Published online Apr 26, 2024. doi: 10.12998/wjcc.v12.i12.2009
Peer-review started: November 30, 2023
First decision: February 2, 2024
Revised: February 9, 2024
Accepted: March 26, 2024
Article in press: March 26, 2024
Published online: April 26, 2024
Processing time: 137 Days and 23.5 Hours
In the evolving landscape of cardiac rehabilitation (CR), adopting digital technologies, including synchronous/real-time digital interventions and smart applications, has emerged as a transformative approach. These technologies offer real-time health data access, continuous vital sign monitoring, and personalized educational enhanced patient self-management and engagement. Despite their potential benefits, challenges and limitations exist, necessitating careful consideration. Synchronous/real-time digital CR involves remote, two-way audiovisual communication, addressing issues of accessibility and promoting home-based interventions. Smart applications extend beyond traditional healthcare, providing real-time health data and fostering patient empowerment. Wearable devices and mobile apps enable continuous monitoring, tracking of rehabilitation outcomes, and facilitate lifestyle modifications crucial for cardiac health maintenance. As digital CR progresses, ensuring patient access, equitable implementation, and addressing the digital divide becomes paramount. Artificial intelligence holds promise in the early detection of cardiac events and tailoring patient-specific CR programs. However, challenges such as digital literacy, data privacy, and security must be addressed to ensure inclusive implementation. Moreover, the shift toward digital CR raises concerns about cost, safety, and potential depersonalization of therapeutic relationships. A transformative shift towards technologically enabled CR necessitates further research, focusing not only on technological advancements but also on customization to meet diverse patient needs. Overcoming challenges related to cost, safety, data security, and potential depersonalization is crucial for the widespread adoption of digital CR. Future studies should explore integrating moral values into digital therapeutic relationships and ensure that digital CR is accessible, equitable, and seamlessly integrated into routine cardiac care. Theoretical frameworks that accommodate the dynamic quality of real-time monitoring and feedback feature of digital CR interventions should be considered to guide intervention development.
Core Tip: Digital technologies have revolutionized cardiac rehabilitation (CR), offering flexible and novel approaches to care. The integration of digital health technologies and artificial intelligence in remote CR is transforming traditional paradigms, providing real-time access to health data, and enhancing patient self-management. Mobile and digital CR models, including synchronous/real-time digital interventions, are addressing accessibility barriers, and promoting equity in healthcare delivery. Despite the potential benefits, challenges such as the digital divide, cost, safety, and data security must be addressed. Future research should prioritize accessibility, equity, and the seamless integration of digital CR into routine cardiac care.
- Citation: Pepera G, Antoniou V, Su JJ, Lin R, Batalik L. Comprehensive and personalized approach is a critical area for developing remote cardiac rehabilitation programs. World J Clin Cases 2024; 12(12): 2009-2015
- URL: https://www.wjgnet.com/2307-8960/full/v12/i12/2009.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i12.2009
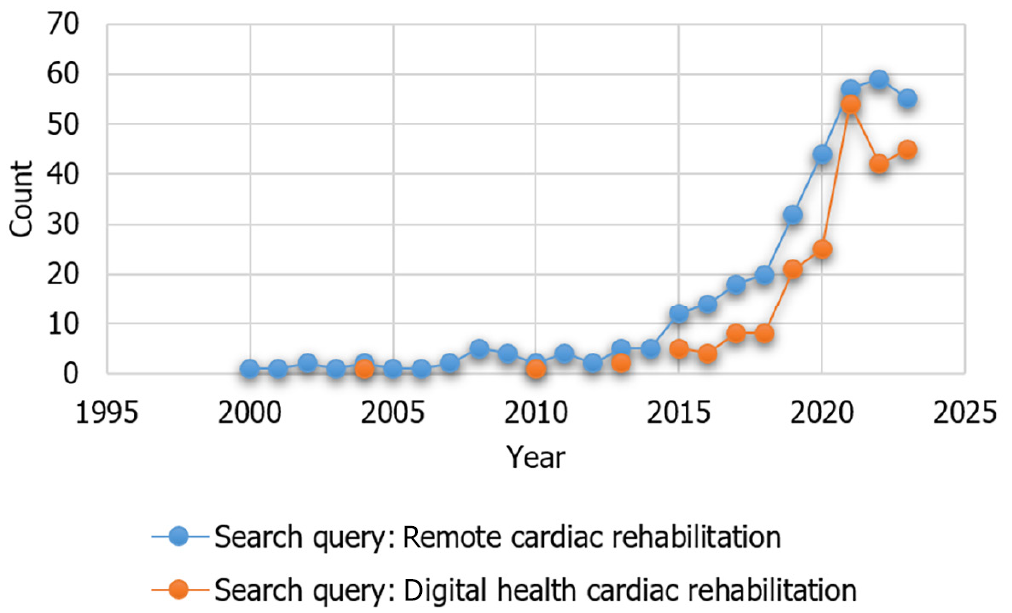
Cardiac rehabilitation (CR) is a comprehensive program that includes risk factor management, exercise training, and optimization of psychosocial health[1,2]. It is recommended by guidelines for individuals with cardiovascular disease (CVD)[3]. Numerous studies have demonstrated that participation in CR programs following a cardiac event, such as myocardial infarction or percutaneous coronary intervention, is associated with improved health outcomes and reduced mortality rates[4,5]. Despite its well-established benefits, CR remains underutilized, and there exist significant differences in referral, admission, and completion rates[6]. With the increasing body of literature