Published online Apr 6, 2024. doi: 10.12998/wjcc.v12.i10.1837
Peer-review started: January 2, 2024
First decision: February 9, 2024
Revised: January 28, 2024
Accepted: March 18, 2024
Article in press: March 18, 2024
Published online: April 6, 2024
Processing time: 91 Days and 5.5 Hours
Percutaneous kyphoplasty (PKP) is a pivotal intervention for osteoporotic frac
A 58-year-old male patient, experiencing a T7 osteoporosis-related pathological compression fracture, underwent PKP at a local hospital. Two weeks post-procedure, the patient developed paraplegic and dysuric symptoms, necessitating emergency decompression surgery. Gradual improvement was achieved, marked by the restoration of muscle strength, sensation, and mobility.
PKP Intradural cement leakage following PKP is unusual and potentially fatal. Prompt imaging examinations, urgent evaluation, and the decompression surgery are essential, which help alleviate symptoms associated with spinal damage, markedly improving the overall prognosis.
Core Tip: The report describes the first documented case of a patient experiencing spinal cord injury, paraplegia, and cere
- Citation: Mao Z, Xiong ZH, Li JF. Thoracic spinal cord injury and paraplegia caused by intradural cement leakage after percutaneous kyphoplasty: A case report. World J Clin Cases 2024; 12(10): 1837-1843
- URL: https://www.wjgnet.com/2307-8960/full/v12/i10/1837.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i10.1837
Percutaneous vertebroplasty (PVP) and percutaneous kyphoplasty (PKP) have emerged as increasingly common techniques for treating osteoporotic and pathological vertebral compression fractures since the late 1980s, with PKP representing a refinement and advancement of PVP[1]. The mechanism of PKP encompasses the reinforcement of vertebral strength, enhancement of spinal stability, and alleviation of spinal pain. Comparative studies have demon
A 58-year-old male patient was admitted to our hospital complaining of lower back pain on September 15, 2023.
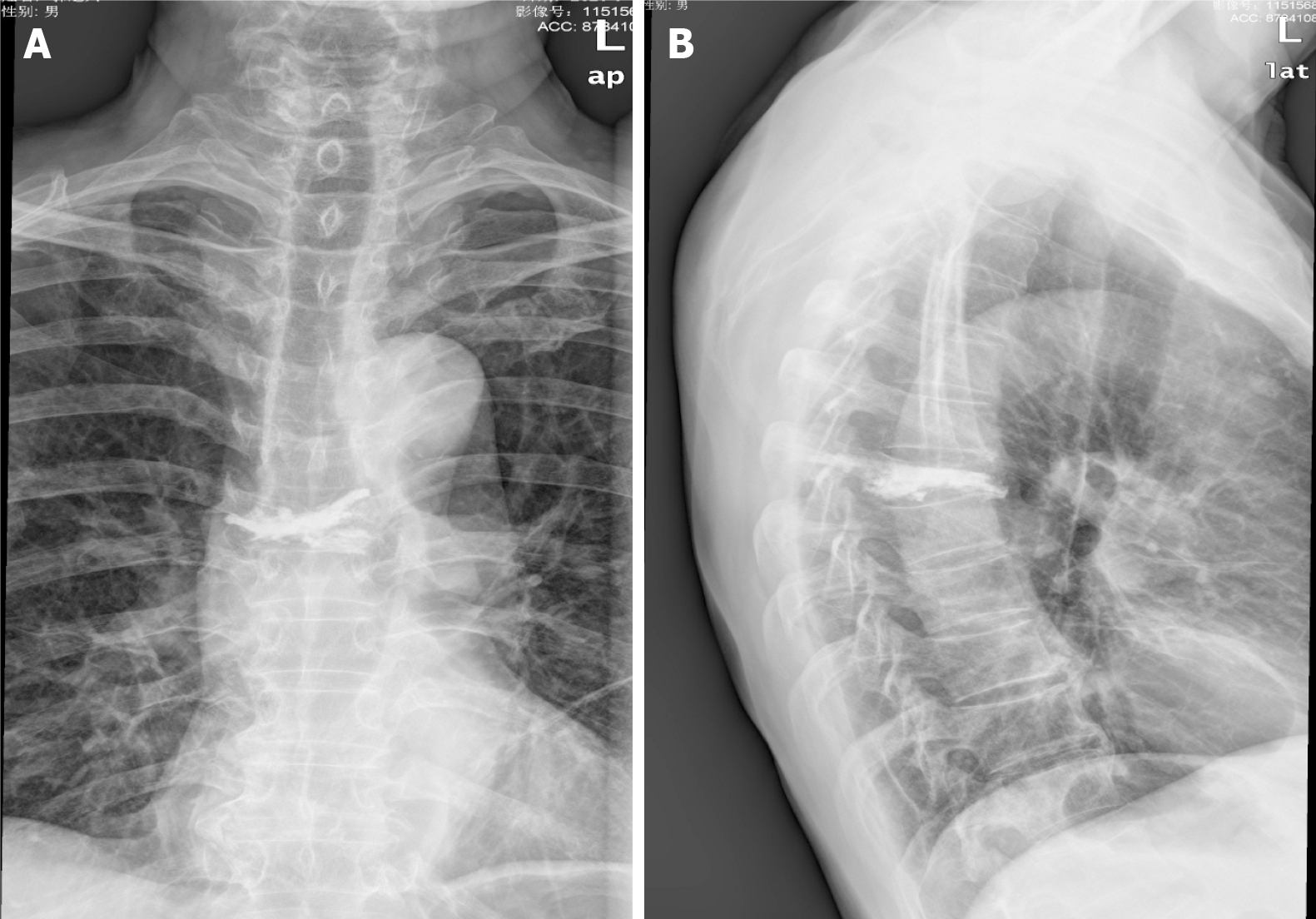
