Published online Jan 6, 2024. doi: 10.12998/wjcc.v12.i1.217
Peer-review started: October 30, 2023
First decision: November 21, 2023
Revised: November 30, 2023
Accepted: December 19, 2023
Article in press: December 19, 2023
Published online: January 6, 2024
Processing time: 63 Days and 15.9 Hours
Addison’s disease (AD) is a rare but potentially fatal disease in Western countries, which can easily be misdiagnosed at an early stage. Severe adrenal tuberculosis (TB) may lead to depression in patients.
We report a case of primary adrenal insufficiency secondary to adrenal TB with TB in the lungs and skin in a 48-year-old woman. The patient was misdiagnosed with depression because of her depressed mood. She had hyperpigmentation of the skin, nails, mouth, and lips. The final diagnosis was adrenal TB that resulted in the insufficient secretion of adrenocortical hormone. Adrenocortical hormone test, skin biopsy, T cell spot test of TB, and adrenal computed tomography scan were used to confirm the diagnosis. The patient’s condition improved after hormone replacement therapy and TB treatment.
Given the current status of TB in high-burden countries, outpatient doctors should be aware of and pay attention to TB and understand the early symptoms of AD.
Core Tip: Symptoms of early-onset depressed mood and skin pigmentation in developing countries warrant consideration for Addison’s disease (AD) induced by adrenal tuberculosis (TB) Diagnostic anti-TB therapy with rifampicin is not recommended because of the risk of adrenal crisis; T cell spot test of TB negativity cannot be used as a criterion to exclude TB, especially in immunocompromised patients or those with hematogenous disseminated pulmonary TB; In AD caused by adrenal TB, recovering adrenal function is difficult, with most cases requiring lifelong hormone replacement therapy.
- Citation: Zhang TX, Xu HY, Ma W, Zheng JB. Addison's disease caused by adrenal tuberculosis may lead to misdiagnosis of major depressive disorder: A case report. World J Clin Cases 2024; 12(1): 217-223
- URL: https://www.wjgnet.com/2307-8960/full/v12/i1/217.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i1.217
Primary adrenal insufficiency or Addison’s disease (AD) is characterized by damage to the adrenal gland, resulting in the insufficient production of cortisol, aldosterone, and sex hormones. AD is a rare disease with an incidence of 4:1000000 cases per year in Western countries and has fatal consequences[1]. This disorder can lead to depressed mood and depression[2].
