Published online May 6, 2024. doi: 10.12998/wjcc.v12.i13.2151
Peer-review started: December 29, 2023
First decision: February 9, 2024
Revised: February 15, 2024
Accepted: March 28, 2024
Article in press: March 28, 2024
Published online: May 6, 2024
Processing time: 118 Days and 8.1 Hours
Acetabular fractures in the geriatric population are typically low-energy fractures resulting from a fall from standing height. Compromised bone quality in the elderly, as well as this population’s concomitant medical comorbidities, render the management of such fractures challenging and controversial. Non-operative management remains the mainstay of treatment, although such a choice is associated with numerous and serious complications related to both the hip joint as well as the general condition of the patient. On the other hand, operatively treating acetabular fractures (e.g., with osteosynthesis or total hip arthroplasty) is gaining popularity. Osteosynthesis can be performed with open reduction and internal fixation or with minimally invasive techniques. Total hip arthroplasty could be performed either in the acute phase combined with osteosynthesis or as a delayed procedure after a period of non-operative management or after failed osteosynthesis of the acetabulum. Regardless of the implemented treatment, orthogeriatric co-management is considered extremely crucial, and it is currently one of the pillars of a successful outcome after an acetabular fracture.
Core Tip: Treatment of geriatric acetabular fractures is a challenging clinical problem that has recently gained significant attention within the orthopaedic community. Whilst non-operative management is a used treatment strategy, surgery in the form of either osteosynthesis or combination of osteosynthesis and acute total hip arthroplasty is currently extensively performed. The orthogeriatric co-management of the fragile patients who have sustained an acetabular fracture is essential and of paramount importance.
- Citation: Tosounidis T, Chalidis B. Management of geriatric acetabular fractures: Contemporary treatment strategies. World J Clin Cases 2024; 12(13): 2151-2156
- URL: https://www.wjgnet.com/2307-8960/full/v12/i13/2151.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i13.2151
The incidence of acetabular fractures in the elderly population has significantly increased over the last years[1]. There are substantial differences that make these fractures different from the ones occurring in the younger counterparts. First, they are low-energy fractures; second the configuration/type of the fracture is different with a significant prevalence of anteriorly based fractures; third, their management includes the option of hip arthroplasty, which is not the case in young patients; and last but not least the co-existing medical comorbidities constitute both the decision making and the overall management more challenging.
The degree of controversy surrounding the issue and the lack of validated management guidelines are vividly depicted in a recent survey that was conducted in 15 level-I Trauma Centers in the United States and included more than 250 patients over the age of 60 years [2]. The study showed that operative treatment was implemented in only 60% of the cases. Age less than 80 years, high-energy fractures, concomitant femoral head lesions, and hip incongruency were the main factors that were taken into consideration by the treating surgeons to decide on the operative management. The vast majority (90%) of the surgically treated patients were managed with open reduction and internal fixation (ORIF) whilst total hip arthroplasty (THA) was performed in the remainder of the cases. From the known risk factors associated with poor outcomes, only dome impaction was significantly associated with receiving surgery. The authors concluded that these results reflected the lack of clear guidelines for management. In general, the decision for surgical intervention is a multifactorial endeavor that takes into account the type of fracture, the physiology and the age of the patients, the expertise of the surgical team, and the logistics of the healthcare setup.
Mortality resulting from geriatric acetabular fractures is a matter that has been recently revisited by many scholars. There is a tendency in the contemporary literature to compare the mortality of acetabular fractures to that of hip fractures that occur in the same age cohorts. Khoshbin et al[3] from the University of Toronto in a matched cohort study that included patients older than 60 years, concluded that acetabular fractures had a much higher risk of early mortality compared to hip fractures. On the other hand, Stetzelberger et al[4] from Switzerland documented that whilst there was no difference in mortality between the acetabular and hip fracture patients at the first 30 postinjury days, the 1-year mortality was double for hip fracture patients (18% acetabular vs 36% hip fractures). Mortality has also been studied by comparing operative vs no-operative management. Firoozabadi et al[5] demonstrated that operative treatment had significantly lower mortality compared to conservative management whilst at the same time more than 80% of the deaths in the no-surgically treated patients occurred within one year from the injury. Gary et al[6] in a larger group of patients also indicated that the 1-year mortality was higher in non-operatively treated patients but when this was adjusted for comorbidities, gender, age, and mechanism of injury, no difference between them was observed. Another interesting parameter that has been recently added and investigated in the long catalog of factors that could potentially strongly affect and predict mortality after acetabular fractures is sarcopenia, which in simple words can be understood as age-related bone loss[7,8]. Considering the increased interest related to sarcopenia and orthopaedic trauma, it is to be expected that in the near future, there will be more studies shedding light on this issue.
Non-operative management used to be the standard of care for these injuries up to the recent past. In the contemporary era despite the fact the surgical management of these injuries is on the rise, there is still a role for the so-called “conservative management”[9]. This by no means should be interpreted as complete bed rest. The latter is fraud with devastating and potentially fatal complications namely pulmonary and/or urinary infections, thromboembolic disease, and recumbency ulcers. Non-operative management should include early mobilization of the patient out of bed, musculoskeletal conditioning, and respiratory physiotherapy. Taking this into consideration, long periods of skeletal traction have no place in the modern management of acetabular fractures in the elderly. Traction should only be applied with caution and only for a few days (maximum 7-10 d). Early and safe mobilization of the patients is a priority and every effort should be made in that direction.
The outcomes of non-operative management have not extensively been studied in the current era. They remain contradictive, with Ryan et al[10] reporting good outcomes at a 2-year follow-up in a cohort of 27 patients that were treated non-operatively even though the patients met at least one of the surgical indications. On the contrary, Baker et al[11] studied 49 patients with associated fracture types and reported significantly reduced mobility and living independence at 1-year follow-up.
Osteosynthesis of acetabular fractures in the elderly is challenging and frequently yields suboptimal results[12]. Several criteria should be considered when a surgeon is choosing osteosynthesis as the mode of surgical management. Chronological age should not be taken into account in isolation. No clear cut-off is used in the contemporary literature to discriminate between elderly vs younger patients. Nevertheless, most of the studies use the age of 60 years as the cut-off point.
Biological age is a more appropriate parameter to be considered. Consequently, the physical condition as well as the comorbidities should be considered when a decision for osteosynthesis is made.
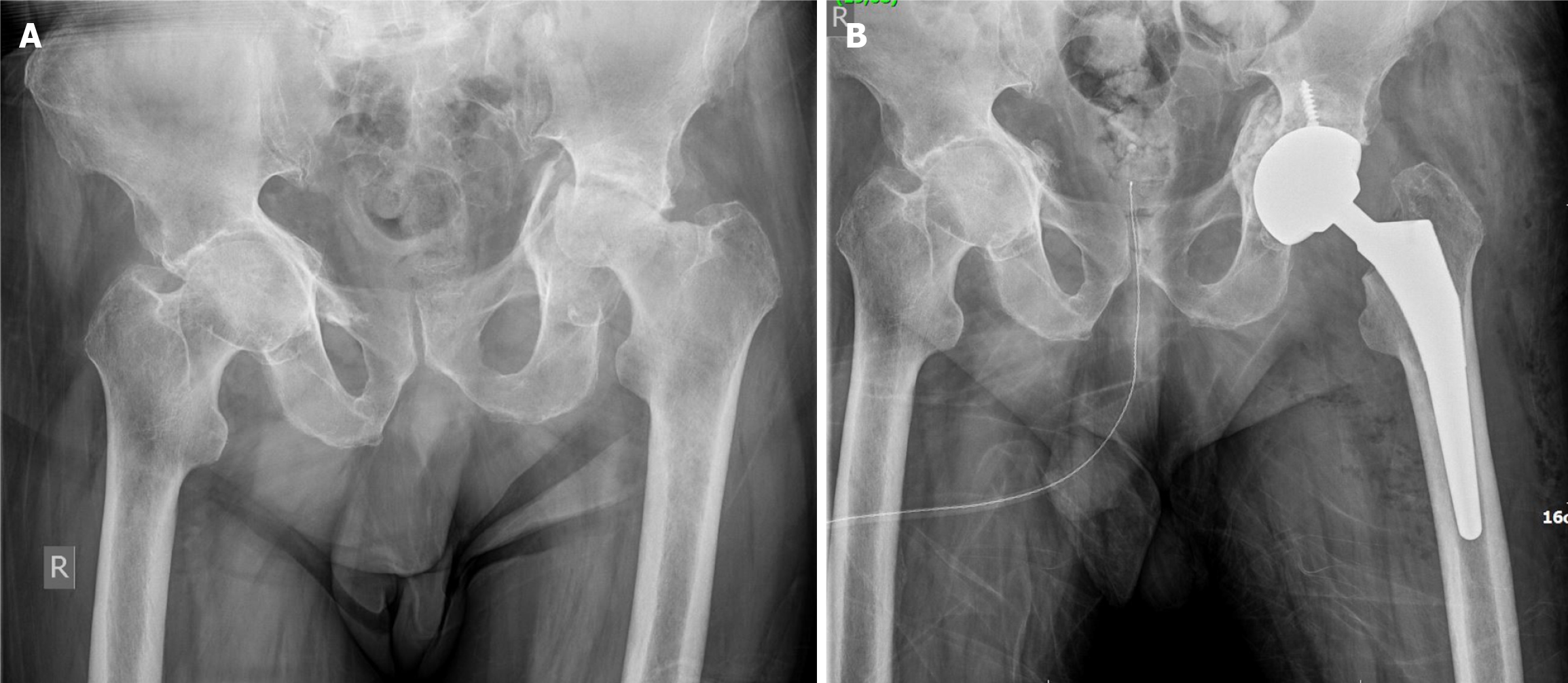
The type of fractures encountered in the elderly are more frequently anterior-based[9] and have a concomitant anteromedial dome impaction[13,14] (Figure 1). This configuration of fracture along with the associated osteopenia make the osteosynthesis quite cumbersome and prone to secondary failure even if intra-operatively a good result has been achieved. In recent days the anterior intrapelvic approach[15] is most frequently used when addressing anterior-based fractures through a typical ORIF technique. Additionally, the pararectus