Published online Mar 26, 2023. doi: 10.12998/wjcc.v11.i9.2043
Peer-review started: November 25, 2022
First decision: December 19, 2022
Revised: December 28, 2022
Accepted: February 15, 2023
Article in press: February 15, 2023
Published online: March 26, 2023
Processing time: 112 Days and 2.5 Hours
Manubriosternal joint (MSJ) disease is a rare cause of anterior chest pain but can be a major sign of systemic arthritic involvement. In patients with ankylosing spondylitis (AS), a type of systemic arthritis, chest pain can be due to MSJ involvement and can be improved by ultrasound-guided corticosteroid injection into the joint.
A 64-year-old man visited our pain clinic complaining of anterior chest pain. There were no abnormal findings on lateral sternum X-ray, but arthritic changes in the MSJ were observed on single-photon emission computed tomography-computed tomography. We performed additional laboratory tests, and he was finally diagnosed with AS. For pain relief, we performed ultrasound-guided intra-articular (IA) corticosteroid injections into the MSJ. After the injections, his pain nearly resolved.
For patients complaining of anterior chest pain, AS should be considered, and single-photon emission computed tomography-computed tomography can be helpful in diagnosis. In addition, ultrasound-guided IA corticosteroid injections may be effective for pain relief.
Core Tip: Manubriosternal joint (MSJ) disease is a rare cause of anterior chest pain but can be a major sign of systemic arthritic involvement. In patients with anterior chest pain, systemic arthritic diseases such as ankylosing spondylitis should be considered but are difficult to diagnose. This report suggests that single-photon emission computed tomography-computed tomography can be an effective diagnostic tool for evaluating musculoskeletal causes of anterior chest pain, and this pain can be controlled by ultrasound-guided intra-articular corticosteroid injections into the MSJ.
- Citation: Choi MH, Yoon IY, Kim WJ. Ultrasound-guided intra-articular corticosteroid injection in a patient with manubriosternal joint involvement of ankylosing spondylitis: A case report. World J Clin Cases 2023; 11(9): 2043-2050
- URL: https://www.wjgnet.com/2307-8960/full/v11/i9/2043.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i9.2043
Manubriosternal joint (MSJ) disease is an often undetected cause of anterior chest pain[1]. Diagnosis is difficult as it is based on exclusion of other causes[2]. Many diagnostic tools can be used to identify diseases that cause anterior chest pain. Particularly, single-photon emission computed tomography-computed tomography (SPECT-CT) can be helpful in differentiating the diagnosis due to musculoskeletal disorders such as arthritis.
Infection, trauma, crystal deposition disease, and inflammatory diseases such as ankylosing spondylitis (AS) and rheumatic arthritis (RA) can cause arthritis of the MSJ[3]. Although these diseases are often accompanied by systemic symptoms, in rare cases intermittent MSJ arthralgia can be a major sign of arthritic involvement.
We report a case in which a patient with anterior chest pain as the main symptom was diagnosed with AS through SPECT-CT, and the pain was relieved by ultrasound-guided intra-articular (IA) corticosteroid injections.
A 64-year-old man (180 cm, 81 kg) visited our pain clinic with intermittent anterior chest pain lasting 6 mo.
The patient’s chest pain worsened when he engaged in exercises like pull-ups or changed position. This pain affected his ability to work and perform activities of daily living. He also had mild back pain, but it did not interfere with his daily activities and did not require treatment.
The patient had no history of trauma to his anterior chest. His symptoms worsened 3 mo prior to his visit, based on which an orthopedic doctor prescribed non-steroidal anti-inflammatory drugs (NSAIDs) and injected corticosteroids into the painful area. However, the pain did not improve.
The patient had no family or personal history related to the symptom.
On physical examination, there was tenderness in the left anterior chest wall but no swelling or heat sensation. There was no back tenderness.
Blood tests including complete blood count, inflammatory markers (C-reactive protein, erythrocyte sedimentation rate), blood biochemistry, and coagulation indices were within the normal ranges.