on the topic, there is a growing interest in exploring novel delivery models for CR, particularly digital and remote approaches (Figure 1). These innovative models have the potential to enhance participation in CR programs, ultimately leading to better health outcomes for individuals with CVD[7]. Remote delivery of CR has received endorsement from international sources, including the European Association of Preventive Cardiology (EAPC)[8]. The EAPC has emphasized the importance of maintaining the delivery of core components of CR through tele-rehabilitation interventions during the COVID-19 pandemic. However, concerns have been raised regarding equity in the use of technology to ensure access to equitable access to outpatient care.
Research findings indicate that alternative delivery models for CR are not only safe but also yield similar effect as standard center-based CR programs[9-11]. However, significant questions remain unanswered regarding which specific remote CR models offer the most substantial benefits for individuals. In this editorial, we aim to provide an overview of various remote CR models and identify key research questions that demand attention. We propose strategies for addressing these questions, which can serve as a valuable solution for scientists, researchers, and clinicians in the field. Two central research focuses emerge as crucial: First, the development of personalized remote CR programs; and second, the implementation of comprehensive methodologies to ensure the delivery of core CR components. Establishing these essential priorities is vital to ensure the provision of high-quality remote CR programs and can serve as a basis for future investigations.
Adopting a comprehensive and personalized approach is crucial for enhancing remote CR programs. This includes addressing issues related to equity in technology access, ensuring that all individuals who could benefit from CR have equal opportunities to participate[12]. Additionally, these programs should prioritize individualized care, tailoring interventions to each patient's specific needs and preferences in both short and longer term[13]. Embracing innovative methods and technology, such as virtual, remote, or mobile CR, can enable the delivery of comprehensive and personalized care to a broader population[14], ultimately improving access and health outcomes for individuals with car
Synchronous/real-time digital CR represents a contemporary alternative mode of CR delivery defined by real-time, two-way, remote audiovisual communication between patients and CR staff[16]. This approach primarily relies on real-time communication via videoconferencing platforms and remote monitoring of vital signs, such as electrocardiography, blood pressure, and heart rate, to facilitate safe and comprehensive home-based digital CR interventions[17]. Data from recent literature support the feasibility of synchronous/real-time digital CR interventions in enhancing the overall cardiac profile via improvements in cardiorespiratory fitness, physical activity levels and quality of life[18]. Despite the initial investment required for digital infrastructure, the cost-effectiveness of digital CR is highly advocated[19]. Furthermore, several barriers to CR enrolment and attendance such as transportation costs, lack of free time and remote residence locations, can be effectively addressed through the implementation of synchronous/real-time digital CR interventions[20]. Additionally, incorporating digitally delivered CR interventions could serve as the sole alternative solution for the continuation of CR during pandemic circumstances in the foreseeing future[21]. Though, numerous logistical, ethical, and clinical issues arise with digital CR, primarily concerning the risk of online patients’ personal data leakage, insufficient internet access and digital literacy. It is essential to prioritize underrepresented racial and ethnic groups, women and older patients for integration into digital synchronous CR[22]. Bearing in mind that the acceptance of digitally delivered CR services and interventions is generally high[23], there is a strong need to further investigate and incorporate synchronous digital CR into the routine of cardiac patients’ secondary prevention routine.