Autoimmune adrenalitis is the leading cause of AD in developed countries, whereas in developing countries, adrenal tuberculosis (TB) remains an important cause of morbidity. The nonspecific symptoms of AD and the low frequency of non-TB epidemic countries often lead to neglect or delay in diagnosing the disease. Less experience in diagnosis has been noted for nonrelated professional doctors, resulting in a higher frequency of misdiagnosis in recent years[3].
A 48-year-old woman was admitted to Shaanxi TB Hospital with the chief complaint of skin pigmentation for 1 year.
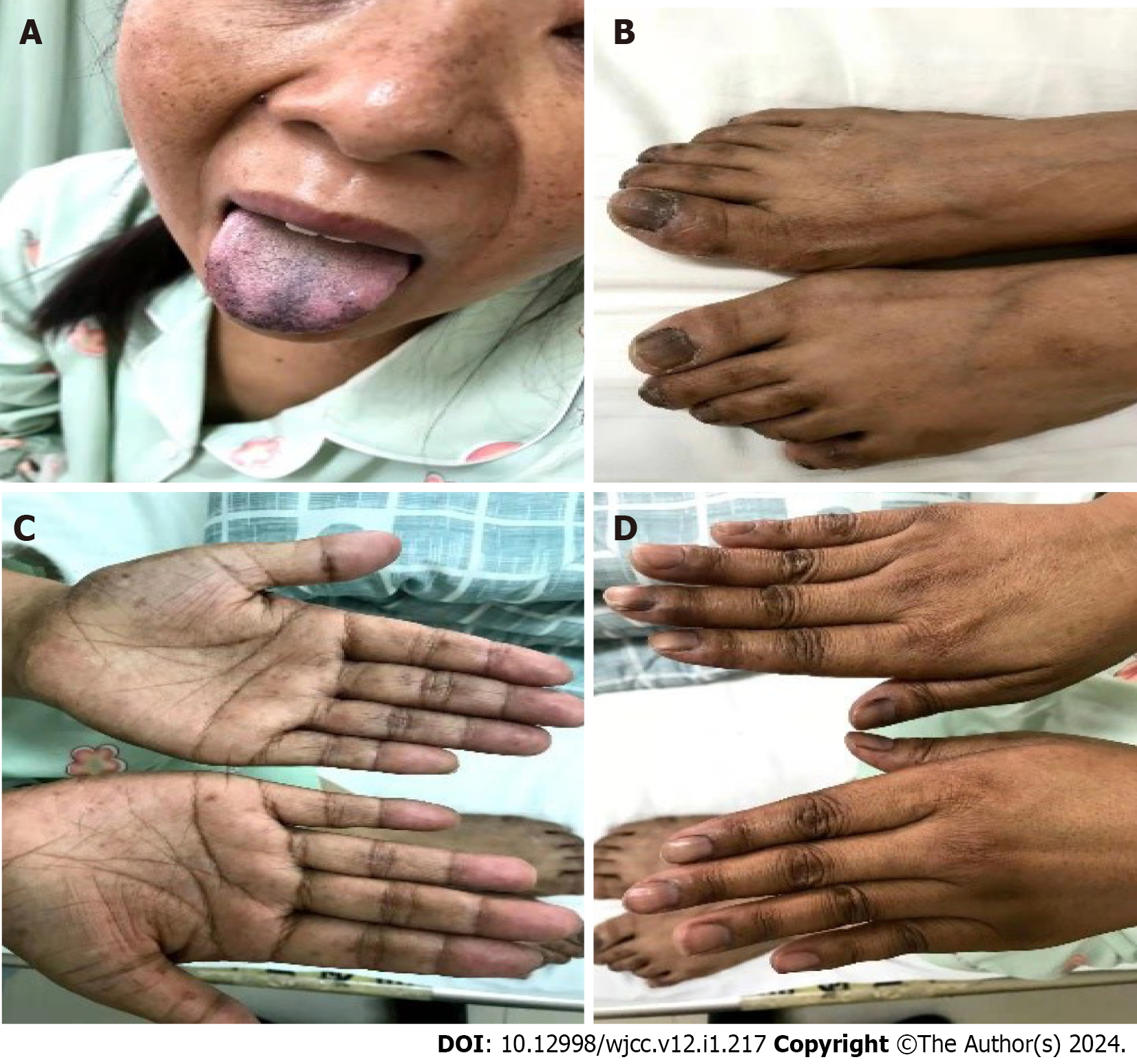
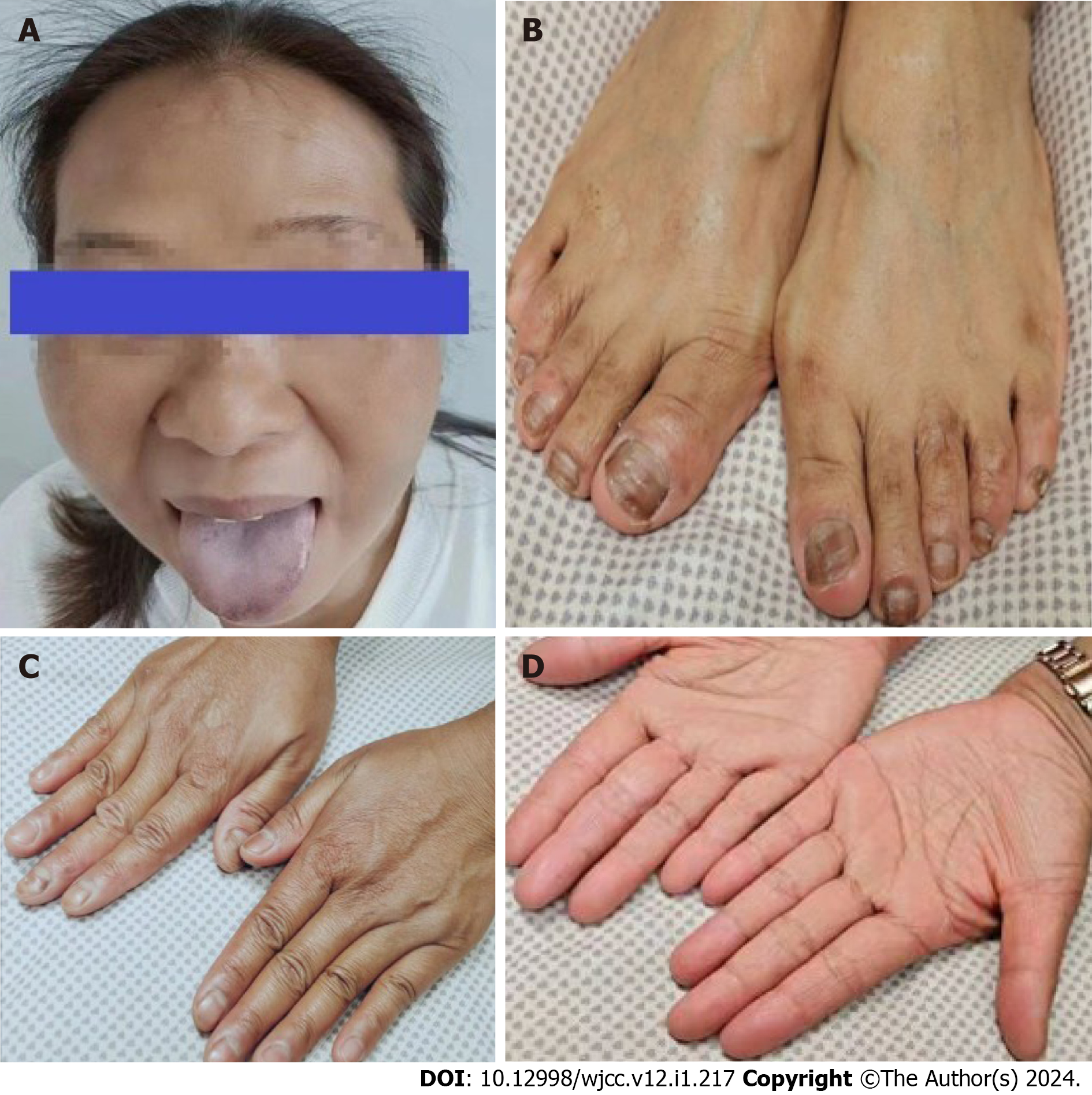
The patient experienced depressed mood, fatigue, decreased appetite, and hyperpigmentation of the skin, nails, mouth, and mucous membranes of the lips (Figure 1), which started 1 year prior to the consultation.
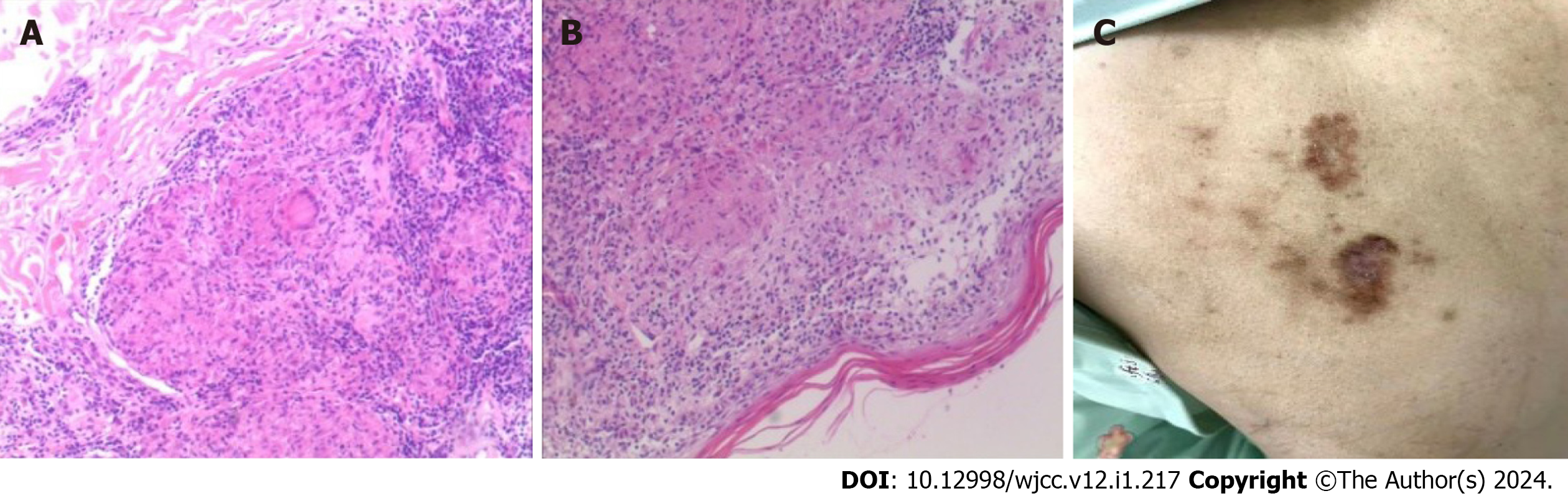
The patient experienced skin pigmentation for 1 year. She was also diagnosed with depression according to ICD-10 at other hospitals and was prescribed duloxetine hydrochloride 60 mg once daily and clonazepam 0.25 mg once daily. However, her depressive symptoms did not improve after 1 mo of treatment. She presented with a skin ulcer on her back, and pathological biopsy of the dorsal skin lesions showed hyperkeratosis and tuberculoid granulomatous inflammation (Figure 2A and B).
The patient denied having any genetic and she did not have a history of smoking or pulmonary TB.