Two months before admission, the patient presented with lower back pain, leading to a diagnosis of herpes zoster at the local hospital outpatient clinic. Despite receiving oral medication and infusion therapy, the symptoms persisted. Subsequently, on August 27, the patient sought care at the Orthopedics Department of the local hospital and was admitted. He was diagnosed with T7 osteoporosis and a pathological compression fracture, prompting the performance of PKP on September 4 (Figure 1). Post-operation, the patient experienced relief from lower back pain; however, he developed bilateral hypochondrium pain and abdominal discomfort. Over the following week, the lower back pain and bilateral hypochondrium pain worsened, accompanied by progressive numbness and weakness in both lower extremities.
The patient had suffered from hypertension for 2 years and underwent PKP at a local hospital on September 4, 2023.
The patient's medical history inquiry revealed the absence of any pertinent familial medical background or genetic predispositions to the observed condition.
During the physical examination, the patient's vital signs were assessed and found to be stable: body temperature was 36.2°C, blood pressure was 120/78 mmHg, heart rate was 73 bpm, and respiratory rate was 20 breaths/min. Examinations of the heart, lungs, and abdomen revealed no specific findings. Upon special examination, positive results were noted for percussion tenderness of the thoracic spinous process, positive findings for extensive tenderness beside the spinous process, and positive tenderness in the bilateral hypochondrium. Muscle strength in both lower limbs, tendon reflexes, and cutaneous sensation exhibited no significant abnormalities. The visual analog scale (VAS) for pain was recorded as 6.
Routine blood examination, liver function, electrolyte, infectious disease-related laboratory tests, coagulation function, rheumatoid factors, and the antistreptolysin O test all yielded normal results. Abnormal test findings are detailed in Table 1.
