Published online Apr 6, 2024. doi: 10.12998/wjcc.v12.i10.1851
Peer-review started: January 23, 2024
First decision: January 31, 2024
Revised: February 4, 2024
Accepted: March 18, 2024
Article in press: March 18, 2024
Published online: April 6, 2024
Processing time: 69 Days and 14.5 Hours
Para-aortic lymph nodes (PALNs) are common sites for the regional spread of cervical squamous cell carcinoma (SCC).
We report the case of a 36-year-old woman who presented with cervical SCC with multiple bulky PALNs, largest measured 4.5 cm × 5 cm × 10 cm. The patient was treated with radical intent with definitive chemoradiation using sequential dose-escalated adaptive radiotherapy, followed by maintenance chemotherapy. The patient achieved a complete response; she has been doing well since the completion of treatment with no evidence of the disease for 2 years.
Regardless of the size of PALN metastases of cervical carcinoma origin, it is still treatable (with radical intent) via concurrent chemoradiation. Adaptive radio
Core Tip: In rare case of locally advanced cervical cancer with massive para-aortic lymph node involvement, we demon
- Citation: Alzibdeh A, Mohamad I, Wahbeh L, Abuhijlih R, Abuhijla F. Can we triumph over locally advanced cervical cancer with colossal para-aortic lymph nodes? A case report. World J Clin Cases 2024; 12(10): 1851-1856
- URL: https://www.wjgnet.com/2307-8960/full/v12/i10/1851.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i10.1851
Cervical cancer is a gynecological cancer, with an incidence of 604127 recorded cases globally in 2020[1]. In Jordan, however, cervical cancer is considered a rare cancer, with 39 recorded cases according to the annual cancer registry by the Ministry of Health, and 115 new cases in 2020, according to the International Agency for Research on Cancer[1]. Locally advanced cancer, defined as International Federation of Gynecology and Obstetrics (FIGO) stage IB2 or higher, is treated with definitive chemoradiation and has a 5-year relative survival rate of 58%[2]. Many prognostic factors have been associated with poor survival in patients with locally advanced cervical cancer treated with chemoradiation. Such factors include enlarged regional lymph nodes on imaging, especially para-aortic lymph node (PALN) involvement (stage IIIC2)[3-5]. PALN metastasis was found to be an independent prognostic factor for survival[5].
In this study, we report a case of locally advanced cervical cancer with bulky PALN involvement. To our knowledge, the size of the lymph nodes in the reported case is the largest in the literature. There is no consensus regarding the radiation dose required to control the disease.
The patient was complaining of intermenstrual and postcoital bleeding for 2 months duration.
Her initial symptoms started 2 months prior to diagnosis (May 2021); as she complained of intermenstrual bleeding and postcoital bleeding that became more frequent with time.
Her medical history included endometriosis at the cesarean section scar, which was managed by resection and mesh reconstruction in 2008. She was not taking any medications and reported no family history of cancer. She was a working woman and did not smoke. The patient had been using combined oral contraceptives.
She was not on any medications and reported no family history of cancer.
Upon examination, her height was 59.84 in (152.00 cm), and her weight was 143.30 kg (65.14 Lb.). Her BMI was 28 kg/m2. Abdominal examination revealed a Pfannenstiel scar without tenderness or masses on palpation. Her vaginal examination was limited because the patient was nervous during examination and showed a narrowed vagina with an irregular cervical os surface. Bleeding was evident after examination. The inguinal lymph nodes were not palpable, and rectal and speculum examinations were not performed for patient comfort.
Her initial labs showed unremarkable kidney and liver function tests and a HGB level of 13.9 g/dL.
