Published online Mar 26, 2023. doi: 10.12998/wjcc.v11.i9.2104
First decision: January 20, 2023
Revised: January 28, 2023
Accepted: February 27, 2023
Article in press: February 27, 2023
Published online: March 26, 2023
Processing time: 72 Days and 7.7 Hours
Renal clear cell carcinoma (RCC) is a malignant tumor of the genitourinary system with a predilection for males. The most common metastatic sites are the lung, liver, lymph nodes, contralateral kidney or adrenal gland, however, skin metastasis has only been seen in 1.0%-3.3% of cases. The most common site of skin metastasis is the scalp, and metastasis to the nasal ala region is rare.
A 55-year-old man with clear cell carcinoma of the left kidney was treated with pembrolizumab and axitinib for half a year after surgery and was found to have a red mass on his right nasal ala for 3 mo. The skin lesion of the patient grew rapidly to the size of 2.0 cm × 2.0 cm × 1.2 cm after discontinuation of targeted drug therapy due to the coronavirus disease 2019 epidemic. The patient was finally diagnosed with skin metastasis of RCC in our hospital. The patient refused to undergo surgical resection and the tumor shrank rapidly after resuming target therapy for 2 wk.
It is rare for an RCC to metastasize to the skin of the nasal ala region. The tumor size change of this patient before and after treatment with targeted drugs shows the effectiveness of combination therapy for skin metastasis.
Core Tip: The skin metastasis of renal cell carcinoma can be diagnosed by pathological biopsy and immunohistochemical staining. The patient’s history, laboratory examination and imaging examination can assist in the diagnosis. The occurrence of skin metastasis often indicates a poor prognosis, and surgical treatment may improve the prognosis. Our patient refused surgery and returned to targeted drug therapy, resulting in significant improvement in skin lesions.
- Citation: Dong S, Xu YC, Zhang YC, Xia JX, Mou Y. Pembrolizumab combined with axitinib in the treatment of skin metastasis of renal clear cell carcinoma to nasal ala: A case report. World J Clin Cases 2023; 11(9): 2104-2109
- URL: https://www.wjgnet.com/2307-8960/full/v11/i9/2104.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i9.2104
It is rare for renal clear cell carcinoma (RCC) to metastasize to the facial region, but dermatologists should be alert to the presence of a facial mass in patients with a history of RCC. Here, we report the diagnosis of this patient in detail and provide our experience for the diagnosis of this kind of disease. In addition, this patient also demonstrated the efficacy of pembrolizumab and axitinib for skin metastasis from renal cancer.
The patient presented to our department due to the tumor on his right nasal ala for three months.
The patient reported that a tumor of 0.3 cm × 0.3 cm × 0.2 cm appeared on his right nasal ala with no significant inducement in January 2022. He felt no pain or itching. There was a small amount of bloody exudation on the surface of the tumor. The diagnosis of granuloma was assigned to the patient and the tumor was treated with CO2 laser physiotherapy at a local hospital. In March 2022, the tumor recurred and grew up to 2.0 cm × 2.0 cm × 1.2 cm, so the patient presented to our hospital. Since the onset of the tumor, the patient presented no fever, no nausea, no vomiting and no significant loss of body weight.
In January 2017, a tumor was identified in the left kidney of the patient by physical examination. The patient underwent a robot-assisted partial nephrectomy at a local hospital. Postoperative pathological examination showed left RCC. No adjuvant therapy was performed. In July 2021, the patient underwent a left renal radical resection in the local hospital. Postoperative pathological examination revealed left RCC. The tumor volume was 3.5 cm × 3 cm × 2.5 cm. Invasion of renal sinus adipose tissue at the maximum diameter of 0.7 cm was observed, vascular cancer infiltration was seen and fat necrosis nodules with fibrosis and calcification occurred in the surrounding renal tissue, pTNM: T3a (2017 AJCC 8th). August 2021, the positron emission tomography/computed tomography (CT) results displayed left renal cell carcinoma after surgery, the surgical area showed high metabolism, and metastasis was suspected. It was found that metastasis occurred to the left humerus, 1st and 12th thoracic vertebrae. In September 2021, posterior thoracic tumor resection and decompression plus radiofrequency ablation, internal fixation plus nerve root exploration were performed in another hospital. Postoperative pathological results showed broken bone and tumor cell infiltration in fibrous soft tissue, cell nest distribution and some empty cytoplasm, which was consistent with renal cell carcinoma metastasis. Pembrolizumab and axitinib were administered regularly after the operation, however, the treatment was discontinued due to the coronavirus disease 2019 epidemic between March and April 2022.
