Published online Apr 26, 2024. doi: 10.12998/wjcc.v12.i12.2109
Peer-review started: January 1, 2024
First decision: January 16, 2024
Revised: January 29, 2024
Accepted: March 19, 2024
Article in press: March 19, 2024
Published online: April 26, 2024
Processing time: 105 Days and 18.2 Hours
Lateral window approach for sinus floor lift is commonly used for vertical bone augmentation in cases when the residual bone height is less than 5 mm. However, managing cases becomes more challenging when a maxillary sinus pseudocyst is present or when there is insufficient bone width. In this case, we utilized the bone window prepared during the lateral window sinus lift as a shell for horizontal bone augmentation. This allowed for simultaneous horizontal and vertical bone augmentation immediately after the removal of the maxillary sinus pseudocyst.
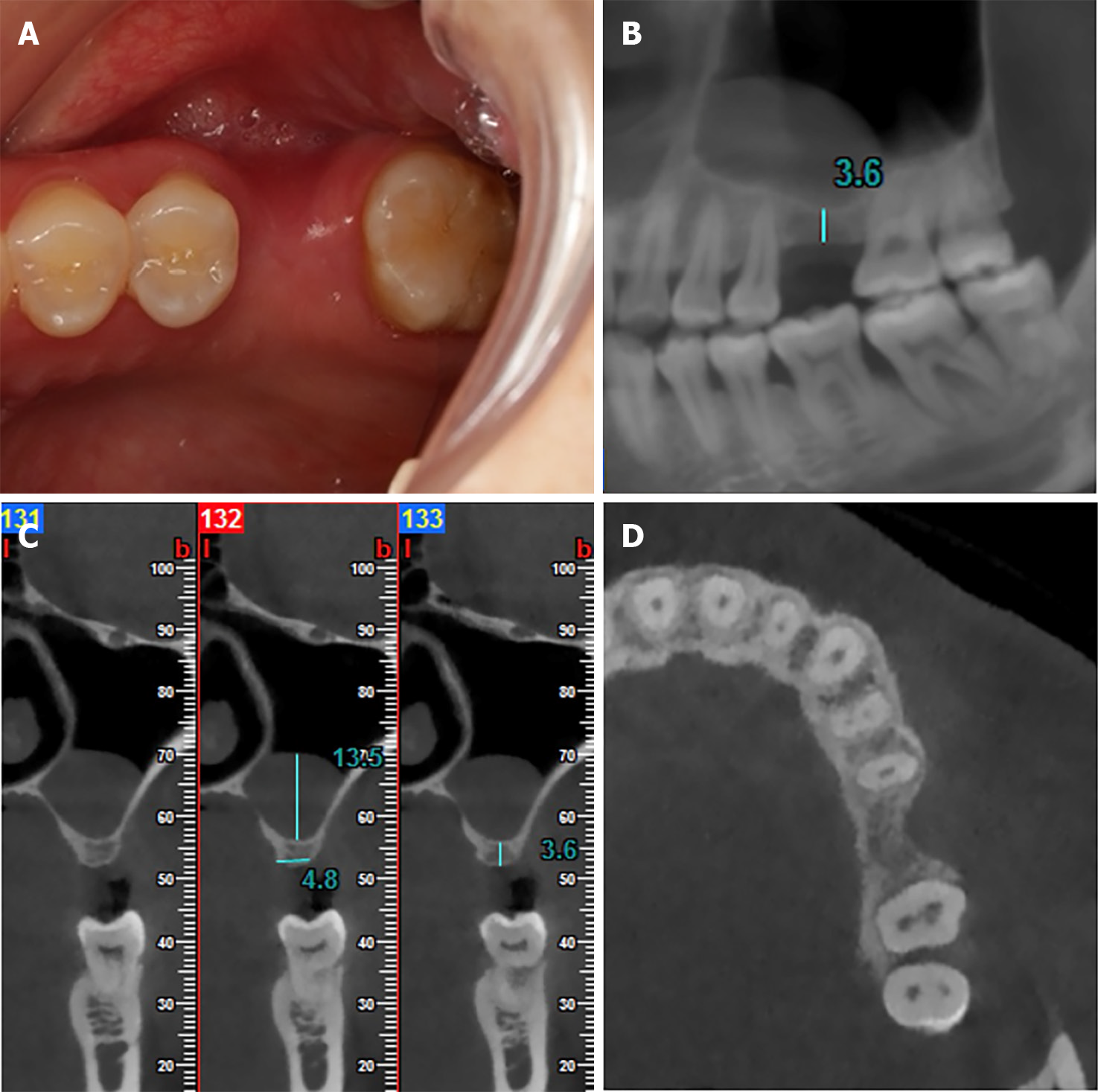
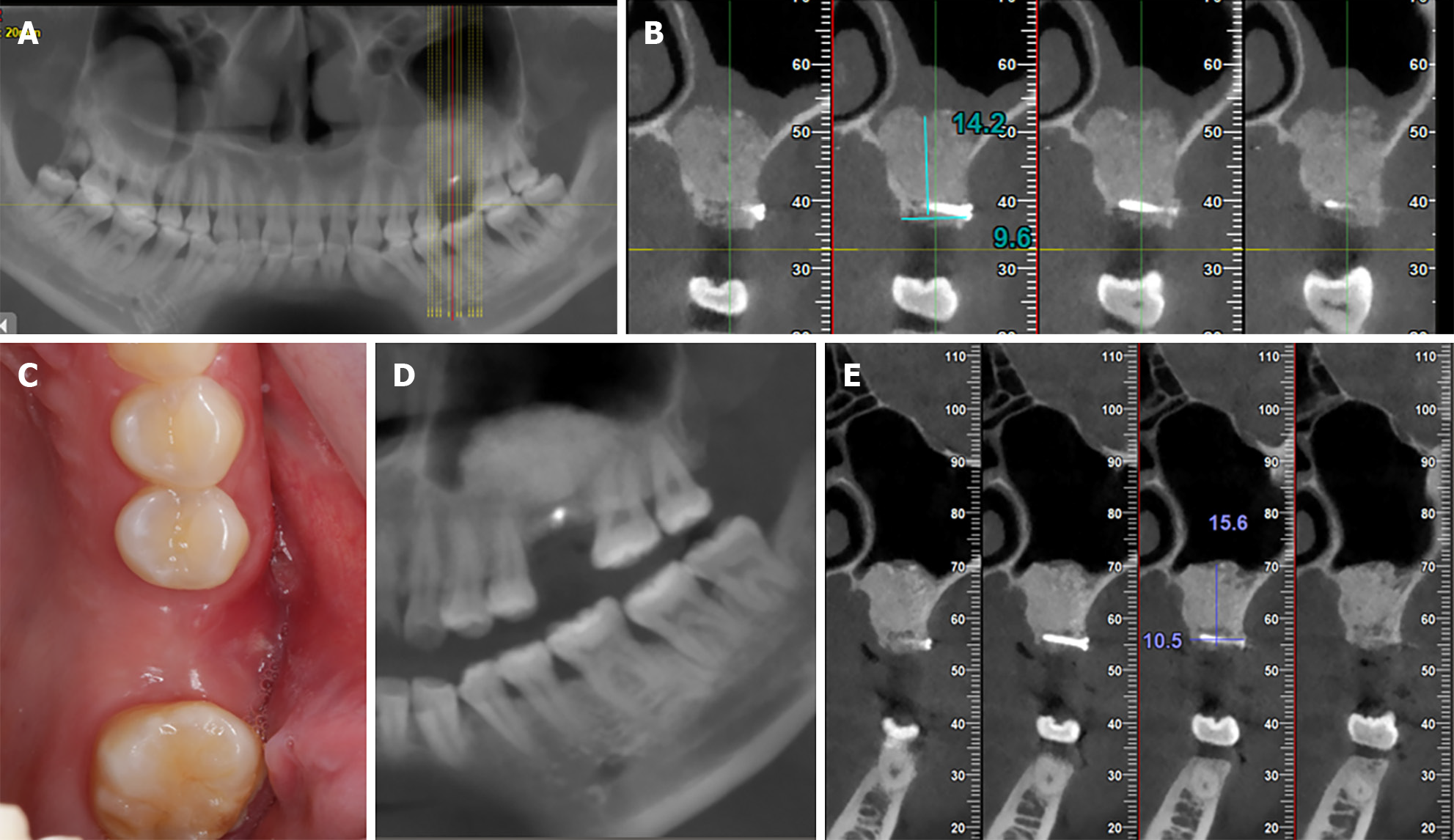
A 28-year-old female presented to our clinic with the chief complaint of missing upper left posterior teeth. Intraoral examination showed a horizontal deficiency of the alveolar ridge contour. The height of the alveolar bone was approximately 3.6 mm on cone beam computed tomography (CBCT). And a typical well-defined 'dome-shaped' lesion in maxillary sinus was observed on CBCT imaging. The lateral bony window was prepared using a piezo-ultrasonic device, then the bony window was fixed to the buccal side of the 26 alveolar ridge using a titanium screw with a length of 10 mm and a diameter of 1.5 mm. The space between the bony window and the alveolar ridge was filled with Bio-Oss, covered with a Bio-Gide collagen membrane, and subsequently sutured. Nine months later, the patient’s bone width increased from 4.8 to 10.5 mm, and the bone height increased from 3.6 to 15.6 mm. Subsequently, a Straumann® 4.1 mm × 10 mm implant was placed. The final all-ceramic crown restoration was completed four months later, and both clinical and radiographic examinations showed that the implant was successful, and the patient was satisfied with the results.