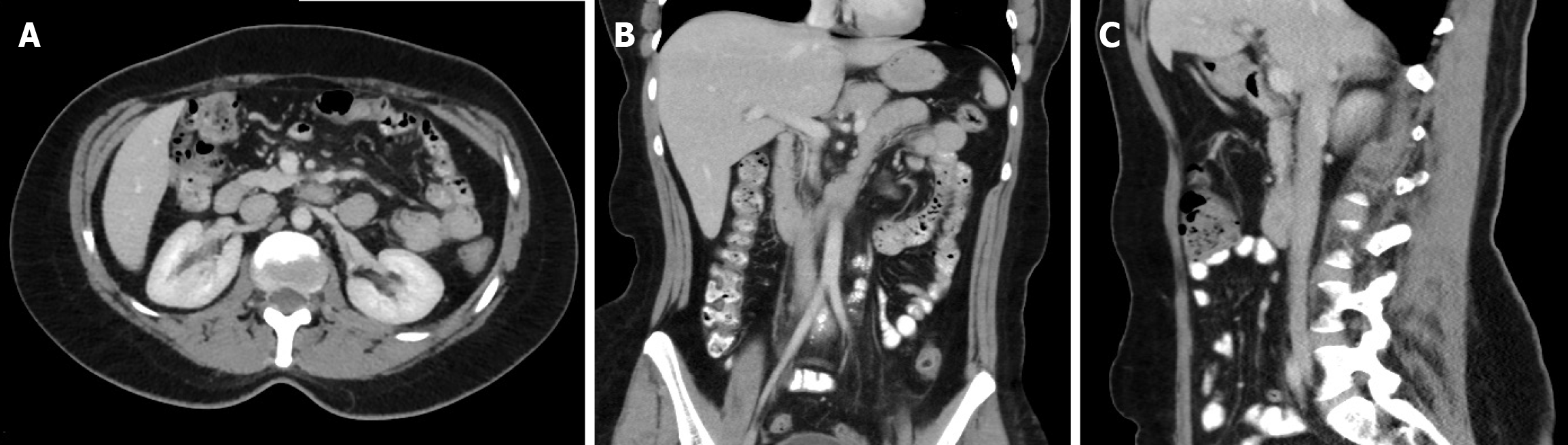
Initial pelvic MRI showed thickening of the external os, consistent with cervical cancer, with no definite parametrial invasion. Contrast CT of the chest, abdomen, and pelvis showed multiple enlarged para-aortic and pelvic lymph nodes, some of which showed foci of calcification, measuring up to 4.8 cm in the short axis (Figure 1).
Her case was discussed in a weekly multidisciplinary clinic for gynecological cancers at our institute, and FDG-18 whole-body PET/CT was recommended. FDG-18 whole body PET/CT scan showed multiple hypermetabolic enlarged abdomino-pelvic lymphadenopathy, involving: retrocrural, aorto-caval, retrocaval, bilateral para-aortic, bilateral common, external, and internal iliac lymph nodes, some of them with calcifications, the most prominent one is measuring about: 5 cm × 4.6 cm in max axial dimension with SUV max of 15. Otherwise, staging was negative for distant metastases.
After completing the workup, the case was discussed again in the multidisciplinary clinic for gynecological cancers, and the final staging was determined to be IIIC2 according to the 9th FIGO staging system. The recommended treatment plan was concurrent chemoradiotherapy with cisplatin-based chemotherapy and radiotherapy with external beam radiation therapy and brachytherapy, followed by subsequent assessment with imaging for possible surgical resection of any residual disease, if necessary.
Cervical poorly differentiated squamous cell carcinoma (stage IIIC2), according to 9th FIGO staging system.
Radiation treatment was planned over three sequential phases via volumetric arc radiotherapy (VMAT): 45 Gy/25 Fx to the primary tumor, upper vagina, parametrium, entire uterus, and elective and positive lymph nodes, as shown in Figure 2. The second and third phases were boost doses targeting the primary tumor and positive bulky lymph nodes up to 65 Gy, instead of brachytherapy. A brachytherapy boost was deferred as the patient had internal iliac deep vein thrombosis (DVT) with submissive pulmonary embolism (PE) and was deemed at moderate risk for general anesthesia after cardiology and respiratory assessment. In addition, the patient prognosis correlated with the nodal disease status rather than the primary disease since she had minimal thickening at the cervical os via MRI following the first phase. Anticoagulation therapy was initiated.
The patient started radiation treatment on September 15, 2021; she required one re-planning CT simulation during treatment as adaptive radiotherapy to account for nodal volume reduction. She also underwent a subsequent CT simulation to plan the boost phase. She completed her treatment on November 24, 2021, with a total duration of 71 d.
She concurrently started chemotherapy with 64 mg of cisplatin and 25 mg of mannitol. The patient received six cycles, and the last cycle was completed on October 24, 2021. Apart from her DVT and PE during treatment, the patient tolerated her treatment well and was seen weekly in a radiotherapy clinic with an acute Radiation Therapy Oncology Group gastrointestinal and genitourinary toxicity profile of grade 1.
After completing chemoradiotherapy, the patient was discussed again by the medical team within the multidisciplinary clinic, and the plan was to administer maintenance chemotherapy with carboplatin/paclitaxel-based therapy. She received five cycles, which were completed in February 2022.
The patient underwent a CT scan with contrast for the chest, abdomen, and pelvis on February 16, 2022, which showed excellent response with no residual uterine cervix tumor and no distant metastases. Stable calcified left para-aortic PALNs were also observed. Enlarged pelvic lymph nodes were not observed.
Follow-up imaging with MRI and CT on May 21, 2022, showed no local recurrence of cervical cancer. Pelvic lymph nodes were unremarkable. Stable calcified left para-aortic PALNs were also observed.
A Pap smear was performed on August 16, 2022, revealing radiation changes, negative for intraepithelial lesion or malignancy, and the subsequent smear on August 15, 2023, was within normal limits.
A CT scan was performed on October 13, 2022, which showed stable left para-aortic inferior calcified lymph nodes, the largest measuring 2 cm. Otherwise, no definite para-aortic, mesenteric, pelvic, or inguinal lymphadenopathy was observed. MRI was performed on January 15, 2023, and showed no suspicious recurrent or metastatic disease in the pelvis.
Her last follow-up images by chest, abdomen and pelvic CT scan and MRI in January 2024 showed a complete res
Cervical cancer comes fourth in global female cancers, and also the fourth most common cause of female mortality[1], however it is a rare cancer in Jordan, most likely due to the conservative culture of sexual practice before marriage, although under reporting is also a contributing factor, considering the imperfect cancer registry systems in developing countries like Jordan.
Locally advanced cancer is treated with definitive chemoradiation, and many prognostic factors have been found to be associated with poor survival in locally advanced cervical cancer treated with chemoradiation. These factors include large size of the primary tumor (> 6 cm), non-squamous cell carcinoma histology, advanced stage (IIIA-IVA), a lower pretreatment hemoglobin level (120 and 126 g/L have been identified as cut-off level/value), enlarged regional lymph nodes on imaging, especially PALN (stage IIIC2), HIV positivity, poor functional status, and treatment duration longer than 56 d[3-8]. Pelvic and PALN metastases were significantly associated with worse progression-free survival (PFS), whereas only PALN metastasis was an independent prognostic indicator of survival[5]. In one study, PALN involvement was the most important prognostic factor in radical radiotherapy for cervical cancer[4].
Oncological outcomes are worse with lymph node metastases and depend on the number, size, and affected region of nodal metastases[9,10]. The term 'bulky' nodes does not have an affixed definition, but a range of ≥ 1.5 or ≥ 2.0 cm of the short axis on imaging has been frequently reported in the literature[11-15]. One study showed that patients with large metastatic nodes (≥ 15 mm) are at an increased risk of early distant disease failure and death from distant metastasis[14]. Large positive pelvic or PALNs (> 10 mm) have been found to be associated with in-field failure after concurrent chemoradiotherapy[9]. A size ≥ 10 mm of the involved pelvis and PALNs was a significant prognostic factor for poor overall survival and disease-free survival rates[9].
Resection of bulky lymph nodes prior to radiotherapy may affect patient survival. A study published in 1995 found that survival was comparable for patients with completely resected bulky pelvic and common iliac nodes in comparison with patients with micrometastases, suggesting that resection prior to concurrent chemoradiotherapy may benefit patients, especially when higher doses may be required to eradicate bulky nodes[15]. There is a paucity of data regarding the dose of radiation that is sufficient to effectively treat bulky lymph nodes, particularly PALNs that reside at levels that require a significantly larger field of radiation.
A study published in 2014 studied 61 patients with locally advanced cervical cancer with nodal involvement (pelvis only in 67% and pelvis + para-aortic in 33%). The median nodal size was 1.8 cm, ranging from 0.7 cm to 4.5 cm. The patient was treated with concurrent chemoradiotherapy and brachytherapy. External beam radiotherapy was performed with extended-field intensity-modulated radiation therapy at a dose of 45 Gy in 25 fractions with simultaneous boost to the involved nodes to a median of 55 Gy in 25 fractions. Local failure rates were low (at a mean follow-up time of 29 months, eight patients experienced recurrence), suggesting that a dose of 55 Gy in 25 fractions was effective in treating the involved nodes[16].
Adjuvant systemic treatment after concurrent chemoradiotherapy is an area of research aimed at improving the outcomes of locally advanced cervical cancer. However, the OUTBACK trial showed that chemotherapy after concurrent chemoradiotherapy for locally advanced cervical cancer did not improve overall survival or PFS[17].
Despite their large size, bulky PALNs can still be treated with chemoradiation for locally advanced cervical carcinoma with curative intent. More prospective studies and trials are needed to fill in the gaps to determine the best radiation doses and regimens and the most suitable adjuvant treatments in terms of oncologic outcomes and toxicity profiles.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: Jordan
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Zeng C, United States S-Editor: Lin C L-Editor: A P-Editor: Zhao S
| 1. | Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, Bray F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J Clin. 2021;71:209-249. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75126] [Cited by in RCA: 64542] [Article Influence: 16135.5] [Reference Citation Analysis (176)] |
| 2. | Siegel RL, Miller KD, Jemal A. Cancer statistics, 2020. CA Cancer J Clin. 2020;70:7-30. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12667] [Cited by in RCA: 15305] [Article Influence: 3061.0] [Reference Citation Analysis (4)] |
| 3. | Endo D, Todo Y, Okamoto K, Minobe S, Kato H, Nishiyama N. Prognostic factors for patients with cervical cancer treated with concurrent chemoradiotherapy: a retrospective analysis in a Japanese cohort. J Gynecol Oncol. 2015;26:12-18. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 33] [Cited by in RCA: 43] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 4. | Yamashita H, Nakagawa K, Tago M, Shiraishi K, Nakamura N, Ohtomo K. Treatment results and prognostic analysis of radical radiotherapy for locally advanced cancer of the uterine cervix. Br J Radiol. 2005;78:821-826. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 18] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 5. | Liu J, Tang G, Zhou Q, Kuang W. Outcomes and prognostic factors in patients with locally advanced cervical cancer treated with concurrent chemoradiotherapy. Radiat Oncol. 2022;17:142. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 13] [Reference Citation Analysis (0)] |
| 6. | Kim HS, Park NH, Wu HG, Cho JY, Chung HH, Kim JW, Song YS, Kim SH, Kang SB. Matched-case comparison for the role of surgery in FIGO stage Ib1-IIa squamous cell carcinoma of cervix and suspicious para-aortic lymph node metastasis. Ann Surg Oncol. 2009;16:133-139. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 7. | Bush RS. The significance of anemia in clinical radiation therapy. Int J Radiat Oncol Biol Phys. 1986;12:2047-2050. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 172] [Cited by in RCA: 145] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 8. | Maiman M, Fruchter RG, Guy L, Cuthill S, Levine P, Serur E. Human immunodeficiency virus infection and invasive cervical carcinoma. Cancer. 1993;71:402-406. [PubMed] [DOI] [Full Text] |
| 9. | Oh J, Seol KH, Choi YS, Lee JW, Bae JY. Clinical significance of lymph node size in locally advanced cervical cancer treated with concurrent chemoradiotherapy. Yeungnam Univ J Med. 2019;36:115-123. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 9] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 10. | Ditto A, Martinelli F, Lo Vullo S, Reato C, Solima E, Carcangiu M, Haeusler E, Mariani L, Lorusso D, Raspagliesi F. The role of lymphadenectomy in cervical cancer patients: the significance of the number and the status of lymph nodes removed in 526 cases treated in a single institution. Ann Surg Oncol. 2013;20:3948-3954. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 57] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 11. | Choi KH, Kim JY, Lee DS, Lee YH, Lee SW, Sung S, Park HH, Yoon SC, Hur SY, Park JS, Kim YS. Clinical impact of boost irradiation to pelvic lymph node in uterine cervical cancer treated with definitive chemoradiotherapy. Medicine (Baltimore). 2018;97:e0517. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 24] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 12. | Kodama J, Seki N, Ojima Y, Nakamura K, Hongo A, Hiramatsu Y. Prognostic factors in node-positive patients with stage IB-IIB cervical cancer treated by radical hysterectomy and pelvic lymphadenectomy. Int J Gynaecol Obstet. 2006;93:130-135. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 19] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 13. | Inoue T, Chihara T, Morita K. The prognostic significance of the size of the largest nodes in metastatic carcinoma from the uterine cervix. Gynecol Oncol. 1984;19:187-193. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 31] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 14. | Song S, Kim JY, Kim YJ, Yoo HJ, Kim SH, Kim SK, Lim MC, Kang S, Seo SS, Park SY. The size of the metastatic lymph node is an independent prognostic factor for the patients with cervical cancer treated by definitive radiotherapy. Radiother Oncol. 2013;108:168-173. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 23] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 15. | Hacker NF, Wain GV, Nicklin JL. Resection of bulky positive lymph nodes in patients with cervical carcinoma. Int J Gynecol Cancer. 1995;5:250-256. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 149] [Cited by in RCA: 113] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 16. | Vargo JA, Kim H, Choi S, Sukumvanich P, Olawaiye AB, Kelley JL, Edwards RP, Comerci JT, Beriwal S. Extended field intensity modulated radiation therapy with concomitant boost for lymph node-positive cervical cancer: analysis of regional control and recurrence patterns in the positron emission tomography/computed tomography era. Int J Radiat Oncol Biol Phys. 2014;90:1091-1098. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 90] [Cited by in RCA: 98] [Article Influence: 8.9] [Reference Citation Analysis (0)] |
| 17. | Mileshkin LR, Moore KN, Barnes E, Gebski V, Narayan K, Bradshaw N, Lee YC, Diamante K, Fyles AW, Small W, Gaffney DK, Khaw P, Brooks S, Thompson JS, Huh WK, Carlson M, Amanda C. Adjuvant chemotherapy following chemoradiation as primary treatment for locally advanced cervical cancer compared to chemoradiation alone: The randomized phase III OUTBACK Trial (ANZGOG 0902, RTOG 1174, NRG 0274). J Clin Oncol. 2021;39:Suppl 18. [RCA] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 39] [Article Influence: 9.8] [Reference Citation Analysis (0)] |