Published online Jan 6, 2024. doi: 10.12998/wjcc.v12.i1.142
Peer-review started: August 28, 2023
First decision: November 20, 2023
Revised: December 3, 2023
Accepted: December 14, 2023
Article in press: December 14, 2023
Published online: January 6, 2024
Processing time: 127 Days and 4.8 Hours
Congestive ischemic colitis is a rare subtype of ischemic colitis with an unknown pathophysiology. Excluding conservative management, such as fasting, no established treatment exists; therefore, surgical intervention should be considered in some cases if symptoms worsen. Current literature suggests that anti-inflammatory agents may effectively treat congestive ischemic colitis.
We present the case of a 68-year-old female patient who underwent laparoscopic left hemicolectomy for transverse colon cancer 3 years ago. Postoperatively, follow-up included an annual colonoscopy and abdominal computed tomography (CT) at a local clinic. However, progressive erythema and edema of the sigmoid colon were observed 1 year postoperatively. Upon admission to our hospital, she complained of abdominal pain and diarrhea. Abdominal CT showed thickening of the sigmoid colon walls, and colonoscopy revealed erythema, edema, and multiple ulcers with exudate in the sigmoid colon. CT angiography showed engorgement of the sigmoid vasa recta without any vascular abnormalities. The diagnosis was congestive ischemic colitis, and we treated the patient with anti-inflammatory agents. After 2 mo of glucocorticoid therapy (20 mg once daily) and 7 mo of 5-aminosalicylate therapy (1 g twice daily), the ulcers completely healed. She has not experienced any recurrence for 2 years.
Anti-inflammatory therapy, specifically glucocorticoids and 5-aminosalicylate, has demonstrated promising efficacy and introduces potential novel treatment options for congestive ischemic colitis.
Core Tip: Congestive ischemic colitis is a rare type of ischemic colitis whose diagnosis requires a comprehensive assessment. Since no clear treatment guidelines exist, surgical treatment should be considered if symptoms worsen during bowel rest. We report, for the first time, the successful treatment of congestive ischemic colitis occurring after left hemicolectomy with glucocorticoids and 5-aminosalicylate. Follow-up revealed complete healing of the sigmoid ulcers without recurrences in the past 2 years.
- Citation: Lee GW, Park SB. Congestive ischemic colitis successfully treated with anti-inflammatory therapy: A case report. World J Clin Cases 2024; 12(1): 142-147
- URL: https://www.wjgnet.com/2307-8960/full/v12/i1/142.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i1.142
Ischemic colitis involves mucosal inflammation and ulcers, occurring when blood flow to the colon is reduced to a level insufficient for maintaining cellular metabolic function[1,2]. Various causes of ischemia exist, including vascular factors, such as atherosclerosis or thrombus formation; intestinal factors that increase intestinal pressure, such as constipation; and congestion-related factors caused by venous return dysfunction[2-4]. Congestive ischemic colitis, which is a rare type of ischemic colitis, has no clear pathophysiology or consensus for optimal treatment. The condition is typically treated with conservative management, such as fasting, although surgical intervention should be considered if symptoms worsen. However, recent reports suggest that anti-inflammatory agents may be effective in treating congestive ischemic colitis.
Here, we present an uncommon case of congestive ischemic colitis caused by inadequate venous return after left hemicolectomy. Conservative treatment and antibiotics were ineffective, and surgical treatment was considered; however, the patient was successfully treated with anti-inflammatory agents, namely, glucocorticoids and 5-aminosalicylate, without the need for additional surgery.
A 68-year-old female patient visited our hospital with abdominal pain and diarrhea.
The patient had experienced persistent abdominal pain and diarrhea over the past month, compelling her to visit a local clinic. After undergoing a colonoscopy and abdominal computed tomography (CT), infectious colitis was suspected. Accordingly, the patient was treated with antibiotics. However, the symptoms did not improve, and she was subsequently referred to our hospital.
The patient had hypertension and type 2 diabetes. Three years ago, she underwent extended cholecystectomy for gallbladder cancer and laparoscopic left hemicolectomy with low ligation of the inferior mesenteric artery (IMA) (IMA preservation and left colic artery ligation) and inferior mesenteric vein (IMV) ligation for transverse colon cancer. Postsurgical follow-up included an annual colonoscopy and abdominal CT at a local clinic. However, progressive erythema and edema were observed below the anastomosis site in the sigmoid colon 1 year postoperatively.
The patient had no family history of gastrointestinal disease or tumors.
Abdominal examination revealed tenderness around the umbilicus and lower abdomen.
Peripheral blood tests showed a white blood cell count of 1.06 × 109/L (neutrophils, 83%), hemoglobin level of 12.3 g/dL, and platelet count of 3.24 × 109/L. Serum biochemistry tests indicated normal levels of total bilirubin (0.7 mg/dL), aspartate transaminase (14 IU/L), and alanine transaminase (9 IU/L) and an elevated C-reactive protein level (4.49 mg/dL). Stool culture, fecal Clostridium difficile toxin, and glutamate dehydrogenase tests were also negative.
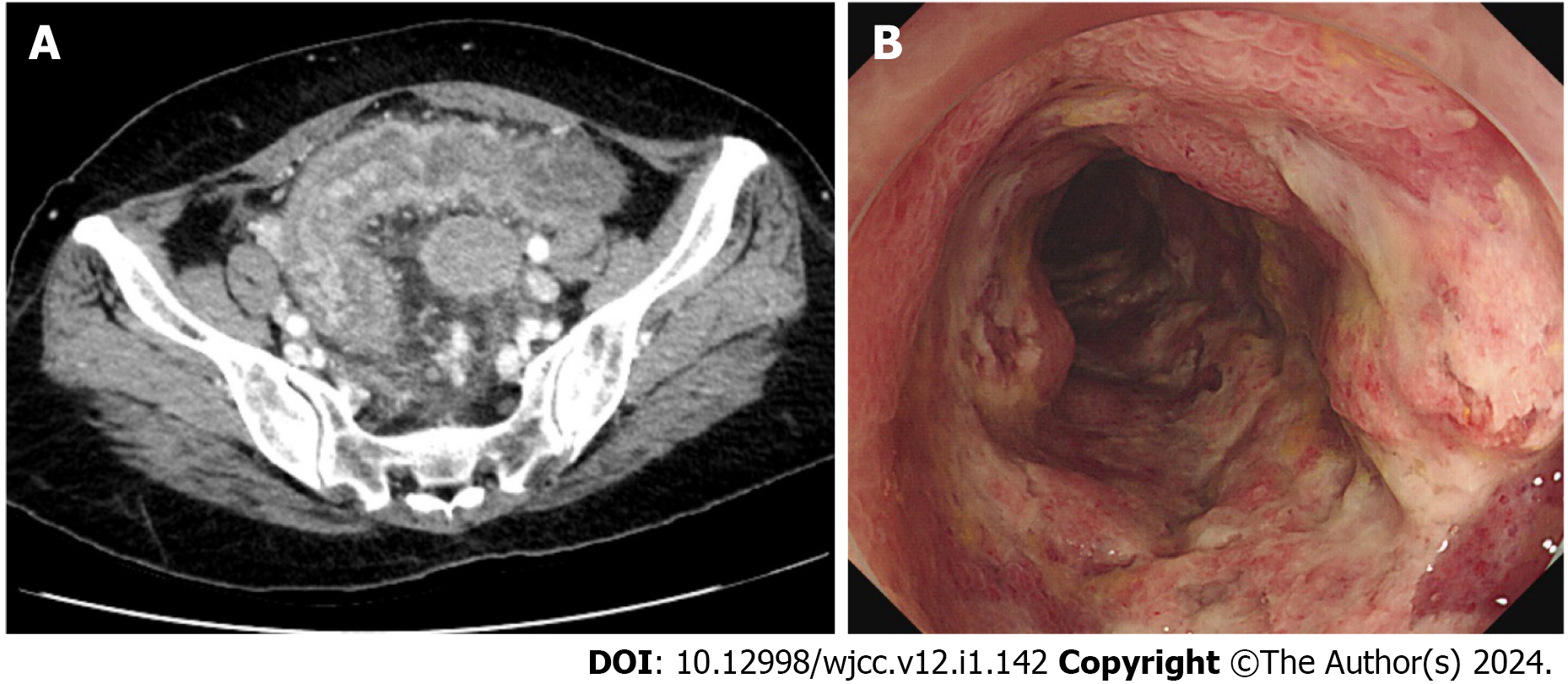
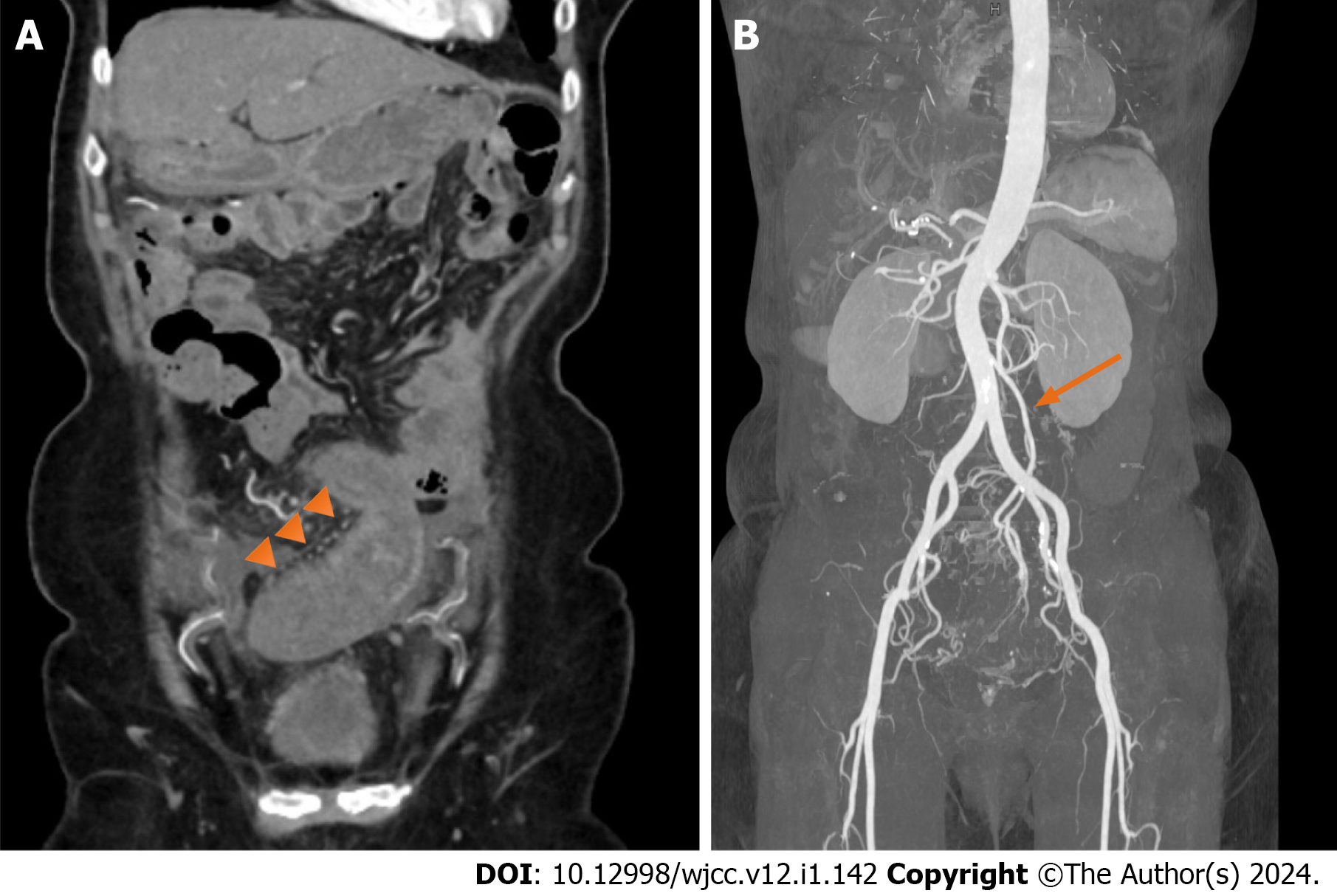
Abdominal CT revealed thickening of the sigmoid colon walls, abnormal attenuation of pericolic fat, and a small amount of ascites (Figure 1A). During the colonoscopy, an anastomosis site was observed 45 cm from the anus, while erythema and mucosal swelling were observed approximately 20–35 cm from the anus. Multiple ulcerations and erosions were also observed (Figure 1B). CT angiography showed diffuse wall thickening and fat infiltration in the sigmoid colon, extending from the anastomosis site to the distal portion of the sigmoid colon. Engorgement of the sigmoid vasa recta was also observed (Figure 2A). However, vascular abnormalities were not observed, and blood flow in the inferior mesenteric, sigmoid colic, and superior rectal arteries was preserved (Figure 2B).
Based on the patient's worsening medical history beginning 1 year after left hemicolectomy with IMA low ligation and IMV ligation and considering the abdominal CT, colonoscopy, and CT angiography findings, the final diagnosis was congestive ischemic colitis.
Conservative treatment, including fasting, high-calorie fluid administration, and antibiotic therapy, was administered. On day 8 of hospitalization, her abdominal pain and diarrhea significantly improved, and a liquid diet was commenced. However, abdominal pain and diarrhea recurred after starting the diet; therefore, fasting was resumed, and a sigmoidoscopy was performed. Sigmoidoscopy revealed active ulcers, severe erythema, and swelling in the sigmoid colon rather than in the rectum; severe mucosal injury was present due to ischemic damage. The patient’s condition did not improve despite conservative treatment. Therefore, we cautiously administered anti-inflammatory agents; if no improvements were observed, surgical intervention was planned. After starting 20 mg of prednisolone once daily and 1 g of 5-aminosalicylate twice daily, her abdominal pain and diarrhea rapidly improved. The patient was discharged on day 16 of hospitalization. At the outpatient clinic, she did not complain of any specific symptoms thereafter, and the steroid dose was discontinued after tapering over 2 mo; 5-aminosalicylate (1 g twice daily) was maintained.
Two months after discharge, a follow-up abdominal CT and colonoscopy were performed. Abdominal CT revealed improvements in the diffuse wall thickening of the sigmoid colon and the engorgement of the sigmoid vasa recta. Ascites was not observed. On colonoscopy, the exudate-covered ulcers, erythema, and swelling had improved but were still present. After maintaining 5-aminosalicylate 1 g twice daily for 7 mo, colonoscopy was repeated, and no abnormal findings were observed (Figure 3). Consequently, 5-aminosalicylate was discontinued, and no adverse effects from the anti-inflammatory agents occurred. The patient was happy to recover without surgical treatment and has remained symptom-free without medication for the past 2 years.
Congestive ischemic colitis is a rare type of ischemic colitis. Fuji et al[2] reported that congestive ischemic colitis occurred in 4 (2.1%) of the 191 patients following left-sided colectomy where the arterial branch (superior rectal artery) was preserved, and the IMV was cut near the root. Similarly, Suh et al[5] reported an incidence of 2.25% (3/133 patients). Congestive ischemic colitis is believed to be caused by venous congestion resulting from an imbalance between the arterial supply and venous return of the remnant colon after colectomy for left colon cancer[2,5]. The descending and sigmoid colons receive blood from the left colic, sigmoid, and superior rectal arteries, originating from the IMA. Venous drainage occurs through the left colic, sigmoid, and superior rectal veins, which ultimately drain into the IMV. Congestion can develop in the descending and sigmoid colons when the arterial blood supply is maintained and venous drainage through the IMV is disrupted due to IMV ligation at the inferior margin of the pancreas during surgery. In contrast, the rectum receives blood from the upper, middle, and lower rectal arteries and is drained by the upper, middle, and lower rectal veins; therefore, IMV ligation typically does not result in rectal congestion. Congestion is more likely to occur when the remnant distal colon is lengthy. Therefore, in that case, preserving the IMV during surgery might be considered to prevent venous congestion and subsequent congestive ischemic colitis[5].
The diagnosis of congestive ischemic colitis requires a comprehensive assessment, including the patient’s symptoms, medical history, and imaging examinations. Specifically, the patient’s medical history reveals characteristic symptoms, such as abdominal pain and diarrhea, occurring several months after undergoing a left-sided colectomy with low ligation of the IMA and IMV ligation[1,2,6]. Abdominal CT shows continuous bowel wall thickening below the anastomosis site, and the rectum is unaffected in most cases. CT angiography shows engorgement of the sigmoid vasa recta without any vascular abnormalities, including stenosis or obstruction[2,5]. Furthermore, colonoscopy reveals edema, erythema, and ulceration consistent with the findings of ischemic colitis[1,6].
The pathophysiology of congestive ischemic colitis may involve venous ischemia and subsequent reperfusion injury[3,7]. Ischemia leads to anaerobic metabolism, resulting in reduced adenosine triphosphate production and the impairment of cellular ion exchange channels. This results in cell swelling and impaired enzymatic activity in the cytoplasm. During the reperfusion state, reactive oxygen species cause oxidative stress and local inflammation, leading to endothelial dysfunction, DNA damage, and cell death[7]. Consequently, mucosal integrity may be compromised, leading to bacterial translocation and bacteremia[8].
Fasting is the most effective treatment for congestive ischemic colitis that reduces colonic oxygen demand, thereby alleviating the imbalance between arterial supply and venous return[2,9]. However, recovery may be protracted with bowel rest alone, and surgical intervention may be necessary in some severe cases. Kruis and Schiff[10] reported that combination therapy with intravenous antibiotics and prednisolone showed promising therapeutic effects without safety concerns in cases of moderate-to-severe ischemic colitis. Antimicrobial therapy can effectively reduce pathogenic bacteria, bacterial translocation, and inflammatory responses to ischemic injury[1,8]. Additionally, glucocorticoids can inhibit the activation, migration, and proliferation of immune cells in both the innate and adaptive immune systems, resulting in anti-inflammatory and immunoregulatory actions[11]. Although the American College of Gastroenterology does not recommend the use of glucocorticoids for treating ischemic colitis, limited use of therapeutic agents for inflammatory bowel disease, such as local or systemic glucocorticoids, sulfasalazine, and 5-aminosalicylate, may be considered in chronic ischemic colitis cases[1].
In this case, the patient had chronic and severe ischemic colitis. Therefore, we administered glucocorticoids and 5-aminosalicylate in addition to bowel rest and antimicrobial therapy. Because of concerns regarding the potentially harmful side effects of glucocorticoids, such as infection, hypertension, hyperglycemia, and Cushing’s syndrome, we administered a 2-mo course of a low dose of glucocorticoids (20 mg once daily) concurrently with 5-aminosalicylate (1 g twice daily). As an anti-inflammatory agent, 5-aminosalicylate exhibits a wide range of activities, such as inhibiting cell- and antibody-mediated immune processes and acting as a potent free radical scavenger and anti-oxidant. The beneficial effects of 5-aminosalicylate can be attributed to its ability to inhibit the activation of nuclear factor-kappa B (NF-κB)[12,13]. The activation of NF-κB is an important factor in inflammatory injury due to ischemia-reperfusion, and the inactivation of the NF-κB signaling pathway to control inflammation has been well studied[14-16]. Therefore, 5-aminosalicylate has been suggested to be beneficial in treating congestive ischemic colitis.
No consensus currently exists on an effective treatment strategy for congestive ischemic colitis. Management of this condition has been challenging because of its complex pathophysiology and lack of specific therapeutic options. However, as reported in this case, the use of anti-inflammatory agents, such as glucocorticoids and 5-aminosalicylate, shows promise and may lead to novel effective therapies. Therefore, further research and clinical trials are necessary to validate and optimize the efficacy and safety of these treatment options for congestive ischemic colitis.