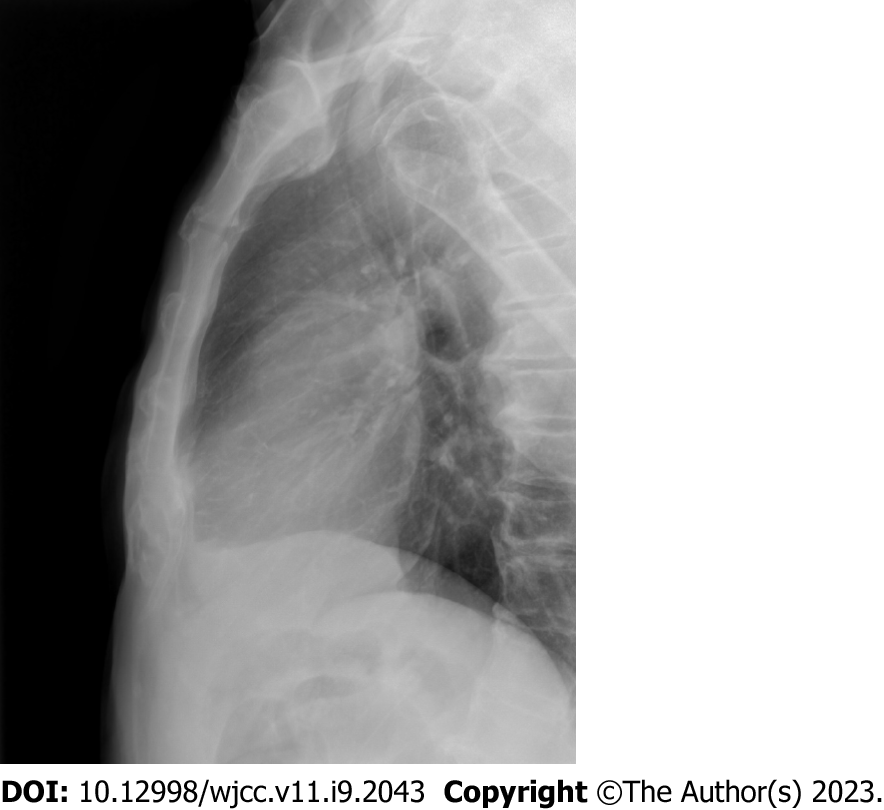
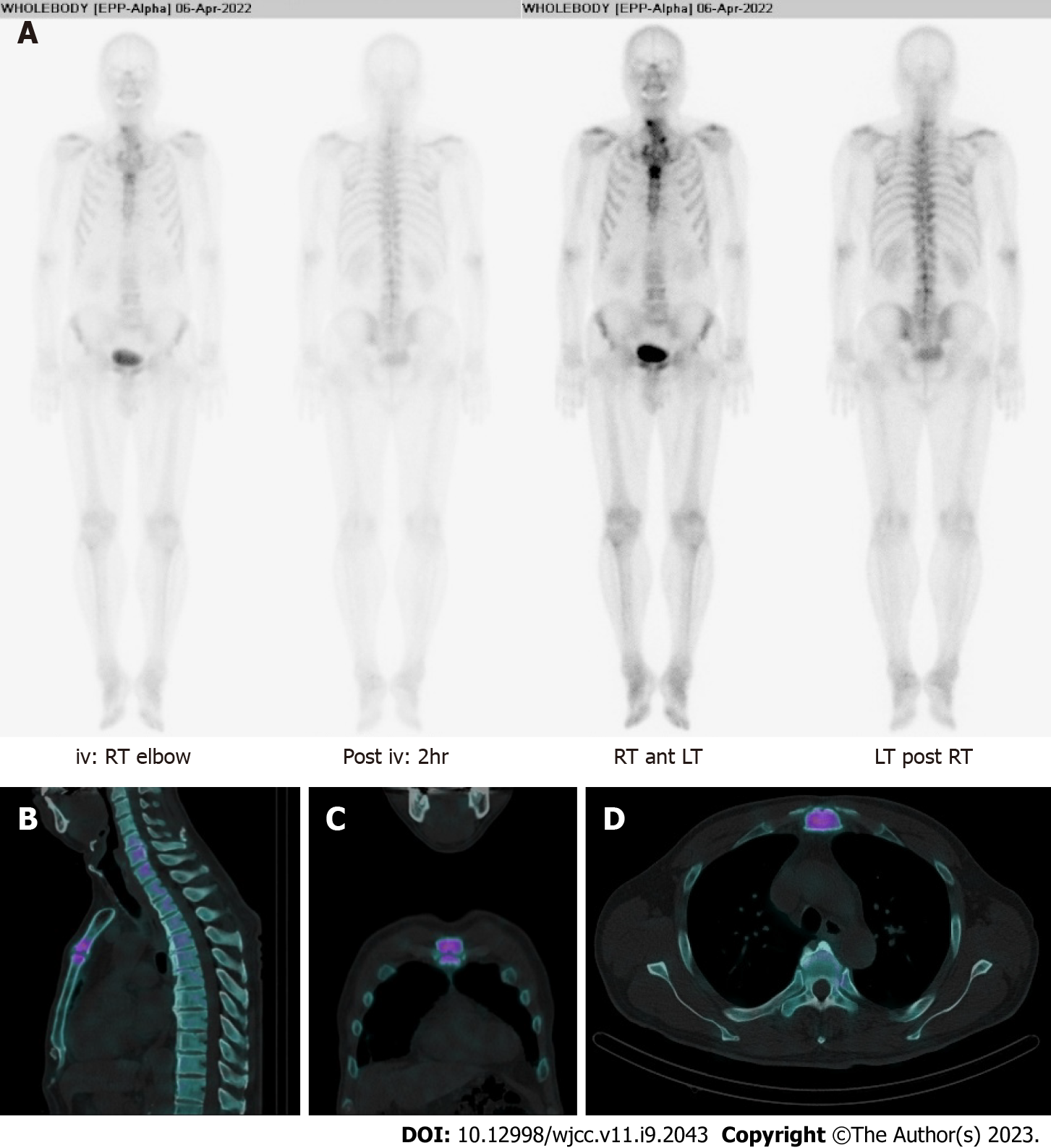
There were no abnormal findings on lateral sternum X-ray (Figure 1), but arthritic changes in the MSJ were observed on SPECT-CT (Figure 2). In bone scintigraphy, there was no active inflammation in the sacroiliac joint (SIJ).