In the evolving landscape of remote CR, the transition toward mobile health technology interventions represents a transformative approach to providing more personalized and accessible cardiac care. These technologies extend beyond the traditional healthcare setting, providing real-time access to health data and fostering patient empowerment in their care management. Wearable devices and mobile applications enable continuous monitoring of vital signs and physical activities, contributing directly to the enhancement of patient self-management[24,25]. This approach is particularly crucial in remote settings[25], where traditional healthcare resources are less accessible, emphasizing the need for patient-centered care that adapts to their lifestyle and environment. Mobile platforms not only facilitate the tracking of rehabilitation outcomes but also play a critical role in lifestyle modifications essential for cardiac health maintenance[26,27]. Additionally, the provision of customized educational content and reminders through these platforms ensures sustained patient engagement and informed participation in their rehabilitation journey[28]. The transition to mobile CR represents a significant move towards redefining patient care in CR, focusing on technology's role in enabling a more dynamic, responsive, and patient-tailored approach.
The integration of digital technologies in CR has sparked discussion about selecting appropriate measures for outcome evaluation, as traditional methods fall short in capturing the dynamic and real-time nature of digitalized interventions. Unlike the static measures from center-based CR trials, digital platforms offer granularity, real-time, and precision through automated, real-time tracking and analysis using sensors and monitors for heart rate, blood pressure and movement[18]. This is crucial as increased digital technology-based theories guiding interventional studies highlighted the dynamic qualities and emphasized the need to unpack the use of technology at home to explain the causal-effect relationship[29].
The formality of the digital CR intervention is diverse and changing rapidly, such as virtual reality, gamification, robot assisted, Chatbot (AI-powered). When researchers use digital technology to deliver CR, the focus is often on evaluating a specific technology such as a wearable device, certain virtual reality scenario, or mobile app, within short duration. The safety and ethical issues should be considered before recommending them as a new standard of care, such as discomfort
Artificial intelligence applies to the use of Information and Communication Technologies (commonly referred to as ICTs) for data-driven policy decision. AI has been broadly studied in various fields such as medicine[30] and economics[31] and is currently embedded in the CR implementation procedures. By engaging AI technology via wearable sensors (worn as wristbands or embedded in smartwatches), early detection of cardiac events is promoted, thereby enhancing the safety of home-based CR interventions, and improving clinician decision-making[32]. Additionally, AI tools offer real-time feedback and support to patients, which could contribute to the improvement of CR adherence, increase of patients’ engagement and the proliferation of their overall cardiac profile[18,28]. The potential of the AI tools to analyze thoroughly the large amounts of data collected by ICT devices enables the provision of patient-tailored CR programs and serves as a cornerstone for improving health outcomes and quality of life. However, the incorporation of digital technology into the CR procedures raises several challenges to be addressed. Innovative technologies such AI might require digital literacy[29]. Consequently, those patients with limited digital literacy may be denied access to AI–based CR; thus, leading to health inequality. Furthermore, considering the importance of data privacy and security, measures should be taken to prevent the unethical use of patients’ data and ensure transparency, fairness, and accountability in algorithmically automated decisions. AI can act as an alternative key component potential enough to improve the efficiency and effectiveness of home-based CR interventions[32]. However, further research is needed to maximize their comprehensive and optimal implementation.
Digital technologies in CR offer a transformative shift from traditional supervised programs to proactive, remotely supported self-care approaches, enhancing accessibility and sustainability. However, this rapid technological advancement risks deepening the digital divide, particularly impacting those with lower socio-economic and educational backgrounds, women, people with disabilities, and those with sensory or motor impairments[33]. Future research should focus not just on technological advancements but also on customizing these interventions to meet the diverse needs and preferences of these subgroups (Table 1). It is crucial to view technology to overcome barriers to CR participation, rather than as the central focus.