| Tests | Results | Normal range |
| Triglyceride (mmol/L) | 3.94 | < 1.7 |
| Uric acid (μmol/L) | 649 | 208-428 |
| Creatinine (μmol/L) | 229 | 57-97 |
| C-reactive protein (mg/L) | 14.3 | ≤ 5 |
| Erythrocyte sedimentation rate (mm/h) | 49 | < 15 |
| Urine protein | 1+ | Negative |
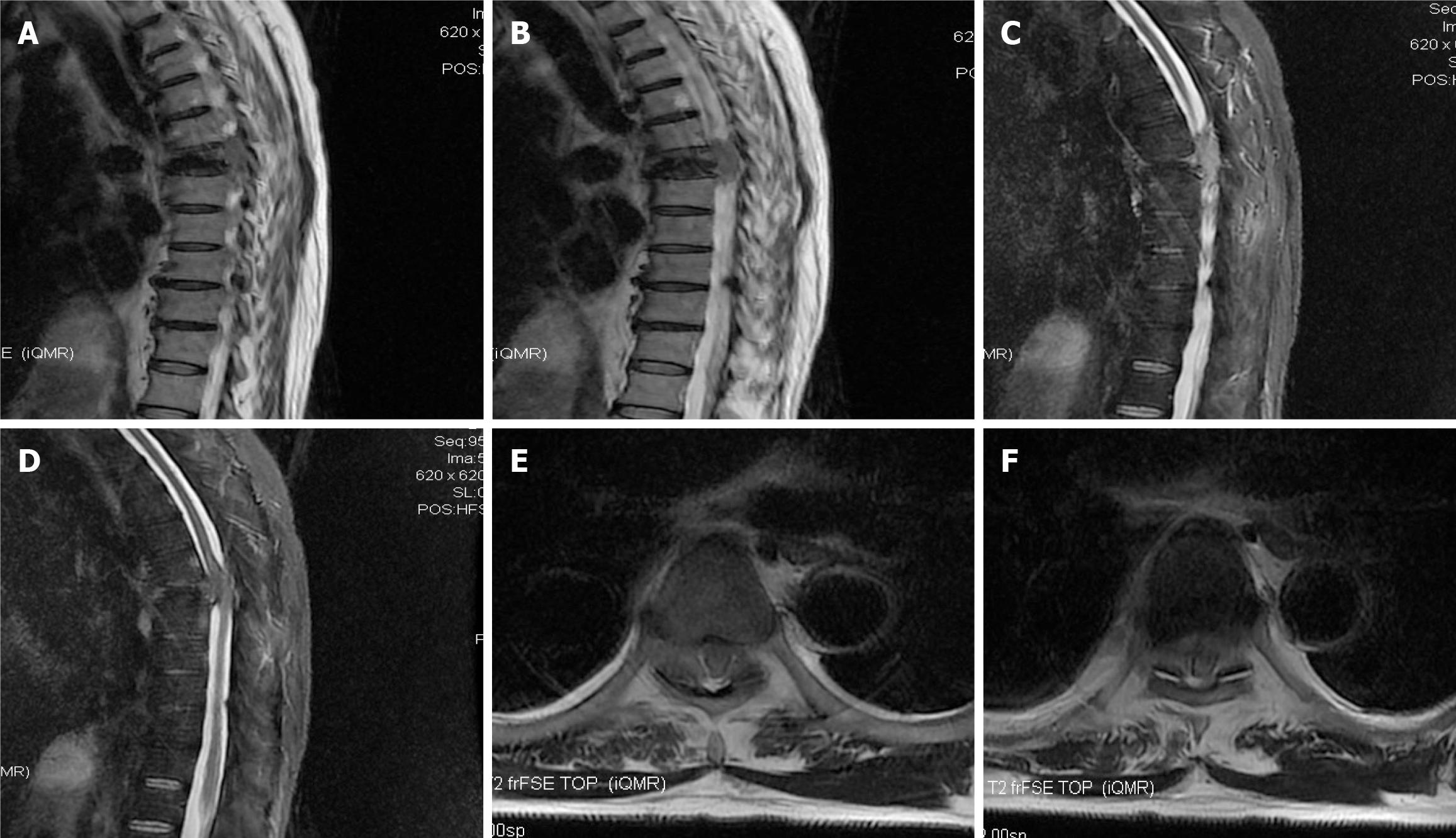
Three days after admission, the patient presented with lower abdominal pain, dysuria, loss of sensation below the T7 level, and immobility of both lower limbs. On September 19, 2023, T2-weighted magnetic resonance imaging (MRI) was conducted. The MRI revealed a wedge-shaped T7 vertebra, indicating spinal canal stenosis and spinal cord compression resulting from the protrusion of T7 vertebra cement into the spinal canal (Figure 2). Based on these abnormal findings, it was hypothesized that the patient’s paralysis symptoms were associated with the inadvertent leakage of cement into the spinal canal during the kyphoplasty procedure.
The patient was diagnosed with thoracic spinal cord injury and paraplegia of both lower limbs.