The bone block harvested from the lateral window sinus lift can be used for simultaneous horizontal bone augmentation acting as a shell for good two-dimensional bone augmentation.
Core Tip: The bone block harvested from the lateral window sinus lift as a shell for simultaneous horizontal bone augmentation can effectively address cases with insufficient bone height and width. This approach enables two-dimensional bone augmentation, leading to successful implant placement and restoration, as demonstrated in this case study.
- Citation: Wang YL, Shao WJ, Wang M. Bone block from lateral window - correcting vertical and horizontal bone deficiency in maxilla posterior site: A case report. World J Clin Cases 2024; 12(12): 2109-2115
- URL: https://www.wjgnet.com/2307-8960/full/v12/i12/2109.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i12.2109
In the edentulous maxillary posterior region, available bone heights (ABH) often decrease due to alveolar ridge resorption and progressive pneumatization of the maxillary sinus, presenting a challenge for implant restorations. The International Team for Implantology consensus recommends lateral window approach for sinus floor elevation when ABH is less than 5 mm in posterior maxilla[1].
The cortical bone tenting technique is an effective method for horizontal bone augmentation, involving the placement of a thin lamina of cortical bone over the particulate bone substitutes[2]. It is characterized by the thin cortical bone acting as a natural biological membrane, which is fixed to the alveolar ridge using titanium nails at a specific distance from the alveolar crest. Systemic review has shown that the cortical tenting technique can achieve a horizontal bone augmentation of 5.55 mm[3].
Although the maxillary sinus floor lift is a well-documented technique for bone regeneration, clinical decision-making for a maxillary sinus floor lift may become more complex when some lesions are present in the maxillary sinus[4,5]. The most commonly encountered condition during a maxillary sinus floor lift is maxillary sinus pseudocyst, with an incidence of approximately 1% to 24%[6,7]. Pseudocysts are usually detected on cone beam computed tomography (CBCT) and show a characteristic faint dome-shaped radiopacities[7]. The management of maxillary sinus cysts and the timing of bone grafting in maxillary sinus is controversial. Some scholars suggest that a period of healing is required after the removal of sinus cysts before bone grafting[8], while other scholars have achieved good results with contemporaneous bone grafting[9]. In some studies, dental implants have been placed at the same time with pseudocyst removal and bone grafting[10,11]. Some reviews have shown that the presence of pseudocysts does not affect the ultimate success of bone grafting and implant placement, but other studies have also suggested that detailed evaluation of patients is crucial to prevent undesirable complications[11,12].
This article presents a case using the bone block harvested from lateral window for sinus floor elevation/lift immediately after pseudocyst removal to correct severe vertical and horizontal bone deficiency in posterior maxilla.
A 28-year-old female patient consulted to Department of Oral Implantology with a complaint of a missing maxillary left upper molar several years ago due to tooth fracture.
The maxillary left upper first molar was extracted several years ago due to tooth fracture.
No significant medical history was reported. The patient denied any medical history and tobacco use.