| No. | Items | Description |
| 1 | Enhance AI and ICT Integration | Continue to embed AI in CR procedures, using wearable sensors for early cardiac event detection, thereby improving home-based CR safety and clinician decision-making |
| 2 | Provide real-time feedback | Utilize AI tools to offer real-time feedback and support to patients, aiming to improve CR adherence and patient engagement |
| 3 | Develop patient-tailored programs | Use AI to thoroughly analyze data from ICT devices for creating personalized CR programs, enhancing health outcomes and quality of life |
| 4 | Address digital literacy gaps | Recognize the challenge of digital literacy and work to make AI-based CR accessible to all patients, reducing health inequalities |
| 5 | Ensure data privacy and security | Focus on ethical considerations, including data privacy, security, and the transparency of AI decision-making processes |
| 6 | Evaluate cost and safety concerns | Study the financial and safety implications of implementing digital technologies in CR, especially in unsupervised settings |
| 7 | Customize interventions for diverse needs | Tailor digital CR interventions to meet the varied needs and preferences of different patient subgroups, such as those with lower socio-economic status or disabilities |
| 8 | Maintain the human interaction in digital CR | Address concerns of depersonalization by integrating moral values into digital therapeutic relationships, ensuring compassionate, patient-centered care |
Moreover, the implementation of digital technologies in CR brings forth concerns about cost and safety[34]. The expenses associated with acquiring and maintaining advanced digital health tools can be substantial, potentially limiting their widespread adoption, especially in resource-constrained settings[35]. Additionally, ensuring safety while using these technologies remotely poses a significant challenge. This includes managing the risk of incorrect usage of equipment, ensuring accurate data transmission, and providing immediate assistance in case of adverse events during unsupervised exercise sessions[18].
Equally important is the concern over data security in digital CR[36]. As patient health information and sensitive data are transmitted and stored digitally, there is a heightened risk of data breaches and unauthorized access[37]. Ensuring the confidentiality, integrity, and availability of patient data is paramount, requiring robust cybersecurity measures and adherence to data protection regulations. This aspect is crucial to maintaining patient trust and the credibility of digital CR programs.
Furthermore, the scope of technology in CR could be broadened to include interventions aimed at preventing CVDs. This may involve managing risk factors in high-risk groups or individuals with metabolic syndrome[38]. Additionally, there is potential for extending CR to patients with co-morbid conditions, such as cancer, who may require cardio-oncology interventions. While CR is traditionally recognized for secondary prevention[39], expanding its application to primary or palliative care settings requires more evidence.
The technologically enabled CR can facilitate culturally sensitive communication and reduce stigma in mental health assessments and psychological interventions. However, this raises concerns about depersonalization, where authentic care and interpersonal connection in therapeutic relationships might be overshadowed by interactions with technology[40,41]. Future studies should explore ways to integrate moral values such as compassion and caring into digital therapeutic relationships, preserving the human element in healthcare[42].
CR has evolved significantly with the advent of digital technologies, offering novel and flexible approaches to delivering care. The integration of digital health technologies and AI in remote CR has transformed the traditional paradigms of cardiac care. These technologies provide real-time health data access, enable continuous monitoring of vital signs and physical activities, and offer personalized educational content, thereby enhancing patient self-management and engagement. The shift towards mobile and digital CR models, including synchronous/real-time digital interventions, addresses barriers such as physical access to care and promotes equity in healthcare delivery. However, adopting these technologies also presents challenges, including the need for digital literacy among patients and concerns regarding data privacy and security. Future research should ensure that digital CR is accessible, equitable, and effectively integrated into routine cardiac care (Table 1). This entails developing personalized remote CR programs and implementing comprehensive methodologies to deliver core CR components.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: Czech Republic