The authors would like to thank the patient for participating in this study.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: South Korea
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Sano W, Japan S-Editor: Lin C L-Editor: Wang TQ P-Editor: Zhang YL
| 1. | Brandt LJ, Feuerstadt P, Longstreth GF, Boley SJ; American College of Gastroenterology. ACG clinical guideline: epidemiology, risk factors, patterns of presentation, diagnosis, and management of colon ischemia (CI). Am J Gastroenterol. 2015;110:18-44; quiz 45. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 183] [Cited by in RCA: 194] [Article Influence: 19.4] [Reference Citation Analysis (0)] |
| 2. | Fujii T, Toda S, Nishihara Y, Maeda Y, Hiramatsu K, Hanaoka Y, Sato R, Matoba S, Ueno M, Kuroyanagi H. Congestive ischemic colitis occurring after resection of left colon cancer: 4 case series. Surg Case Rep. 2020;6:175. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 9] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 3. | Nikolic AL, Keck JO. Ischaemic colitis: uncertainty in diagnosis, pathophysiology and management. ANZ J Surg. 2018;88:278-283. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 17] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 4. | Jin NC, Kim HS, Kim DH, Song YA, Kim YJ, Seo TJ, Park SY, Park CH, Joo YE, Choi SK, Rew JS. A Comparison of clinical characteristics between medically-treated patients and surgically-treated patients with ischemic colitis. Clin Endosc. 2011;44:38-43. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 18] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 5. | Suh JW, Park J, Lee J, Yang IJ, Ahn HM, Oh HK, Kim DW, Kang SB. Clinical impact of inferior mesenteric vein preservation during left hemicolectomy with low ligation of the inferior mesenteric artery for distal transverse and descending colon cancers: A comparative study based on computed tomography. Front Oncol. 2022;12:986516. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 6. | Ahmed M. Ischemic bowel disease in 2021. World J Gastroenterol. 2021;27:4746-4762. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 35] [Cited by in RCA: 38] [Article Influence: 9.5] [Reference Citation Analysis (4)] |
| 7. | Wu MY, Yiang GT, Liao WT, Tsai AP, Cheng YL, Cheng PW, Li CY, Li CJ. Current Mechanistic Concepts in Ischemia and Reperfusion Injury. Cell Physiol Biochem. 2018;46:1650-1667. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 491] [Cited by in RCA: 905] [Article Influence: 129.3] [Reference Citation Analysis (0)] |
| 8. | Luo CC, Shih HH, Chiu CH, Lin JN. Translocation of coagulase-negative bacterial staphylococci in rats following intestinal ischemia-reperfusion injury. Biol Neonate. 2004;85:151-154. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 17] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 9. | Xu Y, Xiong L, Li Y, Jiang X, Xiong Z. Diagnostic methods and drug therapies in patients with ischemic colitis. Int J Colorectal Dis. 2021;36:47-56. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 17] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 10. | Kruis W, Schiff M. Combination Treatment with Antibiotics and Glucocorticosteroids for Severe Ischemic Colitis. Digestion. 2020;101:500-505. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 11. | Bruscoli S, Febo M, Riccardi C, Migliorati G. Glucocorticoid Therapy in Inflammatory Bowel Disease: Mechanisms and Clinical Practice. Front Immunol. 2021;12:691480. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 56] [Cited by in RCA: 113] [Article Influence: 28.3] [Reference Citation Analysis (0)] |
| 12. | MacDermott RP. Progress in understanding the mechanisms of action of 5-aminosalicylic acid. Am J Gastroenterol. 2000;95:3343-3345. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 43] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 13. | Bantel H, Berg C, Vieth M, Stolte M, Kruis W, Schulze-Osthoff K. Mesalazine inhibits activation of transcription factor NF-kappaB in inflamed mucosa of patients with ulcerative colitis. Am J Gastroenterol. 2000;95:3452-3457. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 110] [Cited by in RCA: 128] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 14. | Matsui N, Kasajima K, Hada M, Nagata T, Senga N, Yasui Y, Fukuishi N, Akagi M. Inhibiton of NF-kappaB activation during ischemia reduces hepatic ischemia/reperfusion injury in rats. J Toxicol Sci. 2005;30:103-110. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 32] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 15. | Wu H, Liu L, Tan Q, Wang C, Guo M, Xie Y, Tang C. Somatostatin limits intestinal ischemia-reperfusion injury in macaques via suppression of TLR4-NF-kappaB cytokine pathway. J Gastrointest Surg. 2009;13:983-993. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 37] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 16. | Dong P, Liu K, Han H. The Role of NF-κB in Myocardial Ischemia/Reperfusion Injury. Curr Protein Pept Sci. 2022;23:535-547. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 24] [Reference Citation Analysis (1)] |