Published online Mar 26, 2023. doi: 10.12998/wjcc.v11.i9.2098
Peer-review started: December 26, 2022
First decision: January 12, 2023
Revised: January 18, 2023
Accepted: February 21, 2023
Article in press: February 21, 2023
Published online: March 26, 2023
Processing time: 81 Days and 5.9 Hours
The R-on-T phenomenon is a malignant arrhythmia associated with potentially catastrophic consequences. It may initiate ventricular tachycardia or ventricular fibrillation, which can result in syncope or sudden cardiac death. This manifesta
We herein present a case in which the R-on-T phenomenon was incidentally revealed by 24-h Holter monitoring in a patient diagnosed with sigmoid colon cancer. Careful evaluation and treatment with mexiletine were carried out preoperatively under consultation with a cardiovascular specialist, and surgery was uneventfully performed under general anesthesia after thorough preparation.
Physicians should be vigilant about this infrequent but potentially fatal arrhythmia. Our experience suggests that the anesthetic process can be greatly optimized with careful preparation.
Core Tip: The R-on-T phenomenon is associated with an increased risk of fatal arrhythmia. It may initiate ventricular tachycardia and ventricular fibrillation, and its appearance seem to be associated with a poor prognosis. However, this phenomenon is rarely encountered in the preoperative inpatient setting. The anesthetic management of patients with this particular manifestation poses a great challenge. We herein describe a patient who was scheduled for laparoscopic-assisted sigmoid colon resection when the R-on-T phenomenon was incidentally discovered. Our experience suggests that the anesthetic process can be greatly optimized by detailed preoperative assessment and preparation with interdisciplinary cooperation.
- Citation: Li XX, Yao YF, Tan HY. Anesthetic management of a patient with preoperative R-on-T phenomenon undergoing laparoscopic-assisted sigmoid colon resection: A case report. World J Clin Cases 2023; 11(9): 2098-2103
- URL: https://www.wjgnet.com/2307-8960/full/v11/i9/2098.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i9.2098
The R-on-T phenomenon was first reported by Smirk[1], who described it as R waves interrupting T waves. The R-on-T phenomenon may initiate ventricular tachycardia (VT), torsade de pointes, and ventricular fibrillation (VF)[2-5]. This phenomenon is associated with an increased risk of fatal arrhythmia. The anesthetic management of patients with this particular manifestation poses a great challenge. However, the R-on-T phenomenon is seldom encountered in the preoperative inpatient setting. We found no report describing the anesthetic management of patients with a preoperative electrocardiographic (ECG) manifestation of R-on-T, and there is an extreme lack of experience to which clinicians can refer.
We herein present a case of successful anesthetic management in a patient who was incidentally found to have the R-on-T phenomenon before undergoing laparoscopic-assisted sigmoid colon resection. We also discussed the cause of the appearance of the R-on-T phenomenon and the main issue requiring special precaution during perioperative anesthetic management.
A 69-year-old man was diagnosed with a sigmoid colon mass during a physical examination.
The patient had undergone a colonoscopy 20 d previously, and a sigmoid colon mass was discovered. The diagnosis of sigmoid colon cancer was considered based on pathological biopsy findings. The patient was admitted to our hospital for sigmoid colon resection.
The patient had been previously diagnosed with a congenital ventricular septal defect, and he had a history of fundus hemorrhage 3 years previously. He had been undergoing treatment with Chinese patent medicine containing Panax notoginseng saponins as well as Aescuven forte until 1 mo before presentation to our hospital. He had no history of other systemic diseases such as hypertension, diabetes mellitus, or coronary heart disease.
The patient had a 50-year smoking history. He had undergone an open appendectomy 5 years previously. His brother was diagnosed with colon cancer.
Physical examination revealed no obvious abnormalities except for an old appendiceal incision scar.
Preoperative laboratory results, including a full blood cell count, blood biochemistry (including electrolytes), and coagulation tests, were unremarkable except for a slightly elevated fibrinogen concentration of 456.3 mg/dL and uric acid concentration of 455 μmol/L.