No significant personal and family history was reported.
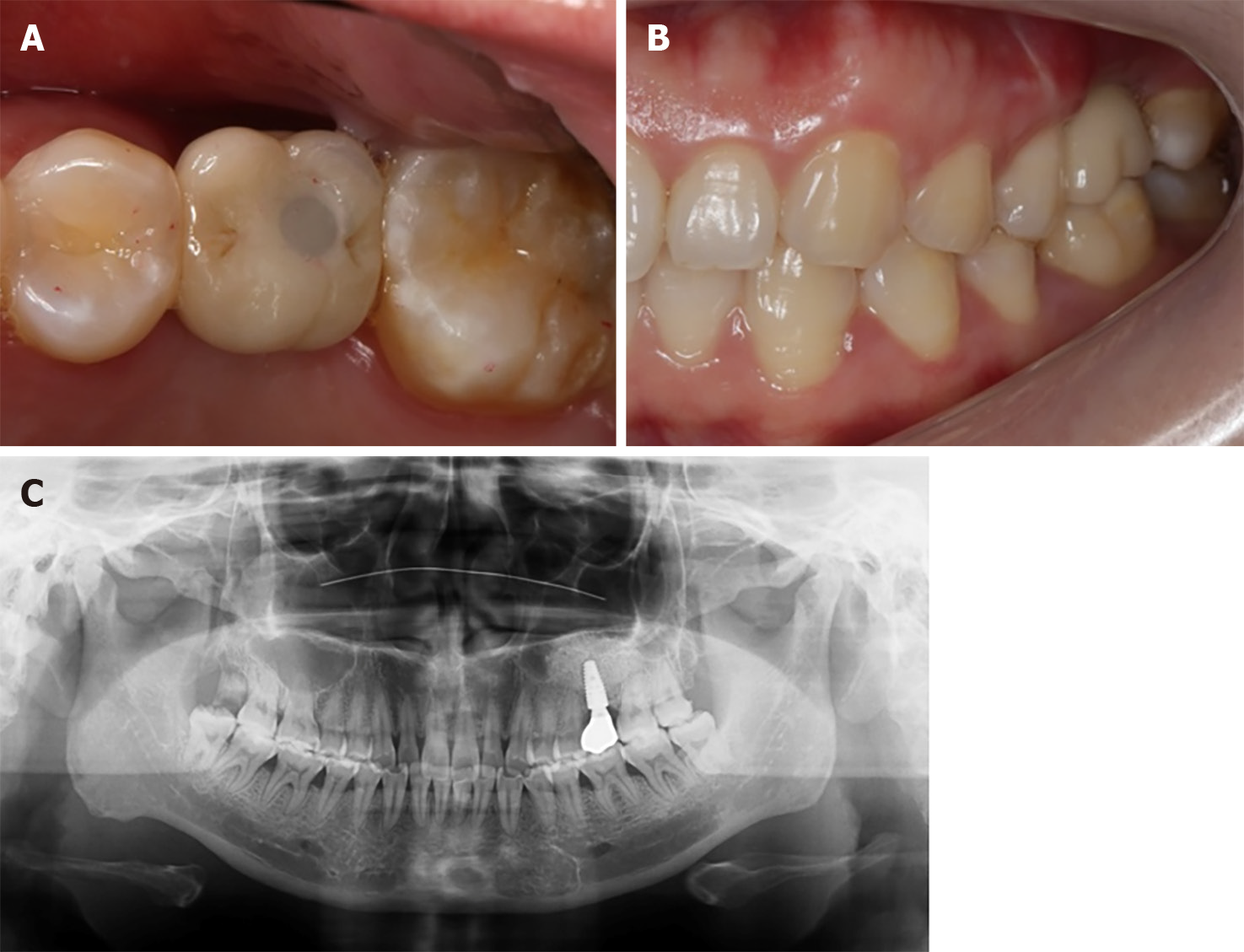
The patient’s blood pressure was 112/74 mmHg with a pulse rate of 72 beats per minutes. The buccal gingival contour of tooth 26 was collapsed from the occlusal view (Figure 1A).
The routine blood count and coagulation profile were within normal limits.
Maxillary dentition defect; sinus pseudocyst.
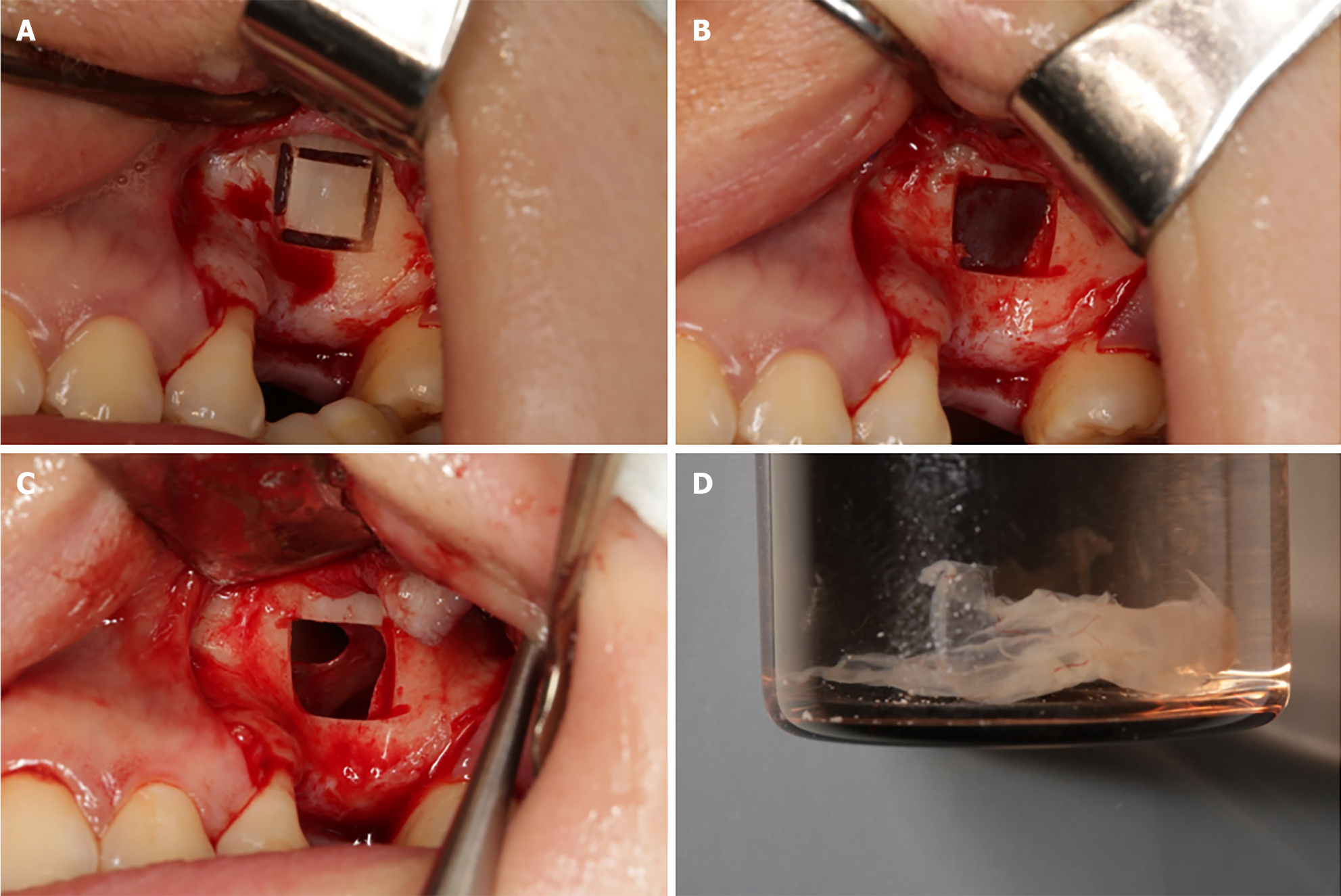
A staged approach for implant placement was planned following vertical and horizontal alveolar bone augmentation and pseudocyst removal. The informed consent for treatment was signed before surgery. Immediately prior to the surgery, the mouth was rinsed three times for three minutes using 0.12% chlorhexidine mouthwash. Adrenaline-containing articaine (4% articaine 1:100000 adrenaline, 3M Espe, Seefeld, Germany) was administered for local anesthesia. A midcrestal horizontal incision and two adjacent buccal releasing incisions were made, and the full-thickness mucoperiosteal flap was reflected to expose the alveolar bone and the lateral wall of maxillary sinus. A piezo-ultrasonic (EMS, Nyon, Switzerland) device was used to prepare a rectangular bony window in the lateral wall of maxillary sinus, the buccal bony plate was gently detached from the maxillary sinus membrane and placed in saline for preservation. The maxillary sinus membrane was then gently and thoroughly elevated. A syringe was used to aspirate fluid from the maxillary sinus cyst by inserting it, while no visible object was extracted. The mucosa on the floor of the maxillary sinus was incised to extract the cyst, revealing perforation in the same mucosal area. The perforation in the mucosa were covered by collagen membrane (Bio-Gide, Geistlich Pharma, Wolhusen, Switzerland), and 1g bone substitutes (Bio-Oss, Geistlich Pharma, Wolhusen, Switzerland) were placed in maxillary sinus cavity (Figure 2).