On physical examination, the vital signs were as follows: Body temperature of 37.4 ℃, blood pressure of 63/40 mmHg, heart rate of 114 bpm, and respiratory rate of 21 breaths per min. There was hyperpigmentation of the skin, nails, mouth, and mucous membranes of the lips, which persisted after pressing and wiping. Two skin lesions were found on the left back, with no secretions (Figure 2C).
Laboratory tests showed elevated inflammatory parameters (erythrocyte sedimentation rate: 42 mm/h, C-reactive protein: 52.2 mg/L, and procalcitonin: 0.65 ng/mL). The patient also had hyperkalemia (5.6 mmol/L), hyponatremia (111.8 mmol/L), and hypochloremia (81.1 mmol/L). Persistent hypotension (80/40 mmHg) was observed. T cell spot test of TB (T-SPOT.TB) was positive.
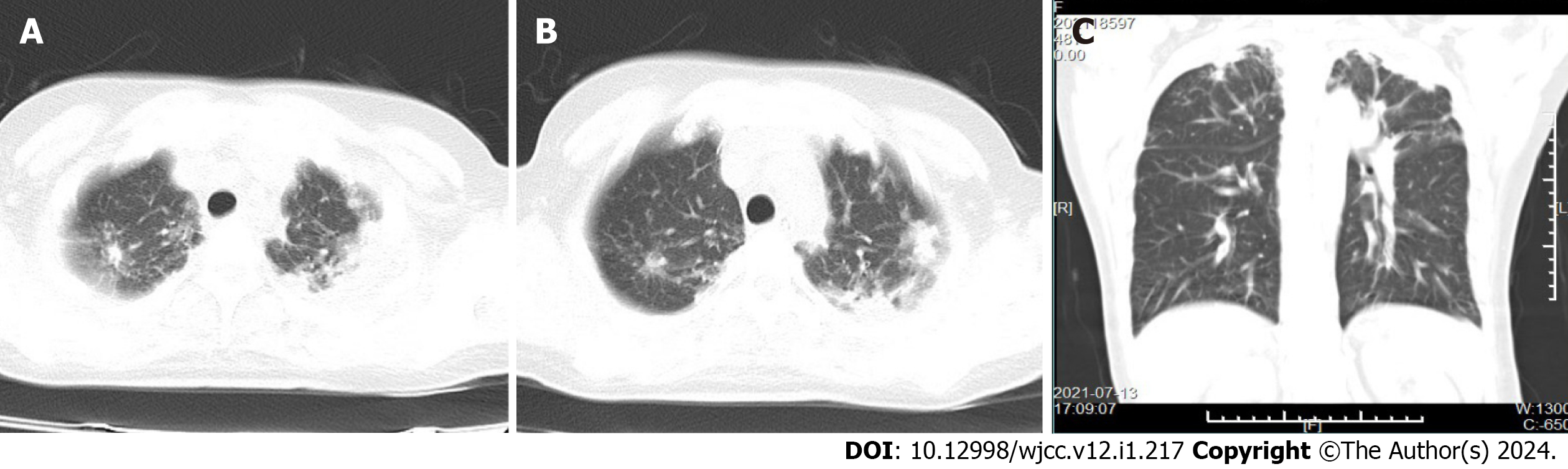
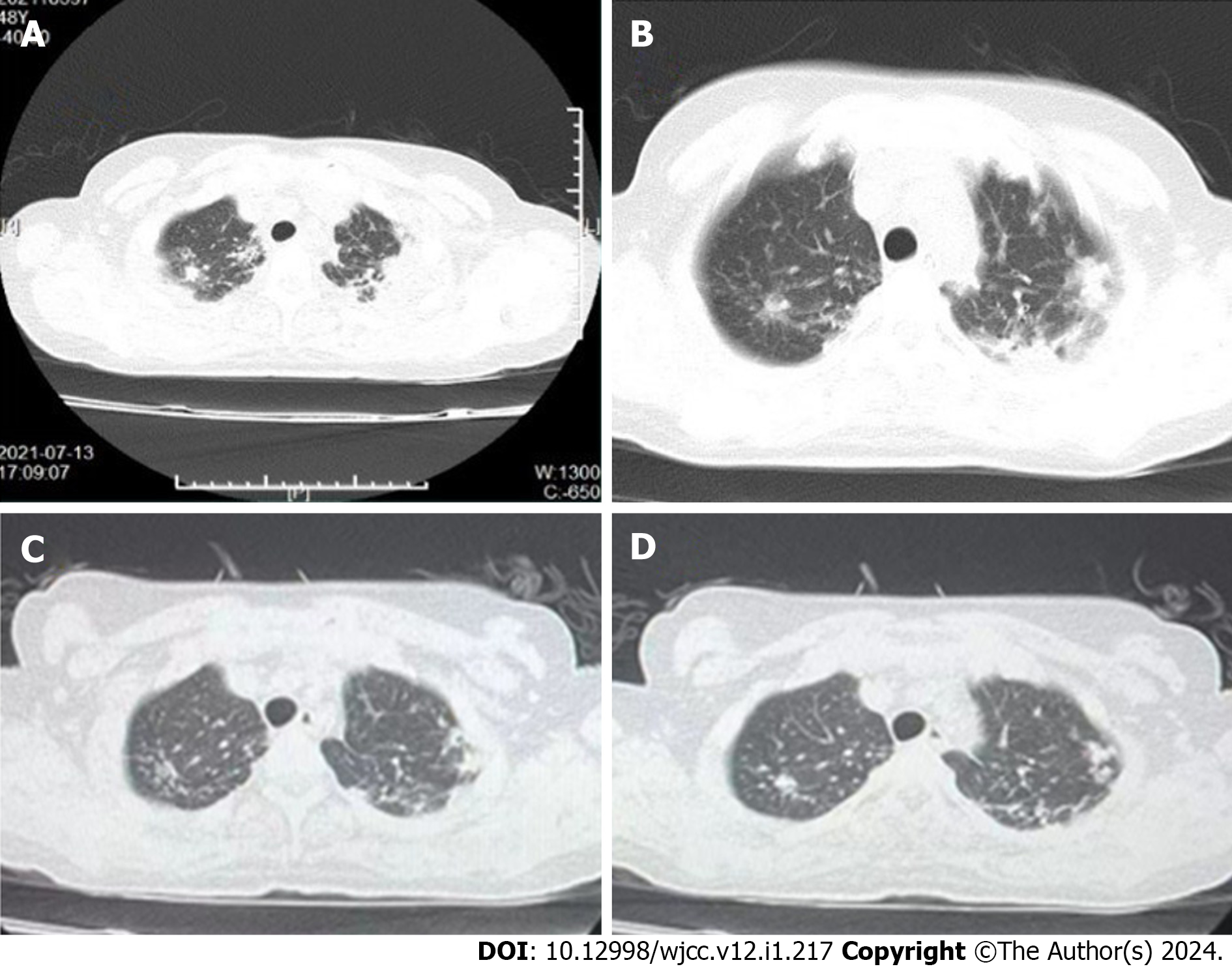
Chest computed tomography (CT) revealed infectious lesions in both lungs (Figure 3). Fiberoptic bronchoscopy was recommended, but the patient did not consent.
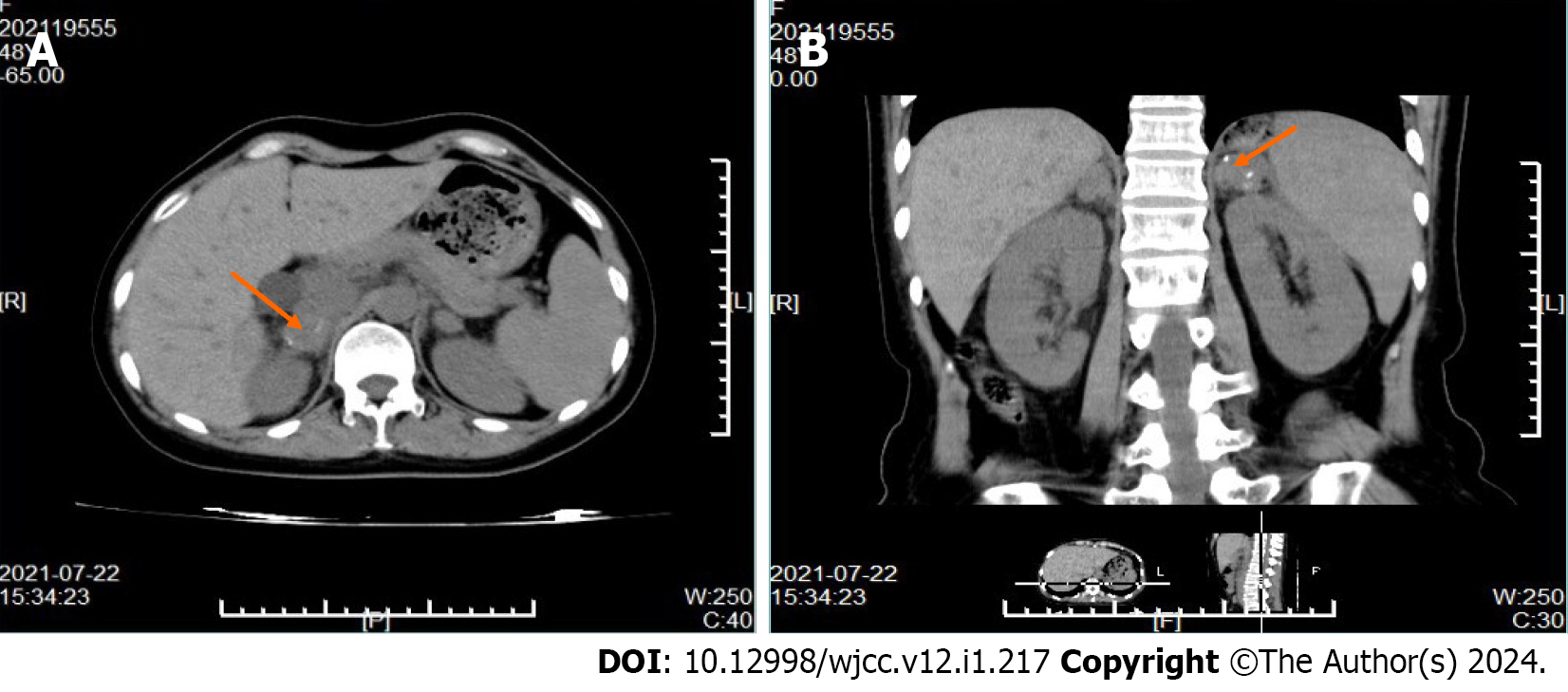
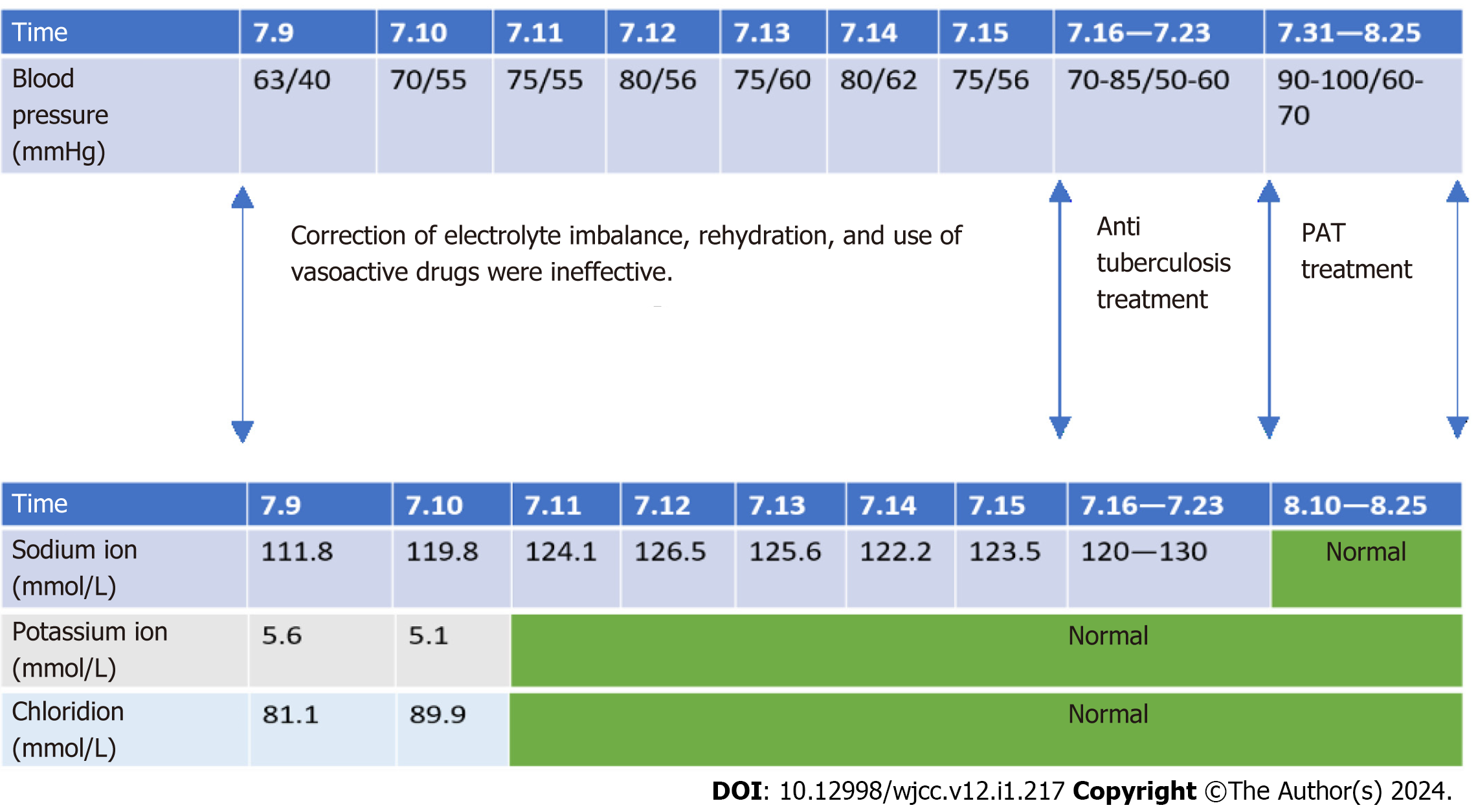
Refractory hyperkalemia and hyponatremia alongside persistent hypotension of 80/40 mmHg were observed. The patient’s condition did not improve despite electrolyte correction, rehydration, and use of vasoactive drugs. Thus, adrenal hormone secretion deficiency was considered based on her symptoms and laboratory tests. Further workup revealed cortisol < 1.31 μg/dL and adrenocorticotropic hormone (ACTH) > 2000 pg/mL. Adrenal CT revealed bilateral calcification and giant masses in the adrenal glands (Figure 4).