The patient has had a history of hypertension for 5 years and smoked for over 30 years. No member of his family has a similar disease.
The general condition of the patient was fair, the left kidney was deficient. Physical examination showed bilateral renal tenderness and tapping pain negative, thoracic surgery, spinal tenderness and tapping pain negative. Limbs and lung examination showed no obvious abnormalities.
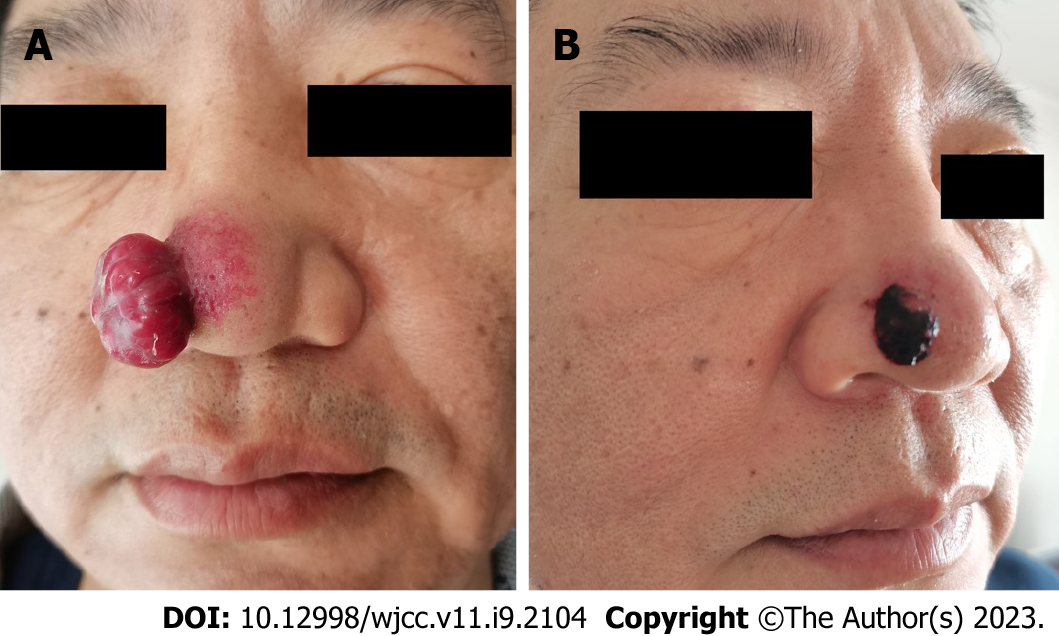
A tumor of 2.0 cm × 2.0 cm × 1.2 cm was seen on the right nasal ala, there was a small amount of bloody exudation on the surface, and no tenderness (Figure 1A). There was no bleeding in the nasal cavity. The superficial lymph nodes of the whole body were not enlarged.
Lung CT showed nodular high-density shadows in each lobe of both lungs, with a size of about 0.2-1.1 cm, and some edges are lobulated, which indicated lung metastasis. Magnetic resonance results showed once surgery and signal changes at the 1st and 2nd thoracic vertebrae and their partial attachment area. Based on the disease history of the patient, tumor metastasis to the vertebrae was suspected. There were 2 suspected tumors in the left head of the humerus and shaft of the humerus. No obvious abnormality was found in the blood routine, coagulation routine, liver and kidney function, thyroid function, myocardial enzyme and electrocardiogram.
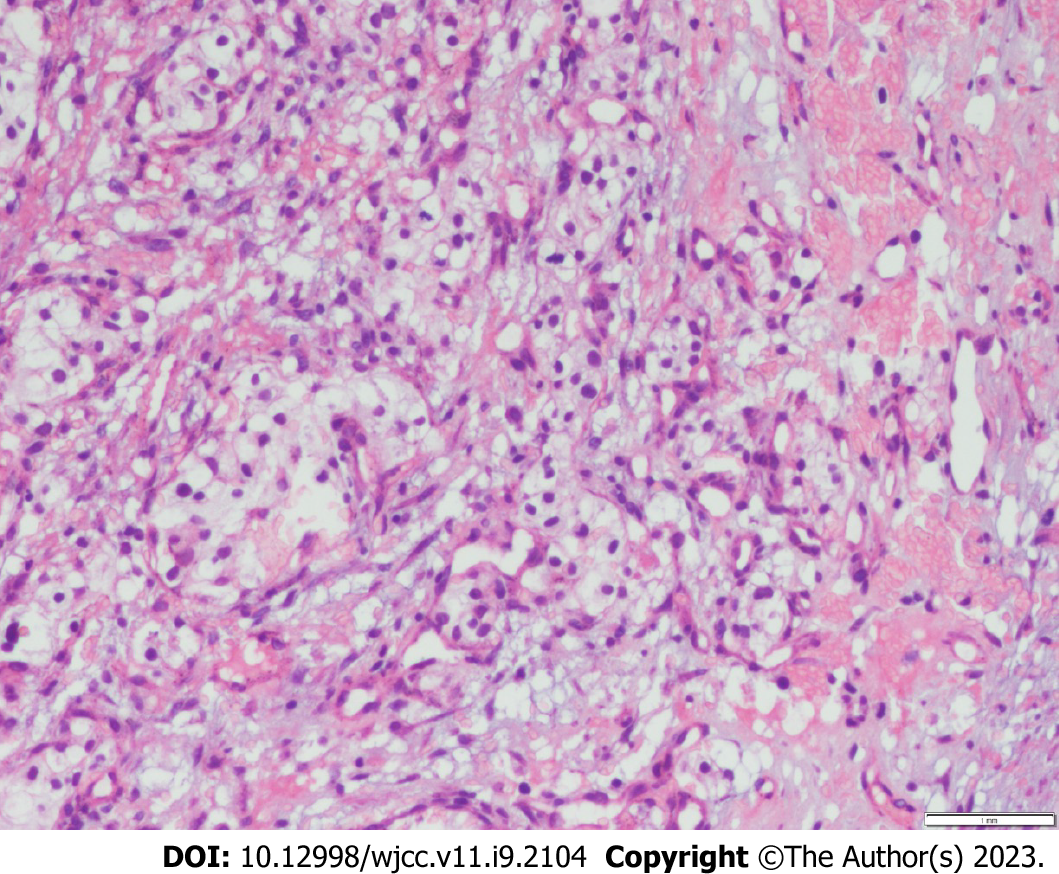
There were significant changes in the epidermis, and the tumor cells gathered to form a mass in the dermis, some tumor cells formed a lumen structure. There were a lot of clear cells and abundant blood vessels (Figure 2).
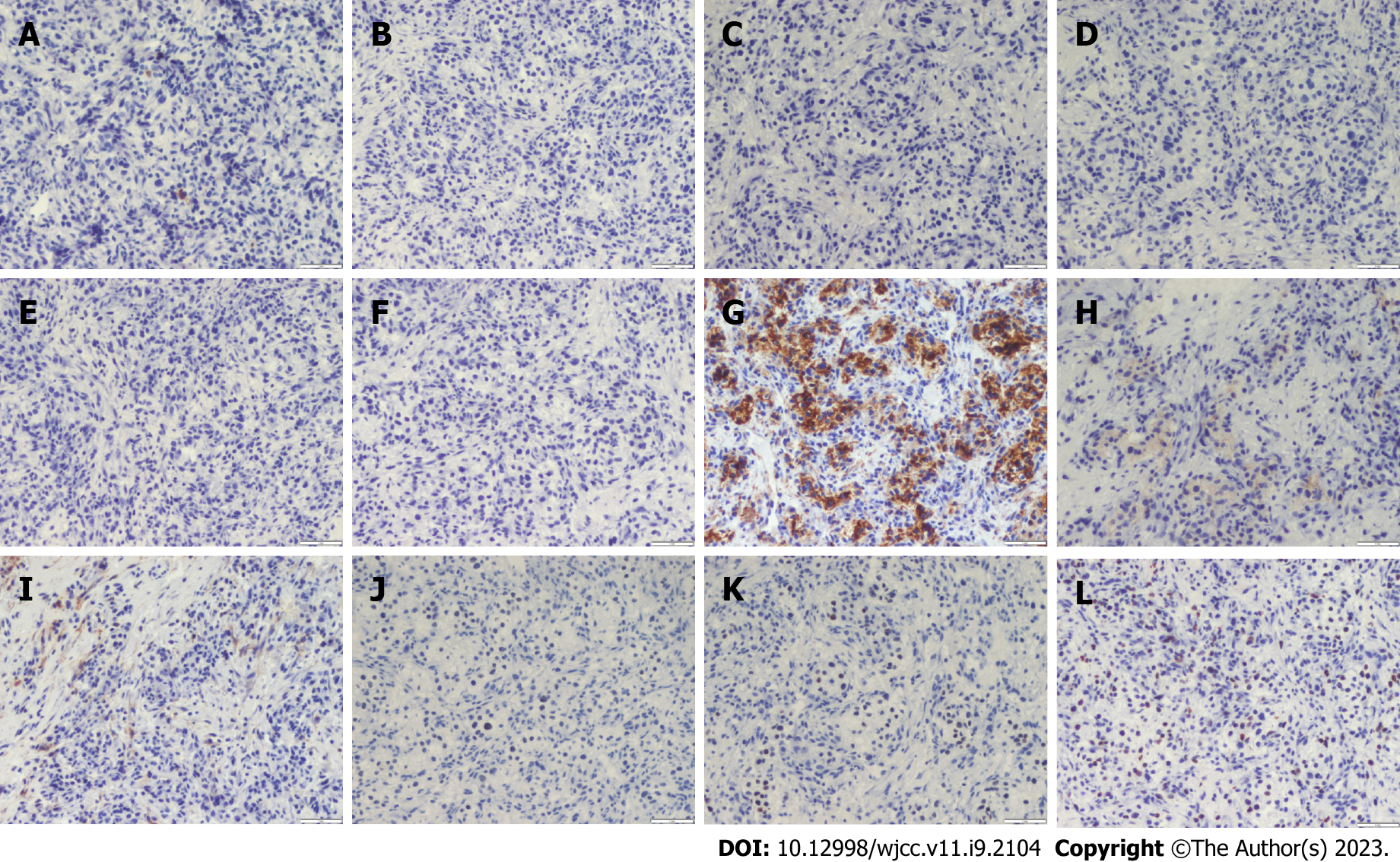
Tumor immune pathology detection: S100-, HMB45-, CK7-, AR-, CK5/6-, CAIX-, Vimentin+, EMA weak+, CD10+, PAX8 weak+, PAX2 weak+ and Ki67 30%+ (Figure 3).
Skin metastasis of RCC.
The proposal for surgical resection of the tumors on the nasal ala was rejected by the patient and the patient also refused to have his suspected bone metastasis or lung metastasis biopsied and treated. The patient resumed his treatment with pembrolizumab and axitinib for 2 wk, and the tumor on his nasal ala shrank to 0.8 cm × 0.8 cm × 0.5 cm (Figure 1B).
200 mg pembrolizumab was administered to the patient through intravenous infusion once every 3 wk combined with axitinib 5 mg twice a day orally. After 8 wk of treatment, the skin lesion was 0.6 cm × 0.6 cm × 0.4 cm. Upon subsequent follow-up, his lesion remained 0.6 cm × 0.6 cm × 0.4 cm and there were no new lesions. Unfortunately, he died of multiple organ failure in December 2022.
RCC is a kind of malignant tumor of the genitourinary system, which usually occurs in males. The most common metastatic sites are the lung, liver, lymph node, contralateral kidney or adrenal gland. Skin metastasis is rare, only in 1.0%-3.3% of RCC cases[1]. Skin metastasis from renal carcinoma mostly occurs in the scalp, rarely in the nasal ala[2]. Balawender et al[3] reported cases of cutaneous metastasis of renal cell carcinoma from 2000 to 2019, with only two cases of nasal cutaneous metastasis.
A cutaneous metastatic lesion from renal cell carcinoma is often present as painless nodules, plaques or pulsatile masses of normal to purplish-red skin and grow rapidly[4]. Vascular-rich metastases are hard to distinguish from hemangiomas, pyogenic granulomas or Kaposi's sarcoma[5]. The histopathology of this case showed a mass-like infiltration of tumor cells in the dermis with clear cytoplasm and nuclei in the center, which should be differentiated from sebaceous adenocarcinoma, melanoma and clear cell squamous cell carcinoma. PAX8 and PAX2 are nuclear transcription factors that are expressed in approximately 90% of renal cell tumors and can be used as markers for the diagnosis of distant metastatic tumors originating from the kidney; CD10 can be used as a marker for the recognition of tumors originating from the renal tubules and CD10 is positive in clear cell renal tumor; EMA and Vimentin are frequently expressed in clear cell renal cell carcinoma, which is uncommon in other clear cell tumors[6]. Immunohistochemical staining of this case showed that melanoma could be excluded because S100 and HMB45 were negative, sebaceous adenocarcinoma could be excluded because CK7 and AR were negative, clear cell squamous cell carcinoma could be excluded because CK5/6 and CAIX were negative[7]. Vimentin positive, EMA weakly positive, CD10 positive, PAX8 weakly positive, PAX2 weakly positive and Ki67 30% positive can be diagnosed as skin metastasis of RCC.
Metastatic RCC is insensitive to both radiotherapy and chemotherapy[8]. Surgical resection of isolated skin metastases has the potential to improve survival[9]. Axitinib is a class of oral small-molecule tyrosine kinase inhibitors that inhibit receptors such as VEGR and PDGFR-B, thereby inhibiting tumor angiogenesis and preventing tumor growth and metastasis[10]. Pembrolizumab, a humanized monoclonal antibody that binds to the PD-1 receptor, blocking the interaction of PD-1 with PD-L1 and PD-L2, relieving the suppression of the immune response mediated by the PD-1 pathway, enhances the body's immune system for the killing of tumor cells. Pembrolizumab and axitinib are used as first-line therapy for advanced renal cancer, the skin lesion of this patient developed rapidly after discontinuation of this regimen, and the tumor shrank significantly after treatment was resumed, which demonstrated the effectiveness of this treatment for skin metastases.
It is very rare for RCC to metastasize to the skin of the nasal ala region. It is easily misdiagnosed as hemangioma, pyogenic granuloma or Kaposi's sarcoma. Learning the detailed medical history and histopathology examination can help to avoid misdiagnosis. RCC patients with skin metastases often have a poor prognosis, and surgical removal of the metastases can be an option to improve the prognosis, but further systemic examination and comprehensive treatment are necessary. In this patient, pembrolizumab in combination with axitinib significantly reduced the size of the lesion, demonstrating the efficacy of the targeted drug for skin metastases.
We thank the patients and their families for their support.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Peer review started: January 4, 2023
Specialty type: Dermatology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Bal’afif F, Indonesia; Sedaghattalab M, Iran S-Editor: Yan JP L-Editor: A P-Editor: Yan JP
| 1. | Singh P, Somani K. Latent distant metastasis of renal cell carcinoma to skin: A case report. Clin Case Rep. 2020;8:1138-1141. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Reference Citation Analysis (0)] |
| 2. | Vilaça M, Braga F, Mesquita A. Cutaneous Metastases and Long-Term Survival of a Patient With Clear Cell Renal Carcinoma. Cureus. 2022;14:e23598. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 3. | Balawender K, Przybyła R, Orkisz S, Wawrzyniak A, Boroñ D, Grabarek BO. Cutaneous metastasis as the first sign of renal cell carcinoma - crossroad between literature analysis and own observations. Postepy Dermatol Alergol. 2022;39:553-558. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 4. | Altinkaya A, Yazar S, Karadag EC, Er O. Large solitary scalp metastasis of renal cell carcinoma: A case report. Niger J Clin Pract. 2021;24:629-631. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 5. | Kramer DE, Kerolus MG, Tan LA, Patel S, Reddy V, Chen M. Embolization of an Exophytic Posterior Neck Mass Secondary to a Cutaneous Renal Cell Carcinoma Metastasis. Neurointervention. 2020;15:162-166. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 6. | Ozcan A, de la Roza G, Ro JY, Shen SS, Truong LD. PAX2 and PAX8 expression in primary and metastatic renal tumors: a comprehensive comparison. Arch Pathol Lab Med. 2012;136:1541-1551. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 75] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 7. | Khoury ZH, Bugshan A, Lubek JE, Papadimitriou JC, Basile JR, Younis RH. Glycogen-Rich Clear Cell Squamous Cell Carcinoma Originating in the Oral Cavity. Head Neck Pathol. 2017;11:552-560. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 9] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 8. | Paula TAd, Silva PSLd, Berriel LGS. Carcinoma de células renais com metástase cutânea: relato de caso. Jornal Brasileiro de Nefrologia. 2010;32:213-215. [RCA] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 9. | Leve PP, Felício J, Carneiro R, Zagalo C. Recurrent renal cell carcinoma presenting as a cutaneous metastasis: A case report and review of the literature. Urol Ann. 2021;13:174-176. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 10. | Keating GM. Axitinib: a review in advanced renal cell carcinoma. Drugs. 2015;75:1903-1913. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 41] [Article Influence: 4.6] [Reference Citation Analysis (0)] |