approach introduced by the Bernese group[16], is an option that offers direct access to the superior and anteromedial dome of the acetabulum and is more atraumatic to the soft tissues compared to other surgical approaches. Although optimal outcomes have been documented with its application, the pararectus approach is not widely used and worldwide, the Anteriorly Intrapelvic Approach is still the most commonly used approach to surgically treat anteriorly based acetabular fractures.
At this juncture, it should be emphasized that perfect anatomic reduction of acetabular fractures is not always feasible in elderly patients and oftentimes the surgeon should accept a less perfect reduction keeping in mind that especially in octogenarians, early and pain-free mobilization is the goal of management.
In a recent systematic review, Capone et al[17] found that the conversion to a THA after an ORIF was performed at a mean of 25.5 months. Anatomical reduction was achieved in 11.6% of cases and imperfect and poor reduction in 22.3%. In the same study, ORIF was associated with longer operative time, more blood loss, higher secondary surgery rate, and higher 1-year mortality when compared to a THA performed in the acute setting. On the contrary, in another systematic review, Daurka et al[18] demonstrated better functional outcomes in the patients treated with ORIF compared to those with THA.
Minimally invasive percutaneous osteosynthesis is advocated by some surgeons to stabilize only the columnar elements of a fracture. Minimal invasion fracture osteosynthesis with closed reduction and percutaneous fixation is an attractive option for acetabular fracture fixation as it may be associated with less blood loss, shorter operative time, and decreased risk for infection, particularly in geriatric populations with low cardiac reserve[10]. The technique has gained popularity not only in simple fractures of the anterior or posterior column but also in displaced fractures that can be reduced with traction, manipulation, and percutaneous leverage under fluoroscopy and can be subsequently fixed with screws[19]. Percutaneous fracture fixation of pelvis and acetabulum is a technically demanding procedure that requires a high level of surgical skills and expertise to perform accurately and safely. Despite the clear advantages of stabilizing the fracture by closed means, the long-term functional outcome and the incidence of conversion to THA are similar[10] or even higher[20] when compared to open fixation techniques.
THA should be considered for the elderly in a threefold perspective: (1) Acute THA along with ORIF; (2) Delayed THA after non-operative management; and (3) THA after failed ORIF of the acetabulum.