The final diagnosis was AD secondary to adrenal TB.
The treatment protocol was as follows: Prednisone (PAT) 5 mg once daily at 8 am, isoniazid 0.3 g once daily, rifampicin 0.6 g once daily, pyrazinamide 0.5 g thrice daily, and ethambutol hydrochloride 1.0 g once daily. During the combined treatment of PAT plus anti-TB therapy, the patient had no adverse drug reactions.
After 2 wk of combined treatment, there was significant improvement in depressive symptoms, and her blood pressure and serum electrolyte levels normalized (Figure 5). After 1 mo of combined treatment, chest CT showed improvement in inflammation (Figure 6), and after 6 mo, the patient’s pigmentation improved (Figure 7).
At present, the prevention and treatment of TB remains grim. In 2020, approximately 1.5 million deaths worldwide were attributable to TB, with a TB case fatality rate of 15% (up from 14% in 2019). The number of TB deaths among human immunodeficiency virus-negative patients increased from 1.21 million to 1.28 million in 2019[4]. Primary adrenal insufficiency was discovered by Addison et al[5] in 1855. When he first described adrenocortical insufficiency in his patients, 6 of 11 cases were caused by the destruction of the adrenal cortex by Mycobacterium tuberculosis[6]. In 1930, Guttman et al[7] reported 566 patients with AD, of whom 70% had AD caused by tuberculous adrenalitis. By 1956, the number decreased to 25%. A meta-analysis performed by Italian scholars in 2011 showed a decrease in the incidence of adrenal failure secondary to tuberculous in 615 patients with AD. Only 9% of the cases were caused by TB[8]. TB is no longer the most common cause of AD in developed countries. Recent data suggest that this trend continues, with an increasing prevalence of AD, particularly in women[9]. Today, in Western societies, 80% of AD cases are caused by autoimmune adrenalitis, followed by TB or other infectious and malignant diseases in approximately 10% the cases. However, the most common cause of AD in developing countries remains infection with M. tuberculosis, which spreads to the adrenal glands via the bloodstream[6]. The current treatment is hormone therapy, with most patients requiring lifelong replacement therapy. Hydrocortisone is the drug of choice for glucocorticoid replacement, but 3-5 mg/dL prednisolone as a single dose or in two divided oral doses is an alternative.
Many patients have no obvious early symptoms. Alterations in sleep habits, mood, and behavior can sometimes be the first symptoms. Severely ill patients seek medical attention owing to fatal adrenal crisis. AD becomes apparent only when > 90% of the adrenal glands are destroyed by TB. Most active or recently active (< 2 years) patients with TB have bilateral adrenal enlargement, calcifications, and atrophy that is typical of longstanding infections caused by TB[10].
In our case, AD was misdiagnosed as depression in the outpatient clinic of the patient due to long-term skin pigmentation. At the time of admission to our hospital, her chest CT showed manifestations of a pulmonary infection, and skin biopsy revealed a pathological diagnosis of TB granuloma. The adrenal gland CT showed enlargement and calcification. Given the signs and symptoms of this patient and the high suspicion for tuberculous adrenalitis, cortisol and ACTH were tested, which resulted in the diagnosis of AD secondary to adrenal TB. After 1 mo of anti-TB and hormone replacement therapy, chest CT showed improvement in inflammation. After 6 mo, the pigmentation was partially reversed.