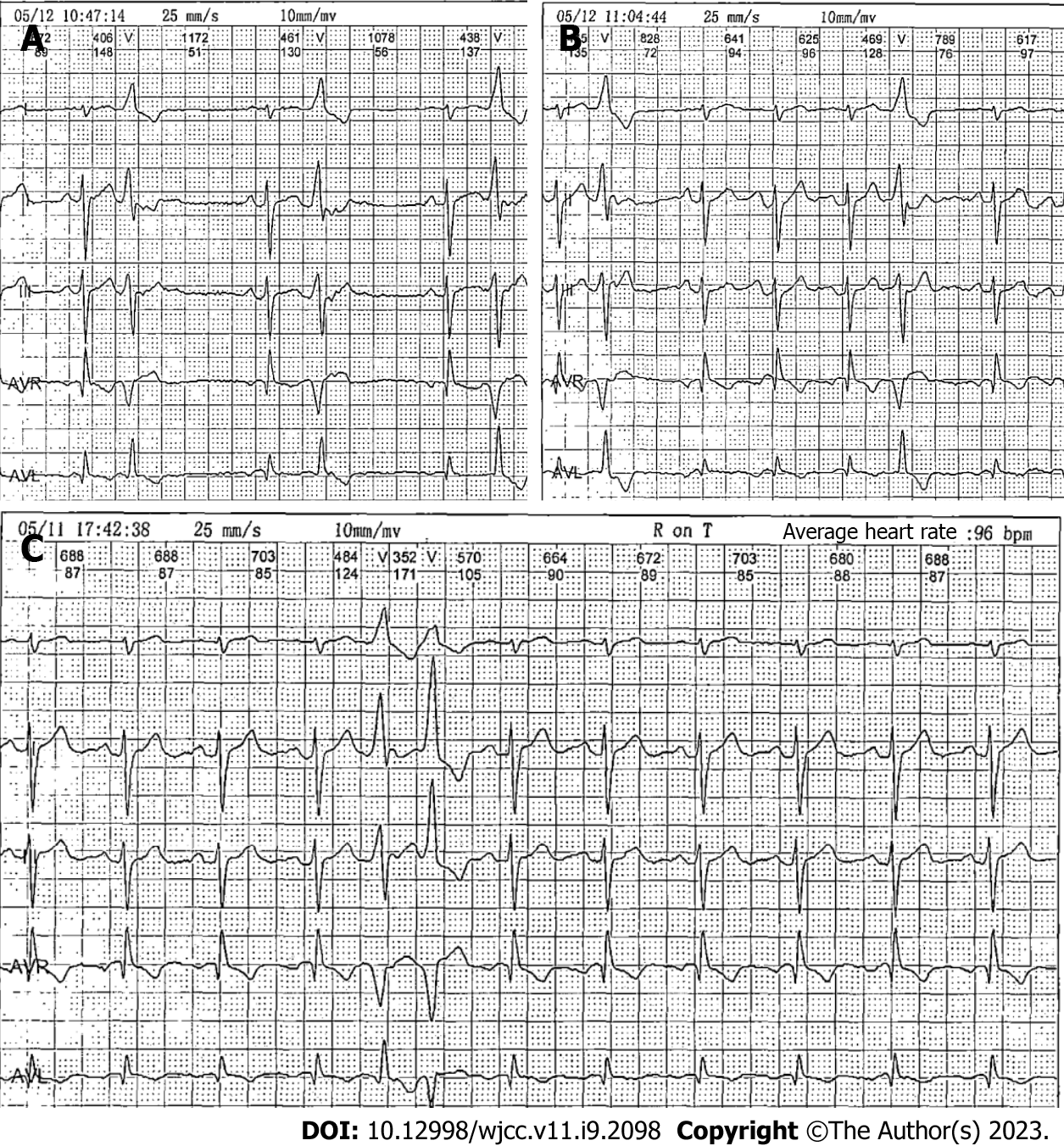
Chest X-ray findings and abdominal computed tomography (CT) findings were unremarkable. A transthoracic echocardiogram showed minor regurgitation of the aortic, mitral, and tricuspid valves; reduced left ventricular diastolic function; and an ejection fraction of 62%. Notably, 24-h Holter monitoring performed 2 d earlier revealed occasional atrial premature beats and frequent premature ventricular contractions (PVCs). The PVCs consisted of 7.5% of the total daily beats (8803 per day), partially occurred in pairs, and occasionally occurred in bigeminy and trigeminy; Twenty-five R-on-T phenomena were revealed (Figure 1).
During pre-anesthetic assessment the day before surgery, the patient denied any history of palpitations, dizziness, syncope, or any symptoms of angina. He stated that his ventricular septal defect was minimal and required no medication or surgical treatment and that his physical activity was not limited. His relatives provided the results of coronary artery CT and exercise myocardial perfusion imaging that had been performed 18 mo previously. The coronary artery CT showed a minimal periventricular septal defect with no hemodynamic effects as well as calcification of the left anterior descending artery, circumflex branch artery, and right coronary artery; the images were negative for arterial stenosis. The exercise myocardial perfusion imaging revealed no definite evidence of myocardial ischemia.
The final diagnoses were sigmoid colon cancer, congenital ventricular septal defect, and arrhythmia.