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Ueda H, Japan S-Editor: Che XX L-Editor: A P-Editor: Yu HG
| 1. | Thomas RJ, Balady G, Banka G, Beckie TM, Chiu J, Gokak S, Ho PM, Keteyian SJ, King M, Lui K, Pack Q, Sanderson BK, Wang TY. 2018 ACC/AHA Clinical Performance and Quality Measures for Cardiac Rehabilitation: A Report of the American College of Cardiology/American Heart Association Task Force on Performance Measures. J Am Coll Cardiol. 2018;71:1814-1837. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 105] [Cited by in RCA: 143] [Article Influence: 20.4] [Reference Citation Analysis (0)] |
| 2. | Visseren FLJ, Mach F, Smulders YM, Carballo D, Koskinas KC, Bäck M, Benetos A, Biffi A, Boavida JM, Capodanno D, Cosyns B, Crawford C, Davos CH, Desormais I, Di Angelantonio E, Franco OH, Halvorsen S, Hobbs FDR, Hollander M, Jankowska EA, Michal M, Sacco S, Sattar N, Tokgozoglu L, Tonstad S, Tsioufis KP, van Dis I, van Gelder IC, Wanner C, Williams B; ESC Scientific Document Group. 2021 ESC Guidelines on cardiovascular disease prevention in clinical practice. Eur J Prev Cardiol. 2022;29:5-115. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 303] [Article Influence: 75.8] [Reference Citation Analysis (0)] |
| 3. | Verdicchio C, Freene N, Hollings M, Maiorana A, Briffa T, Gallagher R, Hendriks JM, Abell B, Brown A, Colquhoun D, Howden E, Hansen D, Reading S, Redfern J. A Clinical Guide for Assessment and Prescription of Exercise and Physical Activity in Cardiac Rehabilitation. A CSANZ Position Statement. Heart Lung Circ. 2023;32:1035-1048. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 27] [Reference Citation Analysis (0)] |
| 4. | Dibben GO, Faulkner J, Oldridge N, Rees K, Thompson DR, Zwisler AD, Taylor RS. Exercise-based cardiac rehabilitation for coronary heart disease: a meta-analysis. Eur Heart J. 2023;44:452-469. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 106] [Cited by in RCA: 166] [Article Influence: 83.0] [Reference Citation Analysis (0)] |
| 5. | Ekblom Ö, Cider Å, Hambraeus K, Bäck M, Leosdottir M, Lönn A, Börjesson M. Participation in exercise-based cardiac rehabilitation is related to reduced total mortality in both men and women: results from the SWEDEHEART registry. Eur J Prev Cardiol. 2022;29:485-492. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 32] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 6. | Smith JR, Thomas RJ, Bonikowske AR, Hammer SM, Olson TP. Sex Differences in Cardiac Rehabilitation Outcomes. Circ Res. 2022;130:552-565. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 59] [Article Influence: 19.7] [Reference Citation Analysis (0)] |
| 7. | Beatty AL, Beckie TM, Dodson J, Goldstein CM, Hughes JW, Kraus WE, Martin SS, Olson TP, Pack QR, Stolp H, Thomas RJ, Wu WC, Franklin BA. A New Era in Cardiac Rehabilitation Delivery: Research Gaps, Questions, Strategies, and Priorities. Circulation. 2023;147:254-266. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 79] [Reference Citation Analysis (0)] |
| 8. | Taylor RS, Dalal HM, McDonagh STJ. The role of cardiac rehabilitation in improving cardiovascular outcomes. Nat Rev Cardiol. 2022;19:180-194. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 192] [Cited by in RCA: 253] [Article Influence: 84.3] [Reference Citation Analysis (1)] |
| 9. | Nacarato D, Sardeli AV, Mariano LO, Chacon-Mikahil MPT. Cardiovascular telerehabilitation improves functional capacity, cardiorespiratory fitness and quality of life in older adults: A systematic review and meta-analysis. J Telemed Telecare. 2022;1357633X221137626. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 5] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 10. | Owen O, O'Carroll V. The effectiveness of cardiac telerehabilitation in comparison to centre-based cardiac rehabilitation programmes: A literature review. J Telemed Telecare. 2022;1357633X221085865. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 9] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 11. | Stefanakis M, Batalik L, Antoniou V, Pepera G. Safety of home-based cardiac rehabilitation: A systematic review. Heart Lung. 2022;55:117-126. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 92] [Cited by in RCA: 88] [Article Influence: 29.3] [Reference Citation Analysis (0)] |
