiosarcoma in postmastectomy lymphedema; a report of six cases in elephantiasis chirurgica. Cancer. 1948;1:64-81. [PubMed] [DOI] [Full Text] |
| 17. | Chen KT, Kirkegaard DD, Bocian JJ. Angiosarcoma of the breast. Cancer. 1980;46:368-371. [PubMed] [DOI] [Full Text] |
| 18. | Daniels BH, Ko JS, Rowe JJ, Downs-Kelly E, Billings SD. Radiation-associated angiosarcoma in the setting of breast cancer mimicking radiation dermatitis: A diagnostic pitfall. J Cutan Pathol. 2017;44:456-461. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 9] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 19. | Cabete J, Lencastre A, Fidalgo A, Lobo L, João A, Serrão V. Postradiation cutaneous angiosarcoma of the breast: a diagnosis to keep in mind. Breast J. 2014;20:89-90. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 13] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 20. | Moe M, Bertelli G. Breast angiosarcoma following lumpectomy and radiotherapy for breast cancer: a case with short latent period and false negative result on biopsies. Ann Oncol. 2007;18:801. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 21. | Chikarmane SA, Gombos EC, Jagadeesan J, Raut C, Jagannathan JP. MRI findings of radiation-associated angiosarcoma of the breast (RAS). J Magn Reson Imaging. 2015;42:763-770. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 34] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 22. | Sanders LM, Groves AC, Schaefer S. Cutaneous angiosarcoma of the breast on MRI. AJR Am J Roentgenol. 2006;187:W143-W146. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 21] [Article Influence: 1.1] [Reference Citation Analysis (0)] |