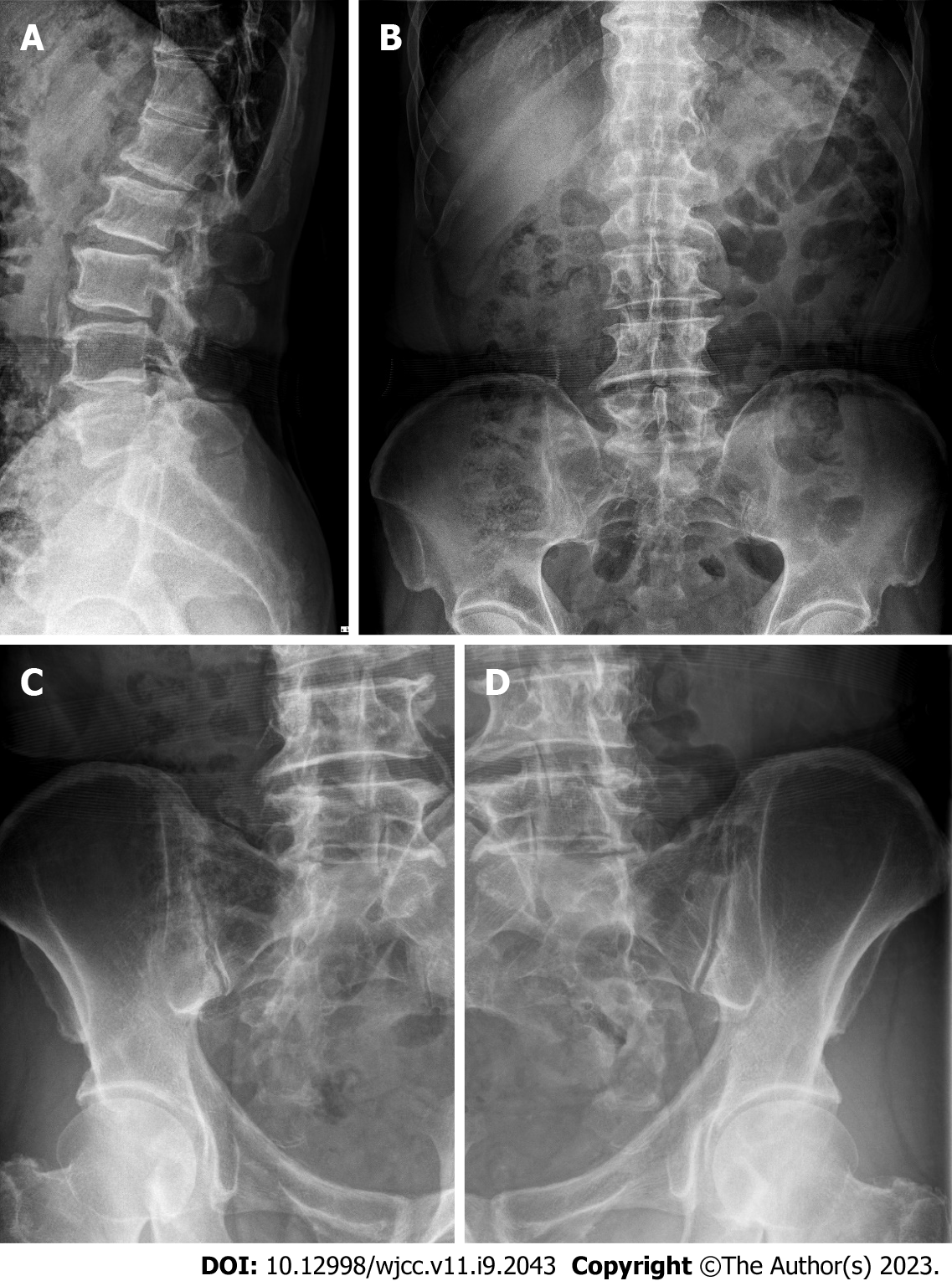
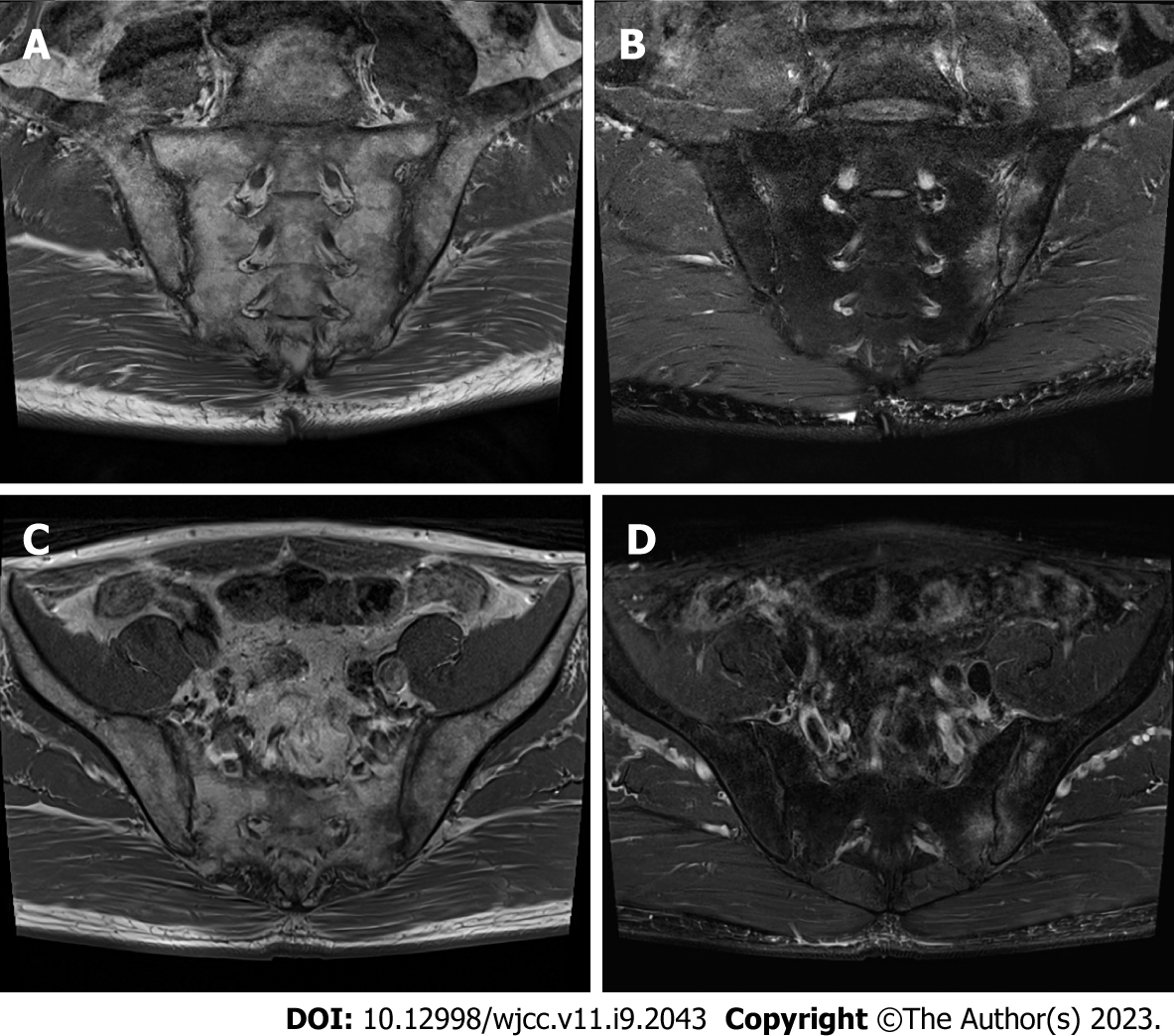
Rheumatoid factor, anti-cyclic citrullinated peptide antibody, uric acid, fluorescent anti-nuclear antibody, and human leukocyte antigen-B27 tests were performed, and human leukocyte antigen-B27 was positive. SIJ pain provocation tests (distraction, thigh thrust, compression, Patrick, and Gaenslen) and the Schober test were negative. X-rays of the lumbar spine and SIJ showed syndesmophytes and sacroiliitis (Figure 3). Subsequent magnetic resonance imaging (MRI) of the SIJ revealed bilateral sacroiliitis with active inflammation at the left SIJ (Figure 4).