| 12. | Ebinger JE, Lan R, Driver MP, Rushworth P, Luong E, Sun N, Nguyen TT, Sternbach S, Hoang A, Diaz J, Heath M, Claggett BL, Bairey Merz CN, Cheng S. Disparities in Geographic Access to Cardiac Rehabilitation in Los Angeles County. J Am Heart Assoc. 2022;11:e026472. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 10] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 13. | Thomas RJ, Sapir O, Gomes PF, Iftikhar U, Smith JR, Squires RW. Advances, Challenges, and Progress in Cardiac Rehabilitation in Chronic CVD Management. Curr Atheroscler Rep. 2023;25:247-256. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 14. | Content VG, Abraham HM, Kaihoi BH, Olson TP, Brewer LC. Novel Virtual World-Based Cardiac Rehabilitation Program to Broaden Access to Underserved Populations: A Patient Perspective. JACC Case Rep. 2022;4:911-914. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 15. | Lee KCS, Breznen B, Ukhova A, Koehler F, Martin SS. Virtual healthcare solutions for cardiac rehabilitation: a literature review. Eur Heart J Digit Health. 2023;4:99-111. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 20] [Reference Citation Analysis (0)] |
| 16. | Beatty AL, Brown TM, Corbett M, Diersing D, Keteyian SJ, Mola A, Stolp H, Wall HK, Sperling LS. Million Hearts Cardiac Rehabilitation Think Tank: Accelerating New Care Models. Circ Cardiovasc Qual Outcomes. 2021;14:e008215. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 42] [Article Influence: 10.5] [Reference Citation Analysis (0)] |
| 17. | Hwang R, Gane EM, Morris NR. No transport? No worries! Cardiac telerehabilitation is a feasible and effective alternative to centre-based programs. Heart Fail Rev. 2023;28:1277-1284. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 7] [Reference Citation Analysis (0)] |
| 18. | Golbus JR, Lopez-Jimenez F, Barac A, Cornwell WK 3rd, Dunn P, Forman DE, Martin SS, Schorr EN, Supervia M; Exercise, Cardiac Rehabilitation and Secondary Prevention Committee of the Council on Clinical Cardiology; Council on Lifelong Congenital Heart Disease and Heart Health in the Young; Council on Quality of Care and Outcomes Research; and Council on Cardiovascular and Stroke Nursing. Digital Technologies in Cardiac Rehabilitation: A Science Advisory From the American Heart Association. Circulation. 2023;148:95-107. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 41] [Reference Citation Analysis (0)] |
| 19. | Kyaw TL, Ng N, Theocharaki M, Wennberg P, Sahlen KG. Cost-effectiveness of Digital Tools for Behavior Change Interventions Among People With Chronic Diseases: Systematic Review. Interact J Med Res. 2023;12:e42396. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 20. | Antoniou V, Pasias K, Loukidis N, Exarchou-Kouveli KK, Panagiotakos DB, Grace SL, Pepera G. Translation, Cross-Cultural Adaptation and Psychometric Validation of the Greek Version of the Cardiac Rehabilitation Barriers Scale (CRBS-GR): What Are the Barriers in South-East Europe? Int J Environ Res Public Health. 2023;20. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 13] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 21. | Gibson I, McCrudden Z, Dunne D, Harris A, Hynes L, Murphy E, Murphy AW, Byrne M, McEvoy JW. Harnessing digital health to optimise the delivery of guideline-based cardiac rehabilitation during COVID-19: an observational study. Open Heart. 2023;10. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 22. | Ghisi GLM, Kim WS, Cha S, Aljehani R, Cruz MMA, Vanderlei LCM, Pepera G, Liu X, Xu Z, Maskhulia L, Venturini E, Chuang HJ, Pereira DG, Trevizan PF, Kouidi E, Batalik L, Ghanbari Firoozabadi M, Burazor I, Jiandani MP, Zhang L, Tourkmani N, Grace SL. Women's Cardiac Rehabilitation Barriers: Results of the International Council of Cardiovascular Prevention and Rehabilitation's First Global Assessment. Can J Cardiol. 2023;39:S375-S383. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 29] [Article Influence: 14.5] [Reference Citation Analysis (0)] |
| 23. | Bäuerle A, Mallien C, Rassaf T, Jahre L, Rammos C, Skoda EM, Teufel M, Lortz J. Determining the Acceptance of Digital Cardiac Rehabilitation and Its Influencing Factors among Patients Affected by Cardiac Diseases. J Cardiovasc Dev Dis. 2023;10. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 11] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 24. | Lu L, Zhang J, Xie Y, Gao F, Xu S, Wu X, Ye Z. Wearable Health Devices in Health Care: Narrative Systematic Review. JMIR Mhealth Uhealth. 2020;8:e18907. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 240] [Article Influence: 48.0] [Reference Citation Analysis (0)] |
| 25. | Jones AK, Yan CL, Rivera Rodriquez BP, Kaur S, Andrade-Bucknor S. Role of wearable devices in cardiac telerehabilitation: A scoping review. PLoS One. 2023;18:e0285801. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Reference Citation Analysis (0)] |