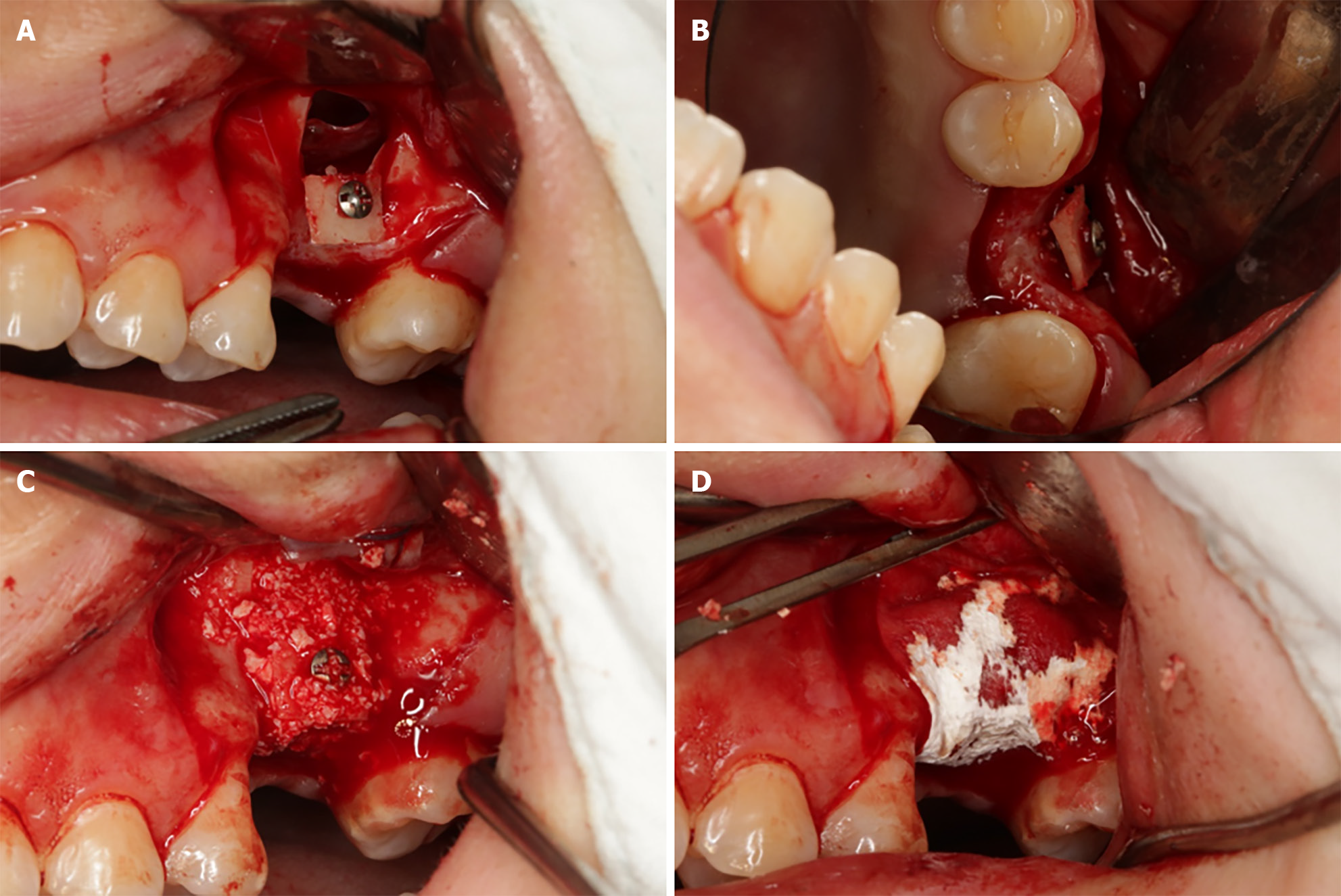
A micro titanium screw was used to penetrate the center of the bony window and fixed to the buccal side of the alveolar bone in the edentulous area, the space between the bone plate and the alveolar ridge was filled with Bio-Oss bone substitutes and the bone plate were covered with collagen membrane (Bio-Gide, Geistlich Pharma, Wolhusen, Switzerland), and the incision was closed tightly with tension-free sutures (Figure 3). Postoperative instructions and antibiotics were given to the patient.