This report aimed to show our experience in the diagnosis and treatment of AD. First, it was important that the physician made the correct diagnosis in the outpatient clinic at an early stage. AD involves multiple organs, including the brain. This patient was diagnosed with depression at another hospital, and the signs of skin hyperpigmentation, hypotension, and electrolyte disorder were ignored. Thus, AD should be considered when multiple mucosal hyperpigmentation and depression are observed in countries with a high burden of TB. Second, reversal of hormone secretion changes in AD induced by adrenal TB is extremely difficult even after long-term anti-TB treatment. Most patients require lifelong hormone replacement therapy. Additionally, we do not recommend diagnostic anti-TB therapy as a diagnostic measure because it is also worth noting that rifampicin has the potential to cause adrenal crisis. This can interfere with the diagnosis of AD and should be carefully differentiated[11]. Third, T-SPOT.TB positivity can be used as a reference indicator for TB infection, but T-SPOT.TB negativity cannot be used as a basis for excluding the infection, especially in immunocompromised patients or those with hematogenous disseminated pulmonary TB[12]. In terms of treatment, once AD induced by adrenal TB is diagnosed, lifelong hormone replacement therapy and a course of anti-TB treatment are required. In summary, AD symptoms caused by TB are insidious and easily misdiagnosed in the early stage.
Given the current status of TB in high-burden countries, outpatient doctors should pay attention to the early symptoms of AD and consider the possibility of TB infection. In addition, recovery of adrenal function after AD caused by adrenal TB is difficult, and most cases require lifelong hormone replacement therapy.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Pavón L, Mexico S-Editor: Qu XL L-Editor: A P-Editor: Zhang YL
| 1. | Puar TH, Stikkelbroeck NM, Smans LC, Zelissen PM, Hermus AR. Adrenal Crisis: Still a Deadly Event in the 21st Century. Am J Med. 2016;129:339.e1-339.e9. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 95] [Cited by in RCA: 107] [Article Influence: 11.9] [Reference Citation Analysis (0)] |
| 2. | van Haren Noman S, Visser H, Muller AF, Limonard GJ. Addison's Disease Caused by Tuberculosis: Diagnostic and Therapeutic Difficulties. Eur J Case Rep Intern Med. 2018;5:000911. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 3. | Rowińska-Zakrzewska E, Szopiński J, Remiszewski P, Szymańska D, Miller M, Pawlicka L, Zwolska-Kwiek Z. Tuberculosis in the autopsy material: analysis of 1500 autopsies performed between 1972 and 1991 in the Institute of Tuberculosis and Chest Diseases, Warsaw, Poland. Tuber Lung Dis. 1995;76:349-354. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 14] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 4. | World Health Organization. Global tuberculosis report 2021. Oct 14, 2021. [cited 31 January 2022]. Available from: https://www.who.int/publications/i/item/9789240037021. |
| 5. | On the Constitutional and Local Effects of Disease of the Supra-Renal Capsules. Br Foreign Med Chir Rev. 1856;18:404-413. [PubMed] |
| 6. | Jacob JJ, Paul PAM. Infections in Endocrinology: Tuberculosis. 2021 Mar 14. In: Endotext [Internet]. South Dartmouth (MA): MDText.com, Inc.; 2000–. [PubMed] |
| 7. | Guttman P, Guttman PH, Guttman P. Addison's disease-a statistical analysis of 566 cases and a study of the pathology. Arch Pathol. 1930;10:742-935. |
| 8. | Betterle C, Morlin L. Autoimmune Addison's disease. Endocr Dev. 2011;20:161-172. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 60] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 9. | Meyer G, Neumann K, Badenhoop K, Linder R. Increasing prevalence of Addison's disease in German females: health insurance data 2008-2012. Eur J Endocrinol. 2014;170:367-373. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 45] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 10. | Gupta S, Ansari MAM, Gupta AK, Chaudhary P, Bansal LK. Current Approach for Diagnosis and Treatment of Adrenal Tuberculosis-Our Experience and Review of Literature. Surg J (N Y). 2022;8:e92-e97. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 11. | Yokoyama T, Toda R, Kimura Y, Mikagi M, Aizawa H. Addison's disease induced by miliary tuberculosis and the administration of rifampicin. Intern Med. 2009;48:1297-1300. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 12] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 12. | Whitworth HS, Badhan A, Boakye AA, Takwoingi Y, Rees-Roberts M, Partlett C, Lambie H, Innes J, Cooke G, Lipman M, Conlon C, Macallan D, Chua F, Post FA, Wiselka M, Woltmann G, Deeks JJ, Kon OM, Lalvani A; Interferon-γ Release Assays for Diagnostic Evaluation of Active Tuberculosis study group. Clinical utility of existing and second-generation interferon-γ release assays for diagnostic evaluation of tuberculosis: an observational cohort study. Lancet Infect Dis. 2019;19:193-202. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 43] [Article Influence: 7.2] [Reference Citation Analysis (0)] |