| 26. | Karihtala K, Leivonen S-K, Karjalainen-Lindsberg M-L. Checkpoint protein expression in the tumor microenvironment defines the outcome of classical Hodgkin lymphoma patients. Blood Adv. 2022;6(6):1919-1931. Blood Adv. 2023;7:1432-1435. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 27. | Imran TF, Wang N, Zombeck S, Balady GJ. Mobile Technology Improves Adherence to Cardiac Rehabilitation: A Propensity Score-Matched Study. J Am Heart Assoc. 2021;10:e020482. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 20] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 28. | Bostrom J, Sweeney G, Whiteson J, Dodson JA. Mobile health and cardiac rehabilitation in older adults. Clin Cardiol. 2020;43:118-126. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 31] [Cited by in RCA: 44] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 29. | Baumel A, Muench FJ. Effort-Optimized Intervention Model: Framework for Building and Analyzing Digital Interventions That Require Minimal Effort for Health-Related Gains. J Med Internet Res. 2021;23:e24905. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 16] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 30. | He J, Baxter SL, Xu J, Zhou X, Zhang K. The practical implementation of artificial intelligence technologies in medicine. Nat Med. 2019;25:30-36. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 597] [Cited by in RCA: 940] [Article Influence: 156.7] [Reference Citation Analysis (0)] |
| 31. | Loukis EN, Maragoudakis M, Kyriakou N. Artificial intelligence-based public sector data analytics for economic crisis policymaking. Transform Gov-People. 2020;14:639-662. [RCA] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 32. | Sotirakos S, Fouda B, Mohamed Razif NA, Cribben N, Mulhall C, O'Byrne A, Moran B, Connolly R. Harnessing artificial intelligence in cardiac rehabilitation, a systematic review. Future Cardiol. 2022;18:154-164. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 13] [Reference Citation Analysis (0)] |
| 33. | Whitelaw S, Pellegrini DM, Mamas MA, Cowie M, Van Spall HGC. Barriers and facilitators of the uptake of digital health technology in cardiovascular care: a systematic scoping review. Eur Heart J Digit Health. 2021;2:62-74. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 128] [Cited by in RCA: 129] [Article Influence: 32.3] [Reference Citation Analysis (0)] |
| 34. | Rosa C, Marsch LA, Winstanley EL, Brunner M, Campbell ANC. Using digital technologies in clinical trials: Current and future applications. Contemp Clin Trials. 2021;100:106219. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 36] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 35. | Abernethy A, Adams L, Barrett M, Bechtel C, Brennan P, Butte A, Faulkner J, Fontaine E, Friedhoff S, Halamka J, Howell M, Johnson K, Long P, McGraw D, Miller R, Lee P, Perlin J, Rucker D, Sandy L, Savage L, Stump L, Tang P, Topol E, Tuckson R, Valdes K. The Promise of Digital Health: Then, Now, and the Future. NAM Perspect. 2022;2022. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 127] [Article Influence: 42.3] [Reference Citation Analysis (0)] |
| 36. | Bouabida K, Lebouché B, Pomey MP. Telehealth and COVID-19 Pandemic: An Overview of the Telehealth Use, Advantages, Challenges, and Opportunities during COVID-19 Pandemic. Healthcare (Basel). 2022;10. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 74] [Article Influence: 24.7] [Reference Citation Analysis (0)] |
| 37. | Basil NN, Ambe S, Ekhator C, Fonkem E. Health Records Database and Inherent Security Concerns: A Review of the Literature. Cureus. 2022;14:e30168. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 38. | Su JJ, Wong AK, Zhang LP, Bayuo J, Lin R, Abu-Odah H, Batalik L. Technology-assisted cardiac rehabilitation for coronary heart disease patients with central obesity: a randomized controlled trial. Eur J Phys Rehabil Med. 2024;60:95-103. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 1] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 39. | Winnige P, Vysoky R, Dosbaba F, Batalik L. Cardiac rehabilitation and its essential role in the secondary prevention of cardiovascular diseases. World J Clin Cases. 2021;9:1761-1784. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 57] [Cited by in RCA: 45] [Article Influence: 11.3] [Reference Citation Analysis (10)] |
| 40. | Barreda-Ángeles M, Hartmann T. Experiences of Depersonalization/Derealization Among Users of Virtual Reality Applications: A Cross-Sectional Survey. Cyberpsychol Behav Soc Netw. 2023;26:22-27. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 41. | Peckmann C, Kannen K, Pensel MC, Lux S, Philipsen A, Braun N. Virtual reality induces symptoms of depersonalization and derealization: A longitudinal randomised control trial. Comput Human Behav. 2022;131:107233. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 12] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 42. | Su JJ, Bayuo J, Lin RS, Batalik L, Chen X, Abu-Odah H, Chan EA. Providing compassionate care via eHealth. Nurs Ethics. 2024;9697330231196226. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Reference Citation Analysis (0)] |