Nine months later, CBCT showed that the ABH was 15.6 mm and ABW was 10.5 mm. Also, the thickness of sinus membrane was normal and the pseudocyst was disappeared (Figure 4). A Straumann BLT dental implant (Straumann®, 4.1 mm × 10 mm, Switzerland) was placed conventionally. A screw-retained all-ceramic restoration was installed 4 months later (Figure 5).
The 1-year follow-up visit showed that the implant was succeeded according to the criteria proposed by Albrektsson et al[13].
The lateral bony window in maxillary sinus lift was opened by either a round drill or ultrasonic tips, it was usually treated in the following 4 ways: Elevated into the newly formed sinus cavity, discarded, repositioned after placing the bone graft, or utilized as a bone graft material[14].
Cortical bone tenting is a technique in which a thin cortical bone sheet is anchored to the alveolar bone by titanium nails and the space below is filled with bone graft material[2]. The thin cortical bone sheet provides a "natural biological membrane" effect and allows neovascularization to grow into the bone graft particles. The distance of the bone gain is not limited by the size of the collected bone mass as in the autologous bone grafting technique, and more bone width and less bone resorption can be achieved than with autologous bone grafting[3,15]. Traditionally, cortical bone plates are taken from the mandibular ramus or the chin. It is reported that the most frequent complication in the donor area is chin paresthesia, primarily associated with grafts harvested from the symphysis[3]. In this case, the bone plate from the lateral wall of the maxillary sinus lift was used for the cortical bone tenting technique without a separate second operative area, which not only reduced the patient’s postoperative trauma, but also shortened the operative time and postoperative pain[16,17].
In this case, the largest possibility in the patient’s maxillary sinus is most likely a pseudocyst, as the patient is asymptomatic, and it presents a typical well-defined ’dome-shaped’ lesion on CBCT imaging. There is currently no consensus on the management regarding such pseudocysts. Some scholars believe that these pseudocysts may potentially lead to infection of bone graft material; therefore, a two-stage treatment approach is recommended[8]. This involves the removal of the cyst first, allowing for healing, followed by maxillary sinus floor elevation surgery. In contrast, studies by other scholars have shown that bone grafting can be performed during the same period of time as the removal of the cyst, with favorable results[9,11]. In this case, there were no contents in the lesion when we aspirated it during operation, and the patient did not have any symptoms preoperatively, so we chose to cover the maxillary membrane perforation with a collagen membrane directly after removing the lesion and perform bone grafting at the same time to minimize the number of surgeries and the patient’s waiting period for the missing teeth. The CBCT showed that the pseudocyst was disappeared thoroughly after 9 months, indicating that the lesion had been removed. The patient had no postoperative complications and healed well.