According to the modified New York Classification Criteria, the patient was diagnosed with AS.
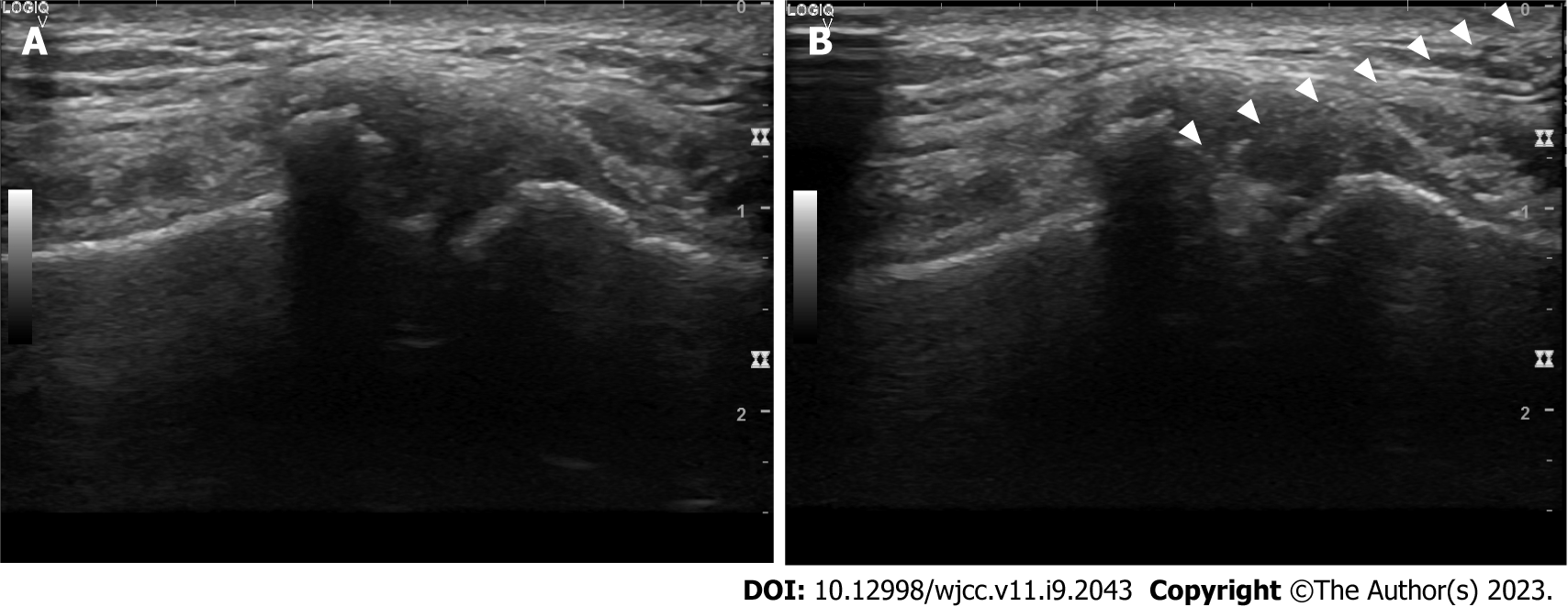
Before visiting our clinic, the patient received NSAIDs and local corticosteroid injections, but the pain did not improve significantly. Therefore, we performed ultrasound-guided IA corticosteroid injections into the MSJ. In the supine position, we prepared the skin of the anterior chest wall aseptically. Then, a 12-Hz linear transducer ultrasound probe was placed parallel to the midsternum to identify the MSJ[4]. We inserted a 25 G needle using ultrasound guidance and injected 1 mL of 0.375% ropivacaine and 2.5 mg dexamethasone into the MSJ (Figure 5). With IA corticosteroid injection, we prescribed NSAIDs.