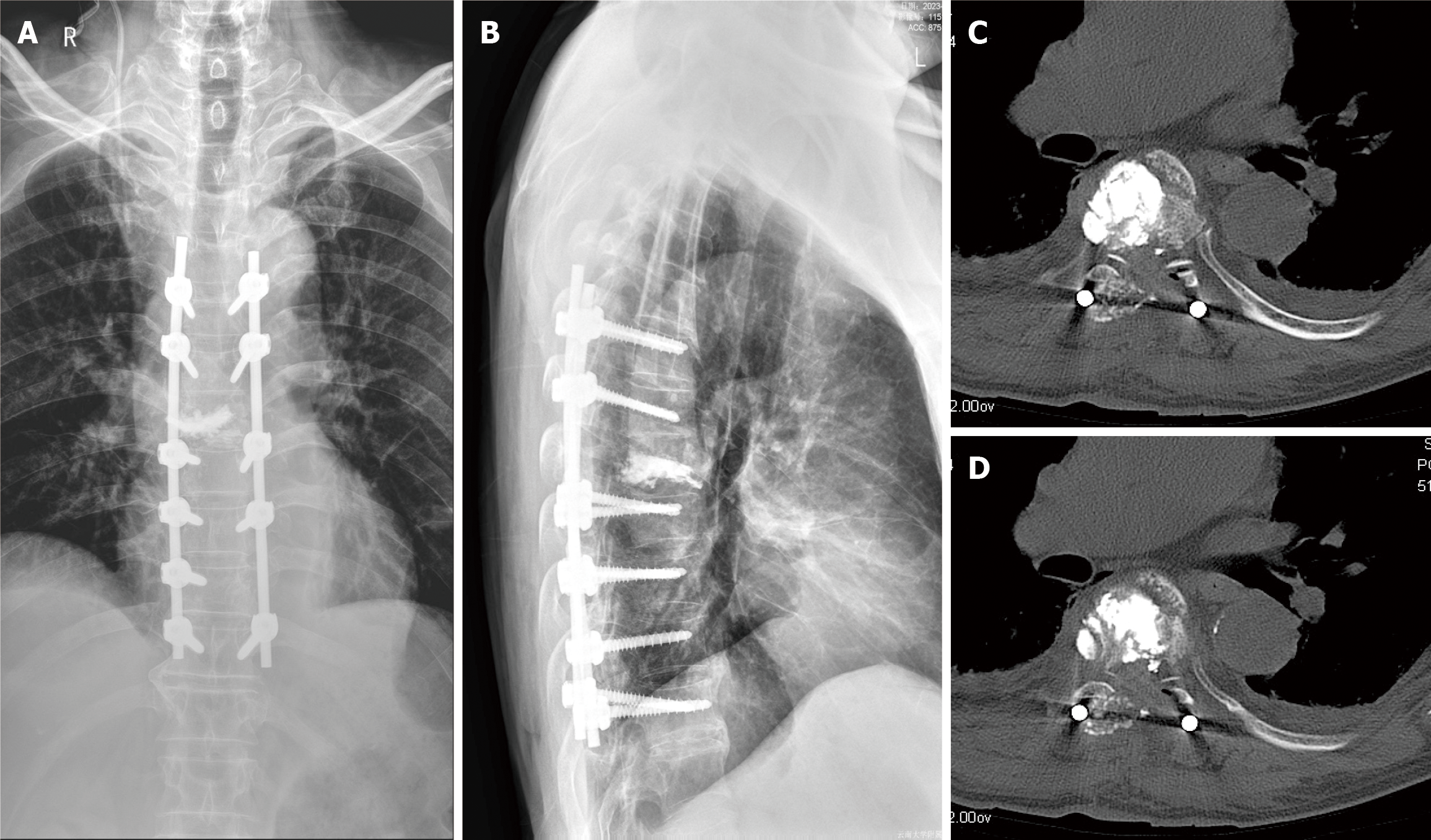
Urgent surgical interventions, including the incision and exploration of the spinal canal, posterolateral decompression, T7 subtotal vertebrectomy, and posterior instrumented spinal fusion (T5-T11), were performed on September 20, 2023 (Figure 3). During the operation, it was observed that cement had leaked into the dura within the spinal canal, compressing the spinal cord from the left side and causing contusions to both the spinal cord and nerve root. Post-surgery, the patient was promptly transferred to the intensive care unit (ICU) for vigilant postoperative monitoring. While in the ICU, the patient received standard treatment comprising routine mannitol and dexamethasone to mitigate spinal cord edema. Additionally, a preventative anti-infection regimen involving ceftriaxone was administered to reduce the risk of central nervous system infection.