The bone plate from lateral window approach for sinus augmentation can be an alternative donor site for severe horizontal bone augmentation in maxillary posterior region. In asymptomatic preoperative pseudocysts in the maxillary sinus and in which no specific intraoperative contents were aspirated, removal of the lesion for simultaneous maxillary sinus floor elevation can also yield good results.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Yuan K, Taiwan S-Editor: Zheng XM L-Editor: A P-Editor: Yu HG
| 1. | Scott R. ITI treatment guide, volume 5: sinus floor elevation procedures. Br Dent J. 2012;212:512. [RCA] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 2. | Le B, Burstein J, Sedghizadeh PP. Cortical tenting grafting technique in the severely atrophic alveolar ridge for implant site preparation. Implant Dent. 2008;17:40-50. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 38] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 3. | Aloy-Prósper A, Carramolino-Cuéllar E, Peñarrocha-Oltra D, Soto-Peñaloza D, Peñarrocha-Diago M. Intraoral onlay block bone grafts versus cortical tenting technique on alveolar ridge augmentations: a systematic review. Med Oral Patol Oral Cir Bucal. 2022;27:e181-e190. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 10] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 4. | Iușan SAL, Costache C, Lucaciu OP, Petrescu BN, Mirică IC, Toc DA, Albu S. Correlations between Dental Implant Infectious Pathologies and Maxillary Sinusitis: A Review Article. J Clin Med. 2023;12. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 5. | Shenoy SB, Talwar A, Shetty S, Anegundi RV. Etiology and Management of Complications Associated with Sinus Augmentation Procedures. J Hlth All Sci-India. 2021;11:113-118. [RCA] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 6. | Beaumont C, Zafiropoulos GG, Rohmann K, Tatakis DN. Prevalence of maxillary sinus disease and abnormalities in patients scheduled for sinus lift procedures. J Periodontol. 2005;76:461-467. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 64] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 7. | Mardinger O, Manor I, Mijiritsky E, Hirshberg A. Maxillary sinus augmentation in the presence of antral pseudocyst: a clinical approach. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;103:180-184. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 56] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 8. | Nosaka Y, Nosaka H, Nakajima Y, Tanioka T, Botticelli D, Baba S. A Reliable Surgical Procedure for Sinus Floor Augmentation with Antral Pseudocysts. Dent J (Basel). 2021;9. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 7] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 9. | Yu H, Qiu L. Histological and clinical outcomes of lateral sinus floor elevation with simultaneous removal of a maxillary sinus pseudocyst. Clin Implant Dent Relat Res. 2019;21:94-100. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 11] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 10. | Feng Y, Tang Y, Liu Y, Chen F, Li D. Maxillary sinus floor elevation using the osteotome technique in the presence of antral pseudocysts: a retrospective study with an average follow-up of 27 months. Int J Oral Maxillofac Implants. 2014;29:408-413. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 11] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 11. | Yu H, Tang Y, He D, Qiu L. Immediately or delayed sinus augmentation after pseudocyst removal: A randomized trial. Clin Implant Dent Relat Res. 2023;25:967-973. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 12. | Fang Y, Bi Y, Mashrah MA, Su Y, Ge L, Dong Y, Qin L, Wang L. Does the Presence of Pathological Change in the Schneiderian Membrane Increase the Risk of Membrane Perforation During Sinus Floor Elevation? A Systemic Review. J Oral Implantol. 2022;48:147-157. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 13. | Albrektsson T, Zarb G, Worthington P, Eriksson AR. The long-term efficacy of currently used dental implants: a review and proposed criteria of success. Int J Oral Maxillofac Implants. 1986;1:11-25. [PubMed] |
| 14. | Juzikis E, Gaubys A, Rusilas H. Uses of maxillary sinus lateral wall bony window in an open window sinus lift procedure: literature review. Stomatologija. 2018;20:14-21. [PubMed] |
| 15. | Morad G, Khojasteh A. Cortical tenting technique versus onlay layered technique for vertical augmentation of atrophic posterior mandibles: a split-mouth pilot study. Implant Dent. 2013;22:566-571. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 25] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 16. | Anitua E, Alkhraisat MH, Miguel-Sánchez A, Orive G. Surgical correction of horizontal bone defect using the lateral maxillary wall: outcomes of a retrospective study. J Oral Maxillofac Surg. 2014;72:683-693. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 17] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 17. | Berberi A, Nader N, Noujeim Z, Scardina A, Leone A, Salameh Z. Horizontal and vertical reconstruction of the severely resorbed maxillary jaw using subantral augmentation and a novel tenting technique with bone from the lateral buccal wall. J Maxillofac Oral Surg. 2015;14:263-270. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |