Published online Apr 26, 2024. doi: 10.12998/wjcc.v12.i12.2122
Peer-review started: January 4, 2024
First decision: February 23, 2024
Revised: March 4, 2024
Accepted: March 22, 2024
Article in press: March 22, 2024
Published online: April 26, 2024
Processing time: 101 Days and 20 Hours
Crossed renal ectopia (CRE) occurs when one kidney crosses the midline from the primary side to the contralateral side while the ureter remains on the primary side. Rectal cancer, one of the most common malignant tumors of the digestive tract, refers to cancer from the dentate line to the rectosigmoid junction. The concurrent presentation of CRE alongside rectal cancer is an uncommon clinical observation.
Herein, we report a 69-year-old male patient with rectal cancer who was diagnosed with CRE via computed tomography during hospitalization. Following thorough preoperative evaluations, the patient underwent Dixon surgery.
We performed laparoscopic radical resection of rectal cancer and adequate lymph node removal in a patient with CRE with no postoperative discomfort.
Core Tip: Rectal cancer is a common malignant tumor in clinical practice, and current treatment methods mainly include surgery and chemotherapy. The occurrence of rectal cancer in conjunction with crossed renal ectopia (CRE) is exceedingly rare. We reported a patient with rectal cancer who underwent CRE and Dixon surgery.
- Citation: Tang ZW, Yang HF, Wu ZY, Wang CY. Crossed renal ectopia with rectal cancer: A case report. World J Clin Cases 2024; 12(12): 2122-2127
- URL: https://www.wjgnet.com/2307-8960/full/v12/i12/2122.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i12.2122
Crossed renal ectopia (CRE) involves the translocation of one kidney from its original side across the midline to the contralateral side. Contrary to what the term might suggest, the kidneys do not actually "cross" each other; instead, one kidney shifts to the same side as the other. Any colon surgery for such patients must take into account possible anatomical abnormalities, such as abnormalities in the renal vessels and variations in the position of the ureter. For patients with CRE, in addition to ensuring an adequate resection margin of the tumor, attention should be given to the protection of blood vessels and nerves in the surrounding organs, and appropriate enlarged combined resection may be performed when necessary. Consequently, conducting a thorough preoperative assessment and formulating a meticulous surgical strategy are of paramount importance. In Japan, Nakai et al[1] reported the laparoscopic treatment of a patient with CRE complicated with sigmoid carcinoma; however, instances of combined laparoscopic treatment for CRE complicated by rectal cancer have yet to be documented.
In this paper, we report a case of CRE with rectal cancer treated by laparoscopic surgery without any postoperative complications.
A one-month history of frequent bowel movements and the passage of dark red bloody stools, with no apparent cause.
A 69-year-old male experienced an increase in the frequency of defecation-approximately 2-3 times/d-mainly due to no obvious cause before 1 month-dark red stool with blood.
The patient had lost 10 pounds in weight in the past five months.
The patient denied any family history of malignant tumors.
On physical examination, the vital signs were as follows: body temperature, 36.5 °C; blood pressure, 135/78 mmHg; heart rate, 74 beats per minute; and breathing, 15 breaths per minute. The abdomen was soft, no mass was palpated, and no obvious abnormalities were found on anal examination.
Routine laboratory tests showed no abnormal values, and evaluation of tumor markers revealed a high level of carcinoembryonic antigen of 10.1 ng/mL (standard value 0-3.4 ng/mL) and no other significant abnormalities.
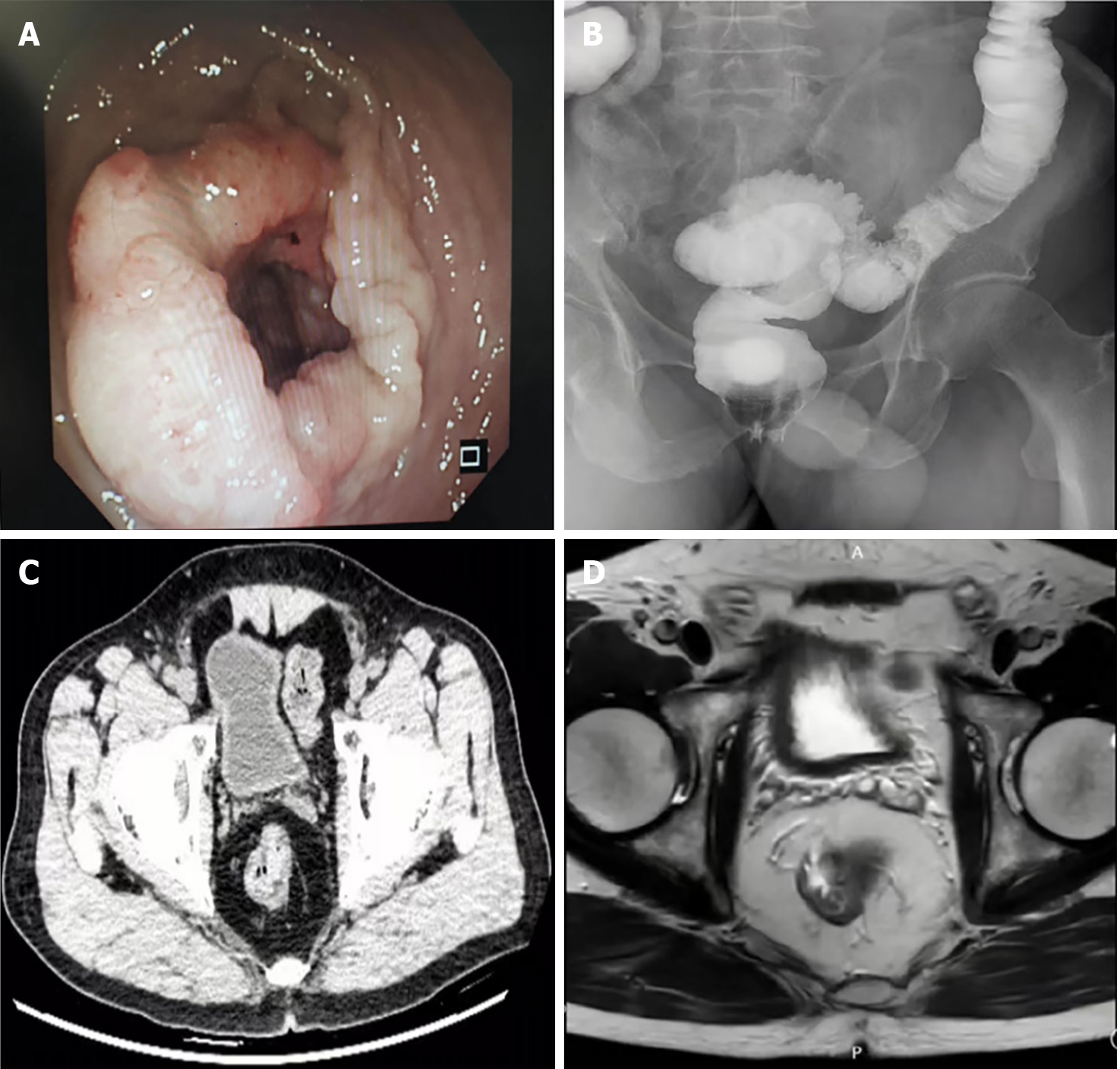
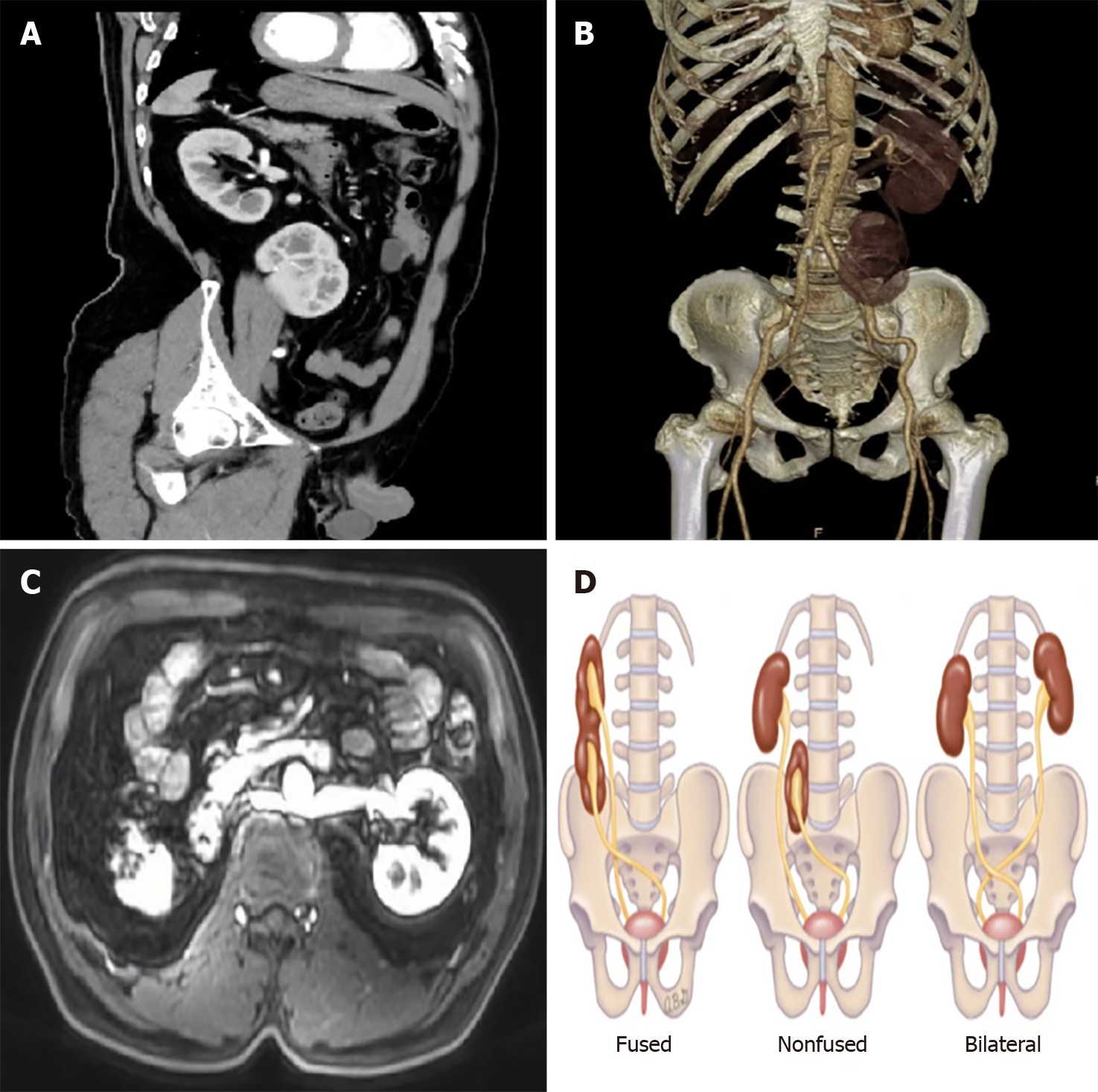
Colonoscopy revealed a peripheral mass approximately 12 cm away from the anal margin (Figure 1A); gastrointestinal angiography revealed space-occupying lesions in the rectum (Figure 1B); colonoscopy revealed moderately differentiated adenocarcinoma. Contrast-enhanced computed tomography (CT) and magnetic resonance imaging (MRI) of the rectum suggested local thickening of the rectum and neoplastic lesions in the middle and upper parts of the rectum, which was considered rectal cancer (T3) (Figure 1C and D). Multiple nodules were observed in the mesorectum, presacral fascia, and bilateral iliac vessels and were considered metastatic lymph nodes (N+), but contrast-enhanced CT also revealed no renal shadow in the right kidney area; additionally, no renal shadow was found in the left lower abdomen or pelvis, and the shape of the kidney was irregular (Figure 2A and B). Subsequently, we performed enhanced MRI of the abdomen and pelvis of the patient, first, to rule out the possibility of liver metastasis that could not be detected by CT, and second, to take a closer look at blood vessels. There was no renal shadow in the right kidney area, and a shadow in the left abdominal or pelvic kidney was considered. A CRE with malrotation and an abnormal internal signal was considered. The left renal vein ran behind the abdominal aorta, suggesting posterior nutcracker syndrome (Figure 2C).