The day after admission to the ICU, the patient was successfully weaned off the ventilator, and exhibited stability in both respiratory and circulatory systems. Subsequently, he was transferred to a regular ward. Over time, the patient experienced gradual improvement in muscle strength, sensation, and overall mobility, leading to a safe discharge one-week post-surgery. At the one-month follow-up, a diagnosis of pancreatic cancer was made at the local hospital. It was hypothesized that the T7 pathological compression fracture was associated with the presence of pancreatic cancer. Unfortunately, the patient opted to discontinue treatment, marking a regrettable conclusion to his medical care.
Currently, PKP is the preferred and optimal treatment for osteoporotic and pathological vertebral compression fractures, representing an innovative departure from traditional PVP. PKP offers distinct advantages by addressing kyphosis deformity, streamlining procedures to reduce operation time, utilizing an expandable balloon to restore vertebral height, and reinforcing the vertebra while minimizing cement leakage[5,6]. Notably, the reported rate of cement leakage exceeds 80% in PVP but remains below 50% in PKP[3,7]. Cement leakage into the perivertebral or intervertebral disc space generally manifests without significant clinical symptoms. However, when it occurs in the spinal canal or epidural space, it may lead to neurological symptoms or infections, while entry into the paraspinal venous system can result in embolism[8]. Research by Hulme et al[9] highlighted that cement leakage in PVP primarily occurs in the spinal canal and epidural region, whereas in PKP, it predominantly occurs in the perivertebral and intervertebral disc space. Several established risk factors for cement leakage include vertebral cortex fragmentation, defects in posterior vertebral walls, pathological compression fractures, high resistance in vertebrae (fracture compression greater than 2/3 or old fracture), a large volume of injected cement, low cement viscosity, low bone mineral density, intravertebral cleft, and Schmorl nodes[10-12]. While cement infiltration into the dura is a rare and serious complication, it has been reported in PVP cases. Herein, we present the first documented case of spinal cord injury, paraplegia, and cerebrospinal fluid leakage due to cement leakage into the intradural space after PKP.
As shown in previously published studies in the same field, the primary cause of dural rupture in this context is attributed to iatrogenic techniques. Specifically, the complication arises from repeated punctures and inaccurate needle angles during the procedure, leading to rupture of the pedicle or vertebral wall cortex and subsequent dural penetration. This sequence of events can result in cement extravasation into the intradural space following withdrawal of the puncture needle[13-16]. In the case of PKP, the recovery effect of the vertebral anterior margin, operative time, and improvement of postoperative low back pain VAS did not show a significant difference between unilateral and bilateral punctures. However, unilateral puncture demonstrated the advantage of a shorter operative time and reduced cement injection[17]. It is crucial to note that in the unilateral approach, an excessively large puncture angle may lead to damage to the medial wall of the pedicle. Therefore, during the procedure, the needle tip should not traverse the medial border of the pedicle on the anteroposterior view until it reaches the posterior cortex of the vertebral body on the lateral view[13-16].
To effectively prevent cement leakage, several key strategies based on summarized experiences have been identified. Firstly, comprehensive preoperative imaging, including computed tomography (CT) and MRI examinations, is imperative to fully understand the conditions of the injured vertebrae. Careful consideration and meticulous operation are particularly crucial for vertebral bodies with cortical damage. Intraoperatively, maintaining clear visualization of the cement is essential, as blurry images and blind punctures not only heighten the risk of cement leakage but also contribute to the inability to detect intraoperative leakage[18]. Secondly, the selection of cement with an appropriate viscosity is crucial. This, coupled with a strategy to reduce repeated punctures and avoid damaging the medial wall of the pedicle, allows for better control over the speed of cement injection[19]. Studies by Lu et al[20] have suggested that infusing a smaller dose (1.8-3 mL) of cement during PKP can achieve equivalent clinical effects to conventional doses (3.5-6 mL) while significantly reducing the incidence of cement leakage. Thirdly, precise control of the strength and depth of the screw tap and guide needle is essential to prevent rupture of the vertebral anterior cortex and subsequent cement extravasation. Implementation of these strategies collectively enhances the safety and efficacy of the PKP procedure[18-20].