The combination of ORIF and acute THA is a complex surgical procedure that requires a mixed and advanced skillset from the orthopaedic surgeon[21,22]. The purpose of the ORIF in this clinical scenario is to restore the anatomy of the columns and thus create a stable bed for the subsequent implantation of the acetabular cup. The ORIF should be applied in a timely and efficient manner to minimize the surgical time, the blood loss, and the physiological stress of the patient. The ORIF can be performed utilizing an anterior-based approach (anterior intrapelvic or pararectus) and then followed by a THA using the posterior approach. Another option is to perform a posterior approach to perform both the ORIF and the THA. A third alternative is to perform a Smith-Petersen-type approach followed by an anteriorly performed THA. The choice depends on the type of fracture and the skillset of the surgeon. In regards to the implant selection for the THA, an uncemented cup is preferred. The option of a big multi-hole cup size should be strongly considered. Trabecular metal offers great initial stabilization of the cup and is an option preferred by many surgeons. Dual mobility articulation should also be considered based on the same rationale that dictates its use during THA after a femoral neck fracture. Acetabular cages must be considered when needed. The critical point of the surgical technique is that the surgeon should be prepared to perform a complex primary THA having implants that are usually used in the revision THA setting.
In recent years, acute THA has yielded optimal clinical outcomes. In a recent systematic review that included 642 patients from 10 observational studies, comparing ORIF vs limited ORIF combined with THA, Tu et al[23] noticed that acute THA was associated with higher hip Harris score (HHS), improved physical function and better SF-36 physical component summary and mental component summary scores after 1-year postoperatively. Moreover, lesser complication and reoperation rates, and greater bodily pain were also recorded. According to a meta-analysis from Jauregui et al[24], acute THA provided a good functional outcome (HSS: 83) and was associated with a revision rate of 4.3% and a complication rate of 20%.
THA after a non-operative acetabular fracture can be either relatively straightforward or very technically demanding[25,26] (Figure 2). If the initial and subsequent displacement is minimal then the technical difficulties are not usually of great extent. On the other hand, if the displacement is significant the distorted anatomy can be very problematic and should be addressed accordingly. The same facts stand true for a delayed THA after ORIF. Although the literature is very scant upon this subject, it suggests that the outcomes are generally inferior to those observed after primary THA.
The proper and optimal management of acetabular fractures in the elderly also encompasses the collaboration of different medical specialties and the application of specific individualized protocols based on patients’ physical and mental status[19]. Orthogeriatric involvement and co-management is a well-established concept and is currently the standard of care for hip fractures worldwide[27,28]. Although fracture liaison service efficiency has not been studied in this subgroup of elderly patients it is logical to assume that this approach should be also implemented in elderly patients with acetabular fractures[29]. Further involvement of anesthesiologists and nurses can additionally decrease the mortality rates and improve the treatment efficacy[20]. Older patients should be acknowledged as a special cohort with diminished phy
In summary, the contemporary literature is devoid of robust evidence to guide the most appropriate management of acetabular fractures in the elderly. There is currently a wide variation of management practices even amongst high-volume, experienced surgeons. The decision should be guided by the physiologic age and the comorbidities of the patient, the fracture configuration as well as the expertise and experience of the surgeon. Non-operative management is appropriate for particular patients, but prolonged bed rest should be avoided. Osteosynthesis is associated with good outcomes in selected patients but there is currently a trend toward a same-setting ORIF in combination with THA. Orthogeriatric co-management is essential and of paramount importance to achieve an overall optimal outcome in the fragile group of elderly patients who have sustained an acetabular fracture.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: Greece
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Ueda H, Japan S-Editor: Che XX L-Editor: A P-Editor: Zhao S
| 1. | Fritz A, Gericke L, Höch A, Josten C, Osterhoff G. Time-to-treatment is a risk factor for the development of pressure ulcers in elderly patients with fractures of the pelvis and acetabulum. Injury. 2020;51:352-356. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 2.2] [Reference Citation Analysis (80)] |
| 2. | Manson TT, Reider L, OʼToole RV, Scharfstein DO, Tornetta P 3rd, Gary JL; Major Extremity Trauma Research Consortium (METRC). Variation in Treatment of Displaced Geriatric Acetabular Fractures Among 15 Level-I Trauma Centers. J Orthop Trauma. 2016;30:457-462. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 28] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 3. | Khoshbin A, Atrey A, Chaudhry H, Nowak L, Melo LT, Stavrakis A, Schemitsch EH, Nauth A. Mortality Rate of Geriatric Acetabular Fractures Is High Compared With Hip Fractures. A Matched Cohort Study. J Orthop Trauma. 2020;34:424-428. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 21] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 4. | Stetzelberger VM, Brouze IF, Steppacher SD, Bastian JD, Schwab JM, Tannast M. Lower 1-Year Postoperative Mortality After Acetabular Versus Proximal Femoral Fractures in Elderly Patients. J Bone Joint Surg Am. 2021;103:1807-1816. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 7] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 5. | Firoozabadi R, Cross WW, Krieg JC, Routt MLC. Acetabular Fractures in the Senior Population- Epidemiology, Mortality and Treatments. Arch Bone Jt Surg. 2017;5:96-102. [PubMed] |
| 6. | Gary JL, Paryavi E, Gibbons SD, Weaver MJ, Morgan JH, Ryan SP, Starr AJ, OʼToole RV. Effect of surgical treatment on mortality after acetabular fracture in the elderly: a multicenter study of 454 patients. J Orthop Trauma. 2015;29:202-208. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 59] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 7. | Deren ME, Babu J, Cohen EM, Machan J, Born CT, Hayda R. Increased Mortality in Elderly Patients with Sarcopenia and Acetabular Fractures. J Bone Joint Surg Am. 2017;99:200-206. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 66] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 8. | Mitchell PM, Collinge CA, OʼNeill DE, Bible JE, Mir HR. Sarcopenia Is Predictive of 1-Year Mortality After Acetabular Fractures in Elderly Patients. J Orthop Trauma. 2018;32:278-282. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 38] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 9. | Albrektsson M, Möller M, Wolf O, Wennergren D, Sundfeldt M. Acetabular fractures: Epidemiology and mortality based on 2,132 fractures from the Swedish Fracture Register. Bone Jt Open. 2023;4:652-658. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 14] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 10. | Ryan SP, Manson TT, Sciadini MF, Nascone JW, LeBrun CT, Castillo RC, Muppavarapu R, Schurko B, OʼToole RV. Functional Outcomes of Elderly Patients With Nonoperatively Treated Acetabular Fractures That Meet Operative Criteria. J Orthop Trauma. 2017;31:644-649. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 34] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 11. | Baker G, McMahon SE, Warnock M, Johnston A, Cusick LA. Outcomes of conservatively managed complex acetabular fractures in the frail and elderly one year post injury. Injury. 2020;51:347-351. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 19] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 12. | Tosounidis TH, Giannoudis PV. What is new in acetabular fracture fixation? Injury. 2015;46:2089-2092. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 12] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 13. | Manson T, Schmidt AH. Acetabular Fractures in the Elderly: A Critical Analysis Review. JBJS Rev. 2016;4. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 21] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 14. | Tosounidis TH, Stengel D, Giannoudis PV. Anteromedial dome impaction in acetabular fractures: Issues and controversies. Injury. 2016;47:1605-1607. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 7] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 15. | Sagi HC, Afsari A, Dziadosz D. The anterior intra-pelvic (modified rives-stoppa) approach for fixation of acetabular fractures. J Orthop Trauma. 2010;24:263-270. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 146] [Cited by in RCA: 164] [Article Influence: 10.9] [Reference Citation Analysis (0)] |
| 16. | Keel MJB, Siebenrock KA, Tannast M, Bastian JD. The Pararectus Approach: A New Concept. JBJS Essent Surg Tech. 2018;8:e21. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 23] [Cited by in RCA: 42] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 17. | Capone A, Peri M, Mastio M. Surgical treatment of acetabular fractures in the elderly: a systematic review of the results. EFORT Open Rev. 2017;2:97-103. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 25] [Cited by in RCA: 37] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 18. | Daurka JS, Pastides PS, Lewis A, Rickman M, Bircher MD. Acetabular fractures in patients aged > 55 years: a systematic review of the literature. Bone Joint J. 2014;96-B:157-163. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 147] [Cited by in RCA: 130] [Article Influence: 11.8] [Reference Citation Analysis (0)] |
| 19. | Antell NB, Switzer JA, Schmidt AH. Management of Acetabular Fractures in the Elderly. J Am Acad Orthop Surg. 2017;25:577-585. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 43] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 20. | McCormick BP, Serino J, Orman S, Webb AR, Wang DX, Mohamadi A, Mortensen S, Weaver MJ, Von Keudell A. Treatment modalities and outcomes following acetabular fractures in the elderly: a systematic review. Eur J Orthop Surg Traumatol. 2022;32:649-659. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 23] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 21. | Manson TT. Open Reduction and Internal Fixation Plus Total Hip Arthroplasty for the Acute Treatment of Older Patients with Acetabular Fracture: Surgical Techniques. Orthop Clin North Am. 2020;51:13-26. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 15] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 22. | Giustra F, Cacciola G, Pirato F, Bosco F, De Martino I, Sabatini L, Rovere G, Camarda L, Massè A. Indications, complications, and clinical outcomes of fixation and acute total hip arthroplasty for the treatment of acetabular fractures: A systematic review. Eur J Orthop Surg Traumatol. 2024;34:47-57. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Reference Citation Analysis (0)] |
| 23. | Tu TY, Chen CY, Lin PC, Hsu CY, Lin KC. Comparison of primary total hip arthroplasty with limited open reduction and internal fixation vs open reduction and internal fixation for geriatric acetabular fractures: a systematic review and meta-analysis. EFORT Open Rev. 2023;8:532-547. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 24. | Jauregui JJ, Weir TB, Chen JF, Johnson AJ, Sardesai NR, Maheshwari AV, Manson TT. Acute total hip arthroplasty for older patients with acetabular fractures: A meta-analysis. J Clin Orthop Trauma. 2020;11:976-982. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 32] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 25. | Sermon A, Broos P, Vanderschot P. Total hip replacement for acetabular fractures. Results in 121 patients operated between 1983 and 2003. Injury. 2008;39:914-921. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 77] [Cited by in RCA: 81] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 26. | Nicol GM, Sanders EB, Kim PR, Beaulé PE, Gofton WT, Grammatopoulos G. Outcomes of Total Hip Arthroplasty After Acetabular Open Reduction and Internal Fixation in the Elderly-Acute vs Delayed Total Hip Arthroplasty. J Arthroplasty. 2021;36:605-611. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 35] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 27. | De Vincentis A, Behr AU, Bellelli G, Bravi M, Castaldo A, Galluzzo L, Iolascon G, Maggi S, Martini E, Momoli A, Onder G, Paoletta M, Pietrogrande L, Roselli M, Ruggeri M, Ruggiero C, Santacaterina F, Tritapepe L, Zurlo A, Antonelli Incalzi R; Società Italiana Geriatria e Gerontologia (SIGG); Associazione Italiana di Psicogeriatria (AIP); Società Italiana di Geriatria Ospedale e Territorio (SIGOT); Società Italiana di Medicina Generale (SIMG); Società Italiana di Anestesia Analgesia Rianimazione e Terapia Intensiva (SIAARTI); Società Italiana di Ortopedia e Traumatologia (SIOT); Fragility Fracture Network-Italia (FFN-I); Società Italiana di Medicina Fisica e Riabilitativa (SIMFER); Società Italiana di Fisioterapia (SIF); Consiglio Nazionale delle Ricerche (CNR); Associazione Italiana di Fisioterapia (AIFI); Istituto Superiore Sanità (ISS). Orthogeriatric co-management for the care of older subjects with hip fracture: recommendations from an Italian intersociety consensus. Aging Clin Exp Res. 2021;33:2405-2443. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 19] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 28. | Fluck B, Yeong K, Lisk R, Watters H, Robin J, Fluck D, Fry CH, Han TS. Changes in Characteristics and Outcomes of Patients Undergoing Surgery for Hip Fractures Following the Initiation of Orthogeriatric Service: Temporal Trend Analysis. Calcif Tissue Int. 2022;110:185-195. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 8] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 29. | Javaid MK, Sami A, Lems W, Mitchell P, Thomas T, Singer A, Speerin R, Fujita M, Pierroz DD, Akesson K, Halbout P, Ferrari S, Cooper C. A patient-level key performance indicator set to measure the effectiveness of fracture liaison services and guide quality improvement: a position paper of the IOF Capture the Fracture Working Group, National Osteoporosis Foundation and Fragility Fracture Network. Osteoporos Int. 2020;31:1193-1204. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 59] [Cited by in RCA: 70] [Article Influence: 14.0] [Reference Citation Analysis (0)] |
| 30. | Bradburn E, Rogers FB, Krasne M, Rogers A, Horst MA, Beelen MJ, Miller JA. High-risk geriatric protocol: improving mortality in the elderly. J Trauma Acute Care Surg. 2012;73:435-440. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 68] [Article Influence: 5.2] [Reference Citation Analysis (0)] |