The patient was scheduled for laparoscopic-assisted sigmoid colon resection under general anesthesia. Myocardial enzyme and electrolyte measurements and continuous ECG monitoring were advised for further evaluation by the anesthesiologist, and a cardiovascular specialist was invited for consultation. All laboratory results were normal. The cardiovascular specialist suggested the administration of mexiletine at 150 mg three times daily and continuous infusion of lidocaine during surgery, and he advised that a defibrillator should be prepared in advance. The surgery was scheduled 1 day after the consultation, and a total of 450 mg of mexiletine was administered preoperatively. The patient underwent continuous bedside ECG monitoring. His heart rate (HR) remained between 67 and 81 bpm. There was a slight trend of slowing of the HR compared with his previous 24-h Holter monitoring (average HR, 84 bpm). There was no sign of QT prolongation. PVCs occurred during observation. However, the patient reported no discomfort.
Standard monitoring on the day of the operation included measurement of the patient’s arterial blood pressure (ABP), ECG, SpO2, bispectral index, and arterial blood gas analysis. Monitoring of cardiac function by a FloTrac system (Edwards Lifesciences, Irvine, CA, United States) was also performed. The patient was in stable condition with a HR of 72 bpm, ABP of 155/80 mmHg, and SpO2 of 99% on room air. The ECG monitoring revealed that the number of PVCs had markedly decreased (approximately two PVCs within 10 min), and no R-on-T phenomenon was observed. The results of the arterial blood gas analysis were within normal range (pH, 7.43; potassium, 4.2 mmol/L; calcium, 1.19 mmol/L; glucose, 5.5 mmol/L). Defibrillation electrode slices were placed on the patient, and rescue medications were prepared. He was premedicated with 5 mg of dexamethasone. After preoxygenation, anesthesia was induced with 20 µg of sufentanil, 40 mg of lidocaine, 20 mg of etomidate, 80 mg of propofol, and 20 mg of cisatracurium. Esmolol (20 mg) was administered at the time of intubation to inhibit the stress response of endotracheal intubation. The patient was intubated successfully with the GlideScope video laryngoscope (Verathon, Bothell, WA, United States). Anesthesia was maintained with propofol, remifentanil, and sevoflurane. Muscle relaxation was achieved with intermittent administration of cisatracurium. Lidocaine was continuously administered at a speed of 40 mg/h throughout the surgery. During surgery, 6 mg of ephedrine was administered once to correct hypotension when the ABP had fallen to 100/60 mmHg. The patient’s ABP was maintained at 100-168/60-82 mmHg, and his HR remained between 55 and 88 bpm. An arterial blood gas analysis performed 1 h after the beginning of surgery showed a pH of 7.33, partial pressure of carbon dioxide of 48 mmHg, and all electrolyte levels within the reference ranges. The ventilator parameters were adjusted according to these results to maintain normal acid base balance and electrolyte levels. His cardiac output and stroke volume variation as monitored by the FloTrac system were within normal limits during surgery. Fluid therapy was directed according to his HR, ABP, cardiac output, and stroke volume variation. Infusion heating and a forced air warmer were used to maintain his body temperature. Occasional PVCs occurred, but the patient was otherwise stable. The amount of bleeding during surgery was 50 mL.
The patient’s surgery and remaining hospital stay were uneventful. He was discharged home in a stable state on postoperative day 6.
The appearance of the R-on-T phenomenon is associated with an increased risk of syncope and sudden cardiac death. The literature shows that the R-on-T phenomenon can be triggered by myocardial damage, reperfusion injury after revascularization, electrolyte imbalance (especially hypokalemia), or hypothermia[1]. In rare cases, the administration of antibiotics can also cause the R-on-T phenomenon[6]. Among all causes, cardiac ischemia and cardiac infarction are most common. A detailed preoperative anesthetic assessment with emphasis on the cardiovascular system is important. Previous cardiac assessment and examinations are helpful for comparison with current data. In the present case, the definitive cause of the R-on-T phenomenon was unclear. Although the patient had a congenital ventricular septal defect, the defect was minimal and had no hemodynamic effects. He had no history of coronary heart disease and no evidence of cardiac ischemia. He was not taking any medication presently and had no electrolyte imbalances. Therefore, we considered the possibility that his arrhythmia was idiopathic.
PVCs, especially with the R-on-T phenomenon, can initiate VT or VF[7-9]. The PVCs that precede VF are considered to trigger the VF episodes in arrhythmic storm. VF recurrence can be avoided by suppressing these PVCs using drugs, pacing, or ablation. The risk of the R-on-T phenomenon can be eliminated or greatly diminished by treatment with antiarrhythmic drugs[1,10,11]. In the present study, the patient was medically treated with the class Ib antiarrhythmic agent mexiletine, and he appeared to respond well to mexiletine based on the fact that the number of PVCs was significantly reduced and the R-on-T phenomenon disappeared on his arrival to the operating room. The literature shows that the application of cardiac resynchronization therapy and catheter ablation can also be an effective remedy when drug therapy is unsatisfactory[9,10,12,13].