Postoperative and meticulous CT scans play a pivotal role in accurately assessing cement leakage. For patients displaying intradural cement leakage and varying degrees of neurological deficits, prompt decompression surgery is imperative[13-16,21-24]. Literature reviews in this specific field indicate symptom improvement in the majority of patients, except one elderly patient who opted against open surgery[24]. Neurological deficits may arise from thermal injury resulting from the exothermic reaction at the posterior cortex of cement leakage in the spinal canal[25]. Early surgical intervention facilitates the removal of cement, reduces chronic inflammation and fibrosis on the cement surface, and prevents further damage to nerve tissue. In our case, the patient developed neurological symptoms, including urination disturbance and paraplegia, two weeks post-PKP. After confirming the precise location of cement leakage by MRI, immediate decompression surgery was performed. After the operation, the patient's muscle power gradually recovered. Our analysis suggests that the root cause of cement leakage in this patient may be attributed to the puncture technique employed by the surgeon.
In presenting this rare and distinctive case of intradural cement leakage following PKP, we emphasize the critical role of refining surgical techniques, conducting thorough preoperative evaluations, ensuring clear intraoperative visualization of the cement, and carefully selecting cement with appropriate viscosity and quantity to mitigate the risk of such complications. In the event of neurological deficits post-PKP, swift action is essential. Performing a prompt CT scan or MRI exploration is imperative to precisely identify the site of cement leakage, facilitating urgent surgical decompression. Our findings underscore the significance of a comprehensive approach to enhance procedural safety and address complications swiftly for improved neurological outcomes.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Orthopedics
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): 0
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Hassel B, Norway S-Editor: Liu JH L-Editor: A P-Editor: Zhao S
| 1. | Gosev I, Nascimben L, Huang PH, Mauri L, Steigner M, Mizuguchi A, Shah AM, Aranki SF. Right ventricular perforation and pulmonary embolism with polymethylmethacrylate cement after percutaneous kyphoplasty. Circulation. 2013;127:1251-1253. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 28] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 2. | Hu KZ, Chen SC, Xu L. Comparison of percutaneous balloon dilation kyphoplasty and percutaneous vertebroplasty in treatment for thoracolumbar vertebral compression fractures. Eur Rev Med Pharmacol Sci. 2018;22:96-102. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 15] [Reference Citation Analysis (0)] |
| 3. | Rose LD, Bateman G, Ahmed A. Clinical significance of cement leakage in kyphoplasty and vertebroplasty: a systematic review. Eur Spine J. 2023;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 6] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 4. | Ma QH, Liu GP, Sun Q, Li JG. Delayed complications of intradural cement leakage after percutaneous vertebroplasty: A case report. World J Clin Cases. 2022;10:8998-9003. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 1] [Cited by in RCA: 2] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 5. | Li Y, Jing Q, Chen F, Xu Y. Comparative Analysis of Therapeutic Outcomes and Prognoses Among Osteoporosis Patients with Varied Bone Mineral Density T-Values Following Percutaneous Kyphoplasty. Altern Ther Health Med. 2023;. [PubMed] |
| 6. | Alarkawi D, Bliuc D, Tran T, Ahmed LA, Emaus N, Bjørnerem A, Jørgensen L, Christoffersen T, Eisman JA, Center JR. Impact of osteoporotic fracture type and subsequent fracture on mortality: the Tromsø Study. Osteoporos Int. 2020;31:119-130. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 34] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 7. | Wang B, Zhao CP, Song LX, Zhu L. Balloon kyphoplasty versus percutaneous vertebroplasty for osteoporotic vertebral compression fracture: a meta-analysis and systematic review. J Orthop Surg Res. 2018;13:264. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 40] [Cited by in RCA: 85] [Article Influence: 12.1] [Reference Citation Analysis (0)] |
| 8. | Verlaan JJ, Oner FC, Dhert WJ. Anterior spinal column augmentation with injectable bone cements. Biomaterials. 2006;27:290-301. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 34] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 9. | Hulme PA, Krebs J, Ferguson SJ, Berlemann U. Vertebroplasty and kyphoplasty: a systematic review of 69 clinical studies. Spine (Phila Pa 1976). 2006;31:1983-2001. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 518] [Cited by in RCA: 493] [Article Influence: 25.9] [Reference Citation Analysis (0)] |
| 10. | Chen C, Fan P, Xie X, Wang Y. Risk Factors for Cement Leakage and Adjacent Vertebral Fractures in Kyphoplasty for Osteoporotic Vertebral Fractures. Clin Spine Surg. 2020;33:E251-E255. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 50] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 11. | Gao C, Zong M, Wang WT, Xu L, Cao D, Zou YF. Analysis of risk factors causing short-term cement leakages and long-term complications after percutaneous kyphoplasty for osteoporotic vertebral compression fractures. Acta Radiol. 2018;59:577-585. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 32] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 12. | Zhan Y, Jiang J, Liao H, Tan H, Yang K. Risk Factors for Cement Leakage After Vertebroplasty or Kyphoplasty: A Meta-Analysis of Published Evidence. World Neurosurg. 2017;101:633-642. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 81] [Cited by in RCA: 131] [Article Influence: 16.4] [Reference Citation Analysis (0)] |
| 13. | Bhide RP, Barman A, Varghese SM, Chatterjee A, Mammen S, George J, Thomas R. A rare presentation of subacute progressive ascending myelopathy secondary to cement leakage in percutaneous vertebroplasty. Am J Phys Med Rehabil. 2014;93:431-436. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 14. | Chen CH, Chuang MT, Wang CK. Intradural cement leakage after vertebroplasty. Spine J. 2015;15:1493-1494. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 15. | Baek IH, Park HY, Kim KW, Jang TY, Lee JS. Paraplegia due to intradural cement leakage after vertebroplasty: a case report and literature review. BMC Musculoskelet Disord. 2021;22:741. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 9] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 16. | Grelat M, Le Van T, Fahed E, Beaurain J, Madkouri R. Rare Complication of Percutaneous Technique: Intradural Cement Leakage and Its Surgical Treatment. World Neurosurg. 2018;118:97. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 17. | Qiao Y, Wang X, Liu Y, Hu J, Yuan FH, Zhao ZG. Comparison of Unilateral and Bilateral Percutaneous Kyphoplasty for Osteoporotic Vertebral Compression Fractures. J Pain Res. 2023;16:1813-1823. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 9] [Reference Citation Analysis (0)] |
| 18. | Potet J, Weber-Donat G, Curis E, Arnaud FX, Thome A, Valbousquet L, Peroux E, Geffroy Y, Bouzad C, Kervella Y, Lahutte M, Ukkola-Pons E, Baccialone J, Teriitehau CA. Incidence of pulmonary cement embolism after real-time CT fluoroscopy-guided vertebroplasty. J Vasc Interv Radiol. 2013;24:1853-1860. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 15] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 19. | Habib M, Serhan H, Marchek C, Baroud G. Cement leakage and filling pattern study of low viscous vertebroplastic versus high viscous confidence cement. SAS J. 2010;4:26-33. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 16] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 20. | Lu LM, Ni XH, Ni JP, Tan W, Zhu XY, Yin S, Wu JS, Xu FC, Zhao QM. Clinical effect of unilateral balloon infusion of low dose bone cement in PKP for osteoporotic thoracolumbar compression fractures in the elderly. Eur Rev Med Pharmacol Sci. 2022;26:3642-3647. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 21. | Sabuncuoğlu H, Dinçer D, Güçlü B, Erdoğan E, Hatipoğlu HG, Ozdoğan S, Timurkaynak E. Intradural cement leakage: a rare complication of percutaneous vertebroplasty. Acta Neurochir (Wien). 2008;150:811-815. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 30] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 22. | Teng MM, Cheng H, Ho DM, Chang CY. Intraspinal leakage of bone cement after vertebroplasty: a report of 3 cases. AJNR Am J Neuroradiol. 2006;27:224-229. [PubMed] |
| 23. | Shapiro S, Abel T, Purvines S. Surgical removal of epidural and intradural polymethylmethacrylate extravasation complicating percutaneous vertebroplasty for an osteoporotic lumbar compression fracture. Case report. J Neurosurg. 2003;98:90-92. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 37] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 24. | Chen YJ, Tan TS, Chen WH, Chen CC, Lee TS. Intradural cement leakage: a devastatingly rare complication of vertebroplasty. Spine (Phila Pa 1976). 2006;31:E379-E382. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 61] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 25. | Lai PL, Tai CL, Chen LH, Nien NY. Cement leakage causes potential thermal injury in vertebroplasty. BMC Musculoskelet Disord. 2011;12:116. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 27] [Cited by in RCA: 37] [Article Influence: 2.6] [Reference Citation Analysis (0)] |