The patient was diagnosed with rectal cancer (cT3N + M0) combined with CRE and underwent laparoscopic radical resection of rectal cancer combined with D3 Lymph node dissection. During Toldt's space separation, a blood vessel very similar to the inferior mesenteric artery (IMA) was found. At the time, given the patient's anatomical variations, the surgeon opted not to dissect the blood vessel. Instead, the separation was conducted laterally and anteriorly to Gerota's fascia, proceeding from the exterior towards the interior, and the posterior kidney and ureter were protected during the operation. With internal and lateral penetration, we found that the blood vessels that were not severed at the beginning were the veins of the ectopic kidney. Then, we safely severed the IMA, protected the hypogastric nerves on both sides, ensured a sufficient tumor resection margin, severed the intestinal tube, and sent specimens for pathology. The remaining descending colon and rectum were moved toward the pelvis, and the descending colon and remaining rectum were anastomosed end to end. The operation time was 190 min, and the blood loss volume was 20 mL. Postoperative pathological findings revealed that the tumor was a moderately differentiated rectal ulcerative adenocarcinoma with a size of 5 cm × 3.5 cm × 1.5 cm. The tumor penetrated deep myometria and reached the peri-intestinal fat (pT3), nerve invasion and vascular cancer thrombus were visible, and no lymph node metastasis (pN0) was observed around it, corresponding to stage pIIA. The immunohistochemical results were as follows: MLH1 (+), MSH2 (+), MSH6 (+), PMS2 (+); the Ki-67 index was 80%.
Based on the patient's medical history, the final diagnosis was rectal cancer with CRE.
The patient was discharged from the hospital on the 7th day after surgery. Considering the risk factors associated with neuroaggression, the patient was advised to receive XELOX chemotherapy after surgery.
Currently, the follow-up patients are still alive.
CRE is a rare congenital genitourinary malformation. Its reported incidence is approximately 1 in 2000 individuals, with most cases being identified at autopsy[2]. There is a male-to-female ratio of approximately 3:2[3] and CRE can be classified into fusion type, nonfusion type and bilateral type. The nonconfluent type refers to an ectopic kidney that crosses the midline but does not integrate with the normal kidney parenchyma. The ureter of the ectopic kidney descends and crosses the midline, but the ureter drains into the bladder in a normal position. In the fused type, the ectopic kidney is usually fused below the normal kidney. Approximately 90% of these lesions are fused, which is commonly observed in the left kidney to the right ectopic fusion[4]. In the bilateral type, both kidneys are ectopic and cross the midline with the ureter to maintain normal bladder insertion (Figure 2D). This patient rarely had a right kidney to the left that was not fused, and some CREs can be accompanied by renal tumors, which are more common in adults. Clear cell carcinoma is the most common histological type and is rare in children, with the main type being Wilms tumor[5].
CRE is usually found incidentally during the investigation of other genitourinary problems, and approximately half of the patients experience other complications, such as kidney stones, hydronephrosis, and frequent urinary tract infections, for which surgical treatment may be the best choice[6]. Fortunately, none of the above symptoms were present in this patient.
Therefore, for patients with CRE, anatomical variation increases the risk and difficulty of colon surgery. The most important difference between the IMA and both kidneys is the difference in treatment because, for rectal surgery, 253 lymph nodes located at the root of the IMA sometimes need to be dissected to ensure the quality of D3 Lymph node dissection in rectal cancer patients. Therefore, the anatomical relationship between them must be clarified[6]. Maeda et al[7] reported a patient with a horseshoe kidney with sigmoid colon cancer who benefited from preoperative three dimensional (3D) angiography. Because a horseshoe kidney is usually accompanied by abnormalities in blood vessels or the ureter, angiography helps determine the location of these structures. Giani et al[8] performed anterior rectal resection surgery on patients with cross-fusion ectopic kidneys using 3D laparoscopy, and 3D laparoscopy technology also provided assurance of surgical safety. In our patient, the location of the IMA during the operation was unclear. For safety, the lateral approach was decisively changed to ensure that there was no wrong vessel. If necessary, open surgery may be considered to ensure a safe radical operation.
During intestinal surgery on patients with CRE, it is imperative to exercise caution to prevent injury to the ectopic kidney, ureter, renal vessels, genital vessels, and other structures located behind the peritoneum. Typically, the appropriate anatomical space for intervention is Toldt's space anterior to Gerota's fascia. If the dissection is too deep, there is a risk of damaging retroperitoneal structures, whereas if it is too superficial, it may result in tumor leakage. Additionally, special attention should be paid to safeguarding the bilateral hypogastric nerves adjacent to the bilateral common iliac vessels to minimize the impact on urinary and reproductive functions.
We recommend that patients with CRE or other renal malformations undergo a comprehensive preoperative evaluation to formulate a detailed surgical plan, and relevant angiography should be performed if necessary before surgical treatment in accordance with the above principles.
We would like to thank other members of the Department of General Surgery, Affiliated Hospital of the North China University of Technology, for the constructive criticism.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Sato T, Japan S-Editor: Zheng XM L-Editor: A P-Editor: Yu HG
| 1. | Nakai N, Yamaguchi T, Kinugasa Y, Shiomi A, Tomioka H, Kagawa H, Yamakawa Y, Sato S. Laparoscopic sigmoid colectomy for a patient with sigmoid colon cancer and crossed-fused renal ectopia: a case report. Int Surg. 2015;100:423-427. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 2. | Ajayi S, Mamven M, Tabari A, Ojji D, Ibrahim A. Crossed fused renal ectopia presenting as recurrent lower abdominal pain and urinary tract infection. Afr J Med Med Sci. 2013;42:193-196. [PubMed] |
| 3. | Solanki S, Bhatnagar V, Gupta AK, Kumar R. Crossed fused renal ectopia: Challenges in diagnosis and management. J Indian Assoc Pediatr Surg. 2013;18:7-10. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 45] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 4. | Bhojwani N, Hartman JB, Ahmed M, Morgan R, Davidson JC. Management of ureteral obstruction in crossed fused renal ectopia: A case report. Can Urol Assoc J. 2014;8:E752-E754. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 5. | Cao Y, Zhang Y, Kang W, Suo N, Cui Z, Luo Y, Jin X. Crossed-fused renal ectopia with renal calculi: Two case reports and a review of the literature. Medicine (Baltimore). 2019;98:e18165. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 6. | Hashiguchi Y, Muro K, Saito Y, Ito Y, Ajioka Y, Hamaguchi T, Hasegawa K, Hotta K, Ishida H, Ishiguro M, Ishihara S, Kanemitsu Y, Kinugasa Y, Murofushi K, Nakajima TE, Oka S, Tanaka T, Taniguchi H, Tsuji A, Uehara K, Ueno H, Yamanaka T, Yamazaki K, Yoshida M, Yoshino T, Itabashi M, Sakamaki K, Sano K, Shimada Y, Tanaka S, Uetake H, Yamaguchi S, Yamaguchi N, Kobayashi H, Matsuda K, Kotake K, Sugihara K; Japanese Society for Cancer of the Colon and Rectum. Japanese Society for Cancer of the Colon and Rectum (JSCCR) guidelines 2019 for the treatment of colorectal cancer. Int J Clin Oncol. 2020;25:1-42. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1024] [Cited by in RCA: 1305] [Article Influence: 261.0] [Reference Citation Analysis (1)] |
| 7. | Maeda Y, Shinohara T, Nagatsu A, Futakawa N, Hamada T. Laparoscopic resection aided by preoperative 3-D CT angiography for rectosigmoid colon cancer associated with a horseshoe kidney: A case report. Asian J Endosc Surg. 2014;7:317-319. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 10] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 8. | Giani A, Garancini M, Delitala A, Riva L, Gianotti L, Giardini V. 3D-laparoscopic anterior rectal resection in a patient with crossed fused renal ectopia: the importance of 3D imaging. Minerva Chir. 2017;72:546-547. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |