Published online Mar 16, 2023. doi: 10.12998/wjcc.v11.i8.1847
Peer-review started: December 8, 2022
First decision: December 26, 2022
Revised: January 9, 2023
Accepted: February 7, 2023
Article in press: February 7, 2023
Published online: March 16, 2023
Processing time: 88 Days and 22 Hours
Breast abscess during lactation is a severe complication of acute mastitis, which can lead to discomfort, high fever, breast fistula, sepsis, septic shock, breast damage, disease persistence and frequent hospitalization. Breast abscesses may also lead the mother to discontinue breastfeeding, thereby harming the infant’s health. The predominant pathogenic bacteria are Staphylococcus aureus, Staphylococcus epidermidis and Streptococcus. The incidence of breastfeeding abscesses in breastfeeding women ranges between 4.0% and 11.0%. In cases of breast abscess, the rate of cessation of lactation is 41.0%. In instances of breast fistula, the rate of cessation of lactation is very high (66.7%). Furthermore, 50.0% of women with breast abscesses must be hospitalized and treated with intravenous antibiotics. Treatment includes antibiotics, abscess puncture and surgical incision and drainage. The patients suffer from stress, pain and easily induced breast scarring; the disease’s progression is prolonged and recurrent, interfering with infant feeding. Consequently, it is crucial to discover an adequate cure.
A 28-year-old woman with a breast abscess was treated with Gualou Xiaoyong decoction and painless breast opening manipulation 24 d after cesarean delivery. On the 2nd d of treatment, the patient’s breast mass was significantly reduced, the pain was significantly reduced, and the general asthenia was improved. All conscious symptoms disappeared after 3 d, breast abscesses faded after 12 d of treatment, inflammation images disappeared after 27 d, and normal lactation images were restored.
In treating breast abscesses during breastfeeding, the combination of Gualou Xiaoyong decoction and painless lactation provides a positive therapeutic impact. This disease’s treatment offers the advantages of a short course of treatment, no need to discontinue breastfeeding and the ability to rapidly mitigate symptoms, which can be used as a reference in clinical practice.
Core Tip: Breast abscess during lactation is a serious complication of acute mastitis, which can cause breast pain, fistula, sepsis, septic shock, breast destruction, disease persistence and discontinuation of lactation. Current treatment includes antibiotics, abscess puncture and surgical incision and drainage. Patients suffer from stress and discomfort, which readily induces breast scarring. Moreover, the disease’s progression is prolonged and recurrent, interfering with newborn feeding. This article described a case of breast abscess that was cured with Gualou Xiaoyong decoction combined with painless breast opening therapy. The advantages are a short treatment course, no trauma, inexpensive, lactation continuation and rapid symptom improvement.
- Citation: Jin LH, Zheng HL, Lin YX, Yang Y, Liu JL, Li RL, Ye HJ. Lactation breast abscess treated with Gualou Xiaoyong decoction and painless lactation manipulation: A case report and review of literature. World J Clin Cases 2023; 11(8): 1847-1856
- URL: https://www.wjgnet.com/2307-8960/full/v11/i8/1847.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i8.1847
The World Health Organization (WHO) recommends 6 mo of exclusive breastfeeding following delivery[1,2]. However, mothers are unable to implement exclusive breastfeeding for various reasons, leaving their infants susceptible to respiratory and gastrointestinal diseases. Furthermore, the risk of noncommunicable diseases in childhood and adulthood, such as heart disease, obesity, diabetes, cancer, allergies, asthma and chronic lung, liver, and kidney diseases, also increases[1,2]. A quarter of lactating mothers believe that acute mastitis during lactation is the primary cause of their decision to wean. It is reported that the incidence rate of mastitis among breastfeeding women is as high as 33%, of which approximately 11% will be secondary to breast abscess[3]. Breast abscesses severely impact the physical and mental health of breastfeeding women, leading to the cessation of breastfeeding (41.0%), breast fistula (11.1%), readmission (50.0%) and even permanent breast deformity[4]. Here, we presented a case of breast abscess in lactation that was successfully treated with Gualou Xiaoyong decoction combined with painless breast opening therapy. It has the advantages of quick symptom alleviation, a short treatment duration, non-invasive, economical and does not require the cessation of breastfeeding.
On August 31, 2022, a 28-year-old Chinese female was initially diagnosed as "24 d after cesarean section, 9 d after breast swelling and pain".
The cesarean section was conducted 24 d before the diagnosis, and the operation was without incident. During the 9 d preceding the diagnosis, the patient experienced breast pain, lethargy, little aversion to colds, nausea and vomiting. On August 27, 2022, an ultrasound test in another hospital reported: “Left breast hypoechoic area, BI-RADS category 3, consider inflammation, right breast hyperechoic mass, consider milk accumulation,” where BI-RADS is the abbreviation for Breast Imaging-Reporting and Data System. Oral consumption of Chinese medicine and cefuroxime axetil pills had no noticeable effect. On August 30, 2022, the other hospital conducted another ultrasound test that reported: “During lactation, several hypoechoic nodules were observed in the left breast, the larger ones were about 2.6 cm × 1.2 cm (in the direction of 8 o’clock) and 1.3 cm × 1.0 cm (in the direction of 10 o’clock), the shape was irregular, the edges were blurry, and fine light spots were detected inside, the imaging behind remained unchanged, and there was no impact on the surrounding tissues. Color Doppler Flow Imaging (CDFI); no blood flow signal was found inside, considering breast abscess, breast cyst with infection.” Under ultrasonography guidance, a fine needle puncture was performed, and 7 mL of purulent fluid was collected. The patient reported the pain and enlargement of both breasts to be excruciating. There was an absence of fever, but the patient experienced lethargy. The pain rating [visual analogue score (VAS) rating] was 7.
The patient reported no other known medical conditions or allergies.
The patient was a non-smoker and a non-drinker with no family history; she also denied any interaction within epidemic areas.
Body temperature was 37 °C, multiple 4 cm × 4 cm sized masses were palpable in the left breast, and a 10 cm × 7 cm sized mass was palpable in the right breast, with obvious tenderness. The breast skin on the surface of the left breast lump was dark and about 2 cm × 2 cm in size.
The white blood cell count (WBC) was 8.3 × 109/L, the neutrophil percentage was 69.8%, lymphocyte percentage was 22.8%, C-reactive protein (CRP) was 16.39 mg/L, procalcitonin (PCT) was 0.03 mg/L, and milk bacterial culture was positive for Staphylococcus epidermidis.
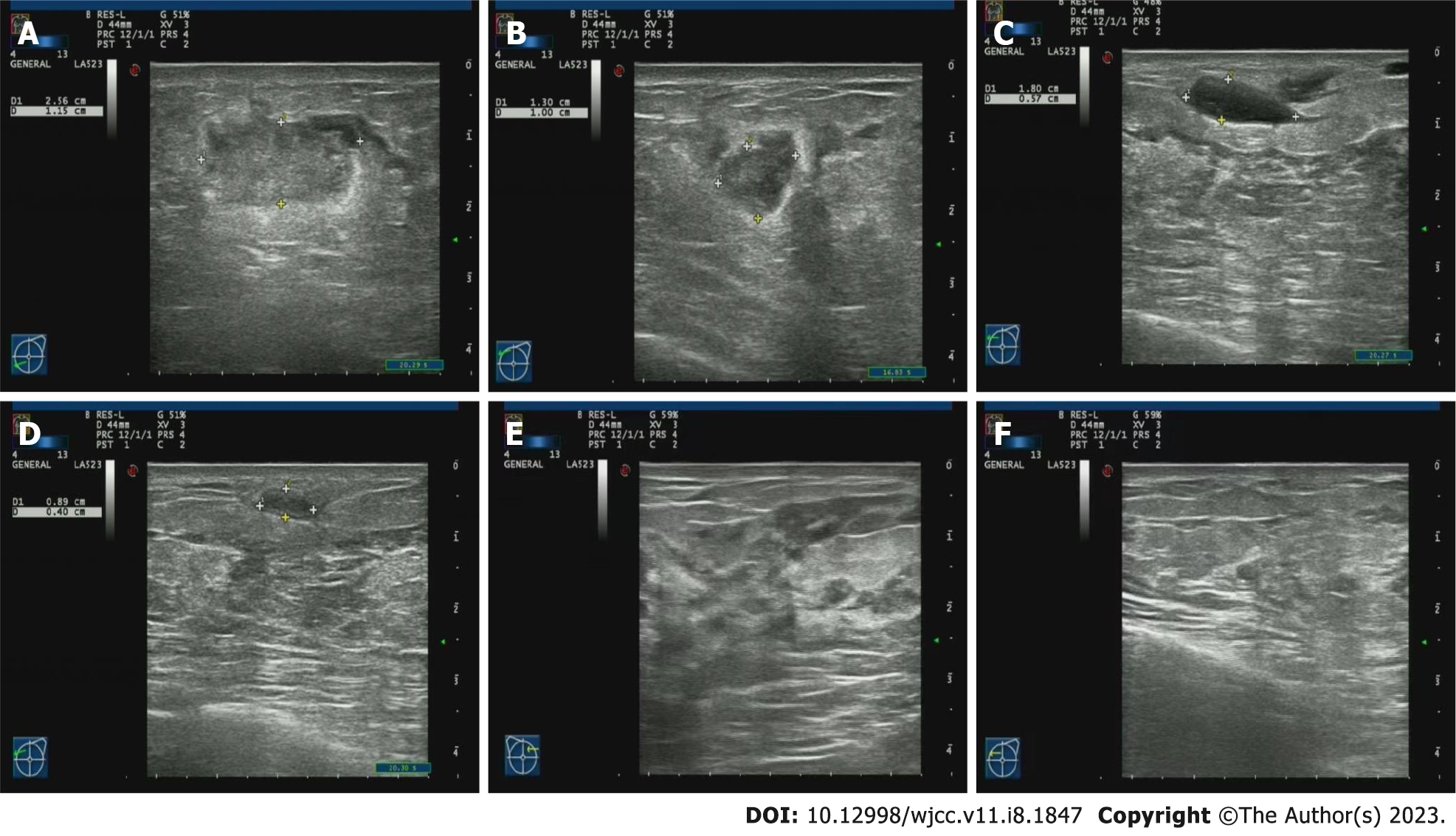
On August 30, 2022 in the lactating breast, several hypoechoic nodules were observed in the left breast. The larger nodules were about 2.6 cm × 1.2 cm (in the direction of 8 o’clock) and 1.3 cm × 1.0 cm (in the direction of 10 o’clock) (Figure 1A).The shape was irregular, the edge was fuzzy, and fine light spots were detected inside. CDFI revealed no blood flow signal inside, several cystic nodules were seen in the right breast, the largest nodule was 0.4 cm × 0.4 cm (in the direction of 10 o’clock) (Figure 1B), and the internal sound transmission was poor.
Cyst in right breast with infection and multiple abscesses in left breast.
Oral Gualou Xiaoyong decoction was given. The milk from the left breast contained hints of blood, while the milk color of the right breast was normal. It was recommended to stop breastfeeding on the left breast for 1 d and regularly use a breast pump to express the milk on the left side. Continuation of breastfeeding from the right breast was recommended.
Gualou Xiaoyong decoction consisted of: Chaihu 9 g; gualou skin 15 g; luffa complex 15 g; lobelia lobata 15 g; dandelion 15 g; paeonia rubra 15 g; tongcao 6 g; peach kernel 10 g; fried coix seed 30 g; chixiaodou 20 g; angelica sinensis 15 g; fried atractylodes macrocephala 15 g; arctium lappa 15 g; honeysuckle 20 g; forsythia suspensa 15 g; poria cocos 15 g; lulutong 10 g; angelica dahurica dahurica 15 g; and saponin 15 g. To prepare the decoction, 400 mL of the medicinal solution was boiled. The decoction was consumed at a lukewarm temperature, 200 mL in the morning and in the afternoon for a total of 5 doses.
Tanzhong, ruzhong, rugen, qimen, shaohai, chize, tianchi, tianxi, etc techniques can be used to massage the breast to remove the accumulated milk. Place the thumb and index finger of one hand at the junction of the black and white areola skin. Remove the front milk with the downward inward pressing method. Then apply massage oil to the hands, gently massage the milk block three times with the finger and towards to the nipple direction to discharge the milk. Massage each breast for 20-30 min using this method.
On the return visit on September 1, 2022 the general fatigue had disappeared, and the patient’s spirit improved significantly compared with the previous day. The swelling and pain of the left breast decreased significantly, and the pain of the right breast lump disappeared. The patient’s VAS was 0. The patient’s body temperature was 36.2 °C, and the left breast mass was significantly smaller than the previous day. Two hard masses with a size of about 2 cm × 2 cm were palpable, the skin was slightly red, and the right breast mass had disappeared. The patient received another painless lactation treatment, and no pyogenic milk was found in either breast. It was suggested that breastfeeding can be performed on both breasts. Another milk culture revealed Staphylococcus epidermidis.
On the follow-up visit on September 2, 2022 the swelling and pain of bilateral breasts mostly disappeared. The mass site on the left breast was slightly red, and there was no obvious fatigue or other discomforts. The patient’s VAS was 0. The routine blood examination revealed WBC of 5.0 × 109/L, neutrophil percentage of 64.3%, lymphocyte percentage of 27.2%, CRP of 4.79 and PCT of < 0.02 mg/L. The bacterial milk culture was positive for Staphylococcus epidermidis.
Another ultrasound was conducted on September 5, 2022. Several hypoechoic masses were seen in the left breast, with a larger size of about 1.8 cm × 0.6 cm (in the direction of 10 o’clock) (Figure 1C). On September 9, 2022, the breast swelling and pain were barely noticeable. A 2 cm × 2 cm mass and a 1 cm × 1 cm mass were palpable on the left breast. The tenderness was not obvious, and the skin was slightly red. Seven doses of Chinese medicine were prescribed.
On September 12, 2022, a repeat ultrasound revealed several hypoechoic masses in the left breast, with a larger size of about 0.9 cm × 0.4 cm (in the direction of 10 o’clock) (Figure 1D). A return visit on September 16, 2022 (which was 40 d after the cesarean section), revealed that the breast pain disappeared (VAS 0). The patient’s body temperature was 36.2 °C. A hard mass sized 1 cm × 1 cm was palpable in the left breast. No tenderness or color change were noticed. Seven more doses of Chinese medicine were prescribed.
At another return visit on September 23, 2022 (47 d after cesarean section), no breast pain or fatigue were reported (VAS 0). A mass sized 0.3 cm × 0.3 cm mass was palpable on the left breast, and it was soft and devoid of tenderness. The skin was not red. Five doses of traditional Chinese medicine were prescribed, and breast opening was performed once.
The ultrasound on September 27, 2022 revealed normal lactation (Figure 1E and F). At the return visit on September 30, 2022 (54 d after cesarean section), no discomfort such as breast swelling and pain were reported. The breast lump had disappeared, and there was no skin redness, swelling, heat or pain. However, the patient had a common cold with a sore throat and coughing. Seven doses of Chinese medicine were subsequently prescribed. On October 7, 2022, the cold was cured, and there was no breast swelling, pain or lump.
Due to repeated positive bacterial culture findings, two boxes of azithromycin tablets and seven doses of traditional Chinese medicine were added. The return visit on October 17, 2022 revealed that the patient had no discomfort such as breast pain, fever and fatigue. The bacterial culture from the milk revealed Staphylococcus epidermidis. The treatment cycle was terminated because the patient had no symptoms and the routine blood test, CRP, PCT, and B-ultrasound were normal. See Table 1 for the results of bacteria culture in the milk.
| Date | Before/after administration | Bacteria cultured in milk | Penicillin resistance | Cephalosporin resistance |
| August 31, 2022 | Before | Staphylococcus epidermidis | Yes | Yes |
| September 2, 2022 | After (Gualou Xiaoyong decoction) | Staphylococcus epidermidis | Yes | Yes |
| September 9, 2022 | After (Gualou Xiaoyong decoction) | Staphylococcus aureus | Yes | Yes |
| September 16, 2022 | After (Gualou Xiaoyong decoction) | Staphylococcus aureus | Yes | Yes |
| September 23, 2022 | After (Gualou Xiaoyong decoction) | Staphylococcus epidermidis | Yes | Yes |
| September 30, 2022 (combined with cold) | After (Gualou Xiaoyong decoction) | Staphylococcus aureus | Yes | Yes |
| October 7, 2022 (add 2 boxes of azithromycin tablets) | Before (azithromycin tablets) | Staphylococcus aureus | Yes | Yes |
| October 17, 2022 | After (azithromycin tablets) | Staphylococcus epidermidis | Yes | Yes |
After 2 mo of follow-up, the patient’s condition had not relapsed. The infant did not suffer from fever, abdominal pain, diarrhea, abdominal distension, nausea, vomiting and other adverse reactions.
For the first 6 mo of life, the WHO recommends exclusive breastfeeding. Acute mastitis and breast abscess during lactation are regarded as the leading causes of unintentional weaning, preventing mothers from implementing exclusive nursing. Acute mastitis during lactation is a form of breast cellulitis affecting the interlobular connective tissue. The WHO defines the disease as “a state of breast inflammation, which may or may not be accompanied by infection”[1,5], which may lead to breast abscess and septic fever[6], and may directly lead to the cessation of breastfeeding. The disease can elicit breast pain locally and is frequently accompanied by fast developing systemic symptoms, such as fever, muscular pain, chills and fatigue[4].
In severe cases, the breast may be permanently scarred, and its occurrence rate ranges from 3% to 33%, with 4% to 11% developing breast abscesses[3]. If any of the following criteria is met, it is diagnosed as acute mastitis during lactation: (1) Local redness of breast, with or without temperature rise; (2) Systemic inflammatory reaction, such as chills, headache and fatigue; (3) Body temperature greater than 37.3 °C or the results of routine blood tests showed that WBC or neutrophils increased or the level of CRP increased; and (4) Patients with positive milk culture[7]. Breast abscess is defined as a local infection with fluid accumulation in breast tissue[8]. A physical examination can generally detect the pain, erythema and stiffness of the breast abscess. However, it is not always simple to palpate the lump, especially if it is positioned deep within a larger breast. Imaging studies are beneficial for breast abscess diagnosis, determining whether there are several small abscesses or a single defined cavity and determining whether the abscesses are located or separated so as to assist in treatment plan formulation[9].
A severe complication of acute mastitis during breastfeeding is breast abscess. The disease is associated with patient fatigue, pressure, blockage of the mammary duct, inadequate feeding times, oral abnormalities of infants (such as cleft lip or palate), local milk stasis, malnutrition of mothers, use of a manual breast suction device, community-acquired infection, breast injury and poor diet, as well as delayed treatment of acute mastitis[10]. It is usually caused by Staphylococcus infection caused by pathogenic bacteria such as Streptococcus and/or Corynebacterium[11]. Breastfeeding discontinuation (41.0%), breast fistula (11.1%) and readmission (50.0%) are prevalent among patients with the disease[4,12]. In cases of breast abscess, the rate of cessation of nursing is 41.0%. In instances of breast fistula, the rate of cessation of nursing is very high (66.7%). In addition, 50% of postpartum Staphylococcus aureus breast abscess patients must be hospitalized again and administered intravenous antibiotics[12]. Consequently, the condition has a somewhat severe impact on mothers and infants and must be addressed promptly.
Breast abscess during lactation is often treated with antibiotics administered orally or intravenously, percutaneous aspiration (ultrasound-guided percutaneous puncture, fine needle puncture, vacuum-assisted biopsy, arthroscopic debridement and drainage, etc.[13-15]) and surgical incision and drainage[16] (Table 2). However, these procedures have limitations. Although antibiotics were empirically administered, it was later discovered that many isolated bacteria were antibiotic-resistant[17]; therefore, the potential threat of antibiotic resistance dramatically enhanced the need for alternative therapies.
| Ref. | Interventions | Population characteristics | Breastfeeding cessation rate | Outcome |
| Pileri et al[19], 2022 | B-ultrasound guided fine needle puncture | 13 of the 64 patients needed hospitalization, 4 cases of bilateral abscesses, 16 cases with the largest abscess diameter greater than 5 cm | The average breastfeeding time was 5 mo, and 40.6% of females with breast abscesses continued to breastfeed for more than 6 mo. 21 mothers stopped breastfeeding | All abscesses > 5 cm in diameter were positive for Staphylococcus aureus, 56% of which were antibiotic resistant. All patients received antibiotic treatment, 71.9% (46/64) of them underwent fine needle aspiration |
| Colin et al[29], 2019 | The same as above, if necessary, VAB shall be used | 92 lactating women, 105 abscesses in total, 82 of 92 patients (89%) had 1 abscess, 10 patients (11%) had 2 or more abscesses (range, 2-4 cm). 4 patients had bilateral abscesses | 18% of women stop breastfeeding | A total of 202 ultrasound-guided fine-needle puncture operations were performed. The number of percutaneous punctures/aspirates per abscess ranged from 1% to 6.4% of patients failed puncture and received incision and drainage surgery |
| Elagili et al[30], 2007 | The same as above, if necessary, abscessotomy shall be used | 16 (53.3%) non-lactating women and 14 (46.7%) lactating women had abscess diameters ranging from 1 cm to 15 cm (median: 4 cm). The volume of pus was between 1 mL and 200 mL (median: 14 mL) | Breastfeeding was encouraged, but rates of continuing or stopping breastfeeding were not recorded | 15 patients (50%) only needed one aspiration, 10 patients needed multiple aspiration, and 5 patients needed incision and drainage. Mean symptom duration was 11.63 d (range: 3-28 d) |
| Hagiya et al[31], 2014 | Operative incision and drainage | A 27-year-old Japanese female presented with high fever, tender breast, red and swollen left breast 17 d after delivery | Stopped breastfeeding | Ceftriaxone, daptomycin, vancomycin and other antibiotics were used for intravenous drip successively. Surgical incision was performed to drain about 15 mL of purulent secretion. The patient was discharged on the 10th d and took clindamycin orally |
| Wang et al[32], 2013 | VAB | 40 cases of lactation and 30 cases of non-lactation breast abscess who failed to use antibiotics and/or needle aspiration | Stopped breastfeeding during drainage | The skin inflammation disappeared within 6 d in all patients (median: 3.02 ± 6.65 d) |
| Kang and Kim[15], 2016 | Fine needle aspiration vs VAB | Fine needle aspiration in 25 patients with breast abscess and VAB in 19 patients with breast abscess | No information about breastfeeding | Compared with the VAB group, the cure rate of the needle aspiration group had no significant difference |
| Lou et al[13], 2022 | Arthroscopic system | 19 cases of breast abscess in lactation | 1 patient with breast fistula stopped breastfeeding, the other 18 patients resumed breastfeeding within 2 wk, of which 13 patients resumed breastfeeding within 1 wk | All patients were cured and did not recur during the 6-mo follow-up period. 1 patient stopped breastfeeding due to milk fistula, and the rest were cured |
Li et al[18] found 1222 cases of Staphylococcus aureus (82.5%) in 1481 cases of breast abscess in lactation by bacterial culture of abscess puncture fluid. Among them, 962 cases (65.0%) were methicillin-susceptible Staphylococcus aureus, 260 cases (17.6%) were methicillin-resistant Staphylococcus aureus, and 20 cases (1.4%) were Staphylococcus epidermidis. Drug sensitivity and resistance were analyzed in 260 strains of MRSA. It was found that 100% of MRSA was resistant to penicillin, amoxicillin clavulanate and cephalosporins, 45.0% of MRSA was resistant to tetracycline, 85.0% of MRSA was resistant to clindamycin, and 82.9% of MRSA was resistant to erythromycin. In most instances, when bacterial milk culture and drug sensitivity tests were performed for patients with breastfeeding mastitis and breast abscess, it was found that these bacteria were resistant to penicillin and cephalosporin antibiotics. Therefore, the actual therapeutic effect of antibiotics was poor.
Percutaneous aspiration, surgical incision and drainage are all surgical procedures. They have the following side effects: Influence of anesthesia on milk; separation of mother and baby; high cost; trauma and pain of patients; cessation of breastfeeding; and leaving local scars on the breast, etc[19]. Therefore, the development of traditional Chinese medicine and traditional Chinese medicine therapy is recommended. In this instance, the combination of Gualou Xiaoyong decoction and painless breast opening manipulation resulted in favorable clinical outcomes for the treatment of breast abscess in lactation.
The Program Committee of the International Society of Nursing Medicine advises moms with breast abscesses to continue breastfeeding because there is no evidence that healthy breastfed infants are at risk when their mothers are infected (Amir and the Program Committee of the Society of Breastfeeding Medicine, 2014). In this case, we recommended temporary cessation of breastfeeding from one breast for 1 d when the patient discovered pus in the milk. We recommended that the patient continue breastfeeding in the subsequent treatment process. We believe that continued breastfeeding can reduce breast milk stasis, which is conducive to disease recovery, and infants have received sufficient breast milk nutrition during this practice as we have not found adverse effects in previous cases. In this case, there was also no adverse reaction of the infant, such as nausea, vomiting, abdominal pain, abdominal distension, diarrhea, fever, etc.
Postpartum breast abscess is a common and intractable disease in clinical practice. In this case, the patient received a non-invasive treatment. On the 2nd d of treatment, the breast mass of the patient was significantly reduced, the pain was significantly reduced, and the general asthenia was improved. All conscious symptoms disappeared after 3 d, the breast abscess disappeared after 12 d of treatment, and the inflammation imaging disappeared after 27 d of treatment. It was a relatively short treatment cycle for the treatment of breast abscess, and our treatment method was not traumatic. We only needed outpatient oral drug treatment, the patient did not need hospitalization and surgery, and she had no pain.
Pileri et al[19] and others reported that fine needle puncture was effective in the treatment of breast abscess. However, it often required multiple puncture treatments, and patients felt pain and trauma and often needed antibiotic treatment. However, through milk culture, we found that most of the bacteria in the milk were Staphylococcus and Streptococcus. These bacteria are often resistant to antibiotics (penicillin and cephalosporins) that could be used during lactation, so it is ineffective to use these two types of antibiotics. Aminoglycoside or quinolone antibiotics are often sensitive to this kind of bacteria, but these two kinds of drugs are not suitable for lactating women.
Through our clinical observation, we found that traditional Chinese medicine has a definite effect on the treatment of lactating mastitis and breast abscess. First, the patients with breast abscesses are still in lactation, and the milk continuously secreted by the breast will aggravate the breast abscess. Therefore, good lactation techniques are needed to solve the problem of milk stasis. Secondly, the traditional Chinese medicine Gualou Xiaoyong decoction has a good clinical effect through our clinical observation. After our clinical observation of more than 100 cases of lactation mastitis and 4 cases of breast abscess, we found that after the use of Gualou Xiaoyong decoction and painless lactation manipulation, the breast lump and pain of the patients