After 1 wk of treatment, the pain was significantly relieved, decreasing from Numeric Rating Scale (NRS) 6 to NRS 3. Because the pain persisted after the injection, although it was relieved significantly, we performed another ultrasound-guided IA corticosteroid injection. Two weeks after the second injection, his symptoms improved from NRS 3 to NRS 2. However, the patient continued to experience discomfort in his anterior chest and requested an additional injection. Two weeks after this third injection, his pain had nearly resolved, and the patient did not revisit after the final injection. During follow-up, we recommended continuing the prescribed medication.
This case report is an account of a patient who complained of localized pain in the anterior chest and was diagnosed with AS on SPECT-CT. He experienced effective pain reduction after ultrasound-guided IA corticosteroid injections.
It is important to identify life-threatening diseases in a patient with chest pain, although such pain is benign in approximately 80% of cases, of which musculoskeletal chest pain accounts for almost 50%[5-8]. Musculoskeletal chest pain can be caused by a variety of factors, grouped into three categories of isolated musculoskeletal pain, rheumatic diseases, and non-rheumatic systemic causes. Even though critical causes of anterior chest pain might be ruled out, various diseases should be considered for differential diagnosis of benign anterior chest pain, such as costochondritis, Tietze syndrome (isolated musculoskeletal pain), fibromyalgia, RA, AS, septic arthritis, psoriatic arthritis (rheumatic disease), neoplasm, and osteoporotic fracture (non-rheumatic system causes)[9]. An MSJ problem is a possible cause of benign chest pains.
The MSJ is a complex joint between the manubrium and the body of the sternum[1]. This secondary cartilaginous joint (symphysis) may resemble a synovial joint susceptible to osteoarthritic degeneration, as 30% of patients undergo fibrocartilage disk absorption. Primary MSJ osteoarthritis (OA) has no identifiable etiology; secondary OA results from RA, AS, psoriatic arthritis, or gout[10]. In most cases, MSJ arthralgia due to secondary MSJ OA is accompanied by systemic symptoms, but it can be the main sign of systemic arthritis[11,12]. Our patient did not complain of systemic symptoms including back pain but only of anterior chest pain. Therefore, evaluation for systemic diseases should be considered when a patient complains of MSJ arthralgia even if there are no other symptoms.
AS is a systemic disease that can cause secondary OA of the MSJ and is a chronic inflammatory disease that mainly affects axial joints[13]. Baek et al[14] reported clinical features of AS in Korean patients, and chronic back pain was a presenting symptom in approximately 75% of AS patients. The most frequently affected extraspinal joints in AS are the hips and shoulders and are involved at presentation in up to 15% of cases. Other peripheral joint involvement presents in 10%-20% of patients. The proportion of patients with enthesis involvement at disease onset is about 1.5%[14]. The most characteristic clinical symptom of AS is inflammatory back pain. Pain and stiffness in the mid-thoracic or cervical region may be the initial symptom instead of the more common presentations of AS[15]. On the other hand, MSJ causing anterior chest pain is a rare presenting symptom[12,16]. In a retrospective study performed in 275 patients with spondyloarthritis, 37% experienced spondyloarthritis-associated chest pain[17]. However, anterior chest wall pain as the presenting symptom occurred in only 4%-6% of cases[18]. For this reason, it is difficult to suspect AS in patients with anterior chest pain, and diagnosis of AS can be delayed in patients with anterior chest pain.
The diagnosis of AS is based on radiologic evidence of sacroiliitis. Therefore, it may be essential to evaluate SIJ in patients with AS. Various physical examination tests have been advocated as diagnostic aids in patient with SIJ problems; however, reliability of SIJ provocation tests have been questioned[19,20]. Although the patient in this case had no symptom related to SIJ and SIJ provocation tests were negative, bilateral sacroiliitis was observed on MRI. Hence, if AS is suspected, imaging of SIJ should be performed even if there is no abnormality on physical examinations.
SPECT-CT offers functional information about increased bone turnover in combination with morphological details[21]. The modality can detect not only metastatic lesions but also benign lesions such as infective, inflammatory, or traumatic bony lesions[22]. The evidence base for the role of SPECT-CT in benign musculoskeletal pathology is emerging, and several studies have revealed the clinical significance of SPECT-CT in the diagnosis of benign musculoskeletal disease[23]. Some prospective studies suggested the usefulness of SPECT-CT as a diagnostic tool for benign musculoskeletal diseases[24,25]. In the present case, SPECT-CT revealed inflammatory arthritic change in the MSJ, although a simple X-ray showed normal findings. Likewise, in a patient complaining of pain in the focal area that is not easily determined with simple X-ray or other general imaging tests, SPECT-CT can be used as a diagnostic method. Since there are many structures in the thorax that can produce musculoskeletal pain such as the costoverterbral, sternocostal, costochondral, and MSJs, it is difficult to identify an exact lesion in the thorax. Considering this, SPECT-CT can be useful in locating the precise lesion in patients with musculoskeletal chest pain.
Oye et al[12] suggested anterior chest pain due to MSJ involvement as a presenting symptom of AS and MRI as a valuable diagnostic tool. MRI has been increasingly used as an imaging modality in patients with AS because of its capacity to identify both active inflammation and chronic structural changes in axial skeletal structures[26]. However, in patients with claustrophobia, pacemakers, or metal implant, use of MRI is limited[27]. SPECT-CT can be an alternative to MRI in these cases.
Systemic drugs like NSAIDs are the primary treatment of AS, but IA corticosteroid injections into the painful joint often satisfactorily ameliorate acute inflammatory pain[28]. Since the MSJ is a narrow space and it can be difficult to inject a corticosteroid, IA corticosteroid injection into the joint space can be performed more easily and accurately using ultrasound guidance. Therefore, in systemic diseases like AS, when symptoms are limited to specific joints, ultrasound-guided IA corticosteroid injections may be effective for pain relief.
Inflammatory arthritis including AS should be considered in patients complaining of anterior chest pain, and SPECT-CT can be helpful in differential diagnosis. Ultrasound-guided IA corticosteroid injections may be an effective treatment option.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: South Korea
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Chiu CD, Taiwan; Cure E, Turkey S-Editor: Li L L-Editor: Filipodia P-Editor: Li L
| 1. | Sebes JI, Salazar JE. The manubriosternal joint in rheumatoid disease. AJR Am J Roentgenol. 1983;140:117-121. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 22] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 2. | Vaishya R, Vijay V, Rai BK. Osteoarthritis of the Manubriosternal Joint: An Uncommon Cause of Chest Pain. Cureus. 2015;7:e370. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 3. | Ehara S. Manubriosternal joint: imaging features of normal anatomy and arthritis. Jpn J Radiol. 2010;28:329-334. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 8] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 4. | Cho JY, Park D. Ultrasound-Guided Corticosteroid Injection in a Patient With Tietze Syndrome Combined With Costochondral Joint Swelling. Am J Phys Med Rehabil. 2019;98:e71-e73. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 8] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 5. | Stochkendahl MJ, Christensen HW. Chest pain in focal musculoskeletal disorders. Med Clin North Am. 2010;94:259-273. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 48] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 6. | Klinkman MS, Stevens D, Gorenflo DW. Episodes of care for chest pain: a preliminary report from MIRNET. Michigan Research Network. J Fam Pract. 1994;38:345-352. [PubMed] |
| 7. | Svavarsdóttir AE, Jónasson MR, Gudmundsson GH, Fjeldsted K. Chest pain in family practice. Diagnosis and long-term outcome in a community setting. Can Fam Physician. 1996;42:1122-1128. [PubMed] |
| 8. | Verdon F, Herzig L, Burnand B, Bischoff T, Pécoud A, Junod M, Mühlemann N, Favrat B; GMIRG. Chest pain in daily practice: occurrence, causes and management. Swiss Med Wkly. 2008;138:340-347. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 9. | Winzenberg T, Jones G, Callisaya M. Musculoskeletal chest wall pain. Aust Fam Physician. 2015;44:540-544. [PubMed] |
| 10. | Mitchell TA, Alderete JF, Helsel BS. Manubriosternal arthrodesis: a novel surgical approach for refractory osteoarthritis. J Thorac Cardiovasc Surg. 2014;148:e232-e233. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 11. | Becker JA, Daily JP, Pohlgeers KM. Acute Monoarthritis: Diagnosis in Adults. Am Fam Physician. 2016;94:810-816. [PubMed] |
| 12. | Oye M, Ali AA, Wasserman PL, Kaeley GS, Thway M. Manubriosternal Joint Involvement as a Presenting Feature of Axial Spondyloarthritis. Cureus. 2021;13:e20527. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 13. | Elsaman AM, Hamed A, Radwan AR. Ultrasound-guided epidural block in axial spondyloarthritis patients with limited spine mobility: a randomized controlled trial. Korean J Pain. 2021;34:114-123. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 3] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 14. | Baek HJ, Shin KC, Lee YJ, Kang SW, Lee EB, Yoo CD, Song YW. Clinical features of adult-onset ankylosing spondylitis in Korean patients: patients with peripheral joint disease (PJD) have less severe spinal disease course than those without PJD. Rheumatology (Oxford). 2004;43:1526-1531. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 34] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 15. | Kim Y, Kim GT, Lee SG, Lee HN, Kang J, Ko TY. First Asian case of biopsy-confirmed manubriosternal joint involvement in rheumatoid arthritis. Z Rheumatol. 2020;79:389-392. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 16. | Wendling D, Prati C, Demattei C, Loeuille D, Richette P, Dougados M. Anterior chest wall pain in recent inflammatory back pain suggestive of spondyloarthritis. data from the DESIR cohort. J Rheumatol. 2013;40:1148-1152. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 24] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 17. | Ramonda R, Lorenzin M, Lo Nigro A, Vio S, Zucchetta P, Frallonardo P, Campana C, Oliviero F, Modesti V, Punzi L. Anterior chest wall involvement in early stages of spondyloarthritis: advanced diagnostic tools. J Rheumatol. 2012;39:1844-1849. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 18] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 18. | Elhai M, Paternotte S, Burki V, Durnez A, Fabreguet I, Koumakis E, Meyer M, Payet J, Roure F, Dougados M, Gossec L. Clinical characteristics of anterior chest wall pain in spondyloarthritis: an analysis of 275 patients. Joint Bone Spine. 2012;79:476-481. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 14] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 19. | Cohen SP. Sacroiliac joint pain: a comprehensive review of anatomy, diagnosis, and treatment. Anesth Analg. 2005;101:1440-1453. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 269] [Cited by in RCA: 263] [Article Influence: 13.2] [Reference Citation Analysis (0)] |
| 20. | Spadaro A, Iagnocco A, Baccano G, Ceccarelli F, Sabatini E, Valesini G. Sonographic-detected joint effusion compared with physical examination in the assessment of sacroiliac joints in spondyloarthritis. Ann Rheum Dis. 2009;68:1559-1563. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 35] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 21. | Bhure U, Roos JE, Pérez Lago MDS, Steurer I, Grünig H, Hug U, Strobel K. SPECT/CT arthrography. Br J Radiol. 2018;91:20170635. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 7] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 22. | Riaz S, Bashir H, Hassan A, Nawaz MK. Musculoskeletal Spect-Ct: A Pictorial Review. J Ayub Med Coll Abbottabad. 2016;28:427-437. [PubMed] |
| 23. | Saha S, Burke C, Desai A, Vijayanathan S, Gnanasegaran G. SPECT-CT: applications in musculoskeletal radiology. Br J Radiol. 2013;86:20120519. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 43] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 24. | Even-Sapir E, Flusser G, Lerman H, Lievshitz G, Metser U. SPECT/multislice low-dose CT: a clinically relevant constituent in the imaging algorithm of nononcologic patients referred for bone scintigraphy. J Nucl Med. 2007;48:319-324. [PubMed] |
| 25. | Linke R, Kuwert T, Uder M, Forst R, Wuest W. Skeletal SPECT/CT of the peripheral extremities. AJR Am J Roentgenol. 2010;194:W329-W335. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 55] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 26. | Zochling J, Baraliakos X, Hermann KG, Braun J. Magnetic resonance imaging in ankylosing spondylitis. Curr Opin Rheumatol. 2007;19:346-352. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 30] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 27. | Parghane RV, Singh B, Sharma A, Singh H, Singh P, Bhattacharya A. Role of (99m)Tc-Methylene Diphosphonate SPECT/CT in the Detection of Sacroiliitis in Patients with Spondyloarthropathy: Comparison with Clinical Markers and MRI. J Nucl Med Technol. 2017;45:280-284. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 28. | Golder W, Karberg K, Sieper J. Fluoroscopy-guided application of corticosteroids for local control of manubriosternal joint pain in patients with spondyloarthropathies. Clin Rheumatol. 2004;23:481-484. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 0.4] [Reference Citation Analysis (0)] |