The patient had a favorable prognosis in the present case; this was attributed to a detailed preoperative assessment and preparation with interdisciplinary cooperation among the surgery, anesthesiology, and cardiovascular departments. Full preparation including elaborate monitoring, rescue medications, and a readily available defibrillator prepared in advance are crucial to decrease patient risk. We placed defibrillation electrode slices on the patient before anesthetic induction in case of VT or VF. Continuous lidocaine infusion can be used for both prophylaxis and treatment of ventricular arrhythmia. All factors that can deteriorate the arrhythmia, including hemodynamic instability, fluid and electrolyte imbalances (meticulous electrolyte control is important especially during laparoscopic surgeries), and hypothermia, should be avoided. Induction drugs that are less likely to cause hypotension, such as etomidate, are preferred. Avoidance of fluid and electrolyte imbalances is essential. Goal-directed fluid therapy is instructive. Insulation measures, including the use of infusion heating and forced air warmers, should also be applied to prevent hypothermia.
The R-on-T phenomenon is rarely encountered in the perioperative setting. Physicians should be vigilant about this infrequent but potentially fatal arrhythmia. The perioperative anesthetic management of patients with this manifestation can be challenging. However, our experience suggests that the anesthetic process can be greatly optimized with careful evaluation, multidisciplinary consultation, and thorough preparation.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Anesthesiology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Kvolik S, Croatia; Yamada T, United States S-Editor: Yan JP L-Editor: A P-Editor: Yan JP
| 1. | Smirk FH. R waves interrupting T waves. Br Heart J. 1949;11:23-36. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 90] [Cited by in RCA: 84] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 2. | Schulman PM, Merkel MJ, Rozner MA. Accidental, unintentional reprogramming of a temporary external pacemaker leading to R-on-T and cardiac arrest. J Cardiothorac Vasc Anesth. 2013;27:944-948. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 3. | Ergul Y, Kafali HC, Uysal F. Accelerated idioventricular rhythm resulting in torsades de pointes and cardiac arrest in a child: successfully cryoablated in left'coronary cusp. Cardiol Young. 2020;30:418-421. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 4. | Cho J, Afolabi B. Ventricular fibrillation associated with Graves' disease and amiodarone induced thyrotoxicosis. Cardiovasc Endocrinol Metab. 2019;8:119-124. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 5. | Marume K, Ishibashi K, Noda T, Ohta-Ogo K, Yasuda S, Kusano K. Short coupled Torsade de pointes with myocardial injury: A possible sequela of myocarditis. J Cardiol Cases. 2019;19:62-65. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 6. | Anyfantakis D, Makrakis G. R on T Phenomenon and Long QTc Syndrome due to Moxifloxacin in a Healthy Female. P R Health Sci J. 2019;38:196-197. [PubMed] |
| 7. | Oksuz F, Sensoy B, Sahan E, Sen F, Baser K, Cetin H, Unal S, Ozeke O, Topaloglu S, Aras D. The classical "R-on-T" phenomenon. Indian Heart J. 2015;67:392-394. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 8. | Nakamori Y, Maeda T, Ohnishi Y. Reiterative ventricular fibrillation caused by R-on-T during temporary epicardial pacing: a case report. JA Clin Rep. 2016;2:3. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 8] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 9. | Lasocka Z, Dąbrowska-Kugacka A, Lewicka E, Liżewska-Springer A, Królak T. Successful Catheter Ablation of the "R on T" Ventricular Fibrillation. Int J Environ Res Public Health. 2021;18. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 10. | Vyas A, Lokhandwala Y. Coronary sinus as a site for stable temporary atrial pacing to tide over premature ventricular complex-triggered recurrent ventricular fibrillation in a patient with severe left ventricular dysfunction after coronary bypass surgery. Indian Heart J. 2018;70 Suppl 3:S483-S485. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 11. | Sánchez Muñoz JJ, García-Alberola A, Martínez-Sánchez J, Peñafiel-Verdú P, Caro-Martínez C, Manzano-Fernández S, Valdés Chávarri M. Premature ventricular complexes as a trigger for ventricular fibrillation. Rev Esp Cardiol. 2010;63:798-801. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 12. | Jeon DS, Park JS. Rapid and Potent Antiarrhythmic Effect of Cardiac Resynchronization Therapy in a Patient with Advanced Dilated Cardiomyopathy and a Large Ventricular Arrhythmia Burden. Korean Circ J. 2017;47:523-527. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 13. | Katis G, Wiles B, Saba MM. Short-coupled ventricular ectopics leading to cardiac arrest in a young woman. Egypt Heart J. 2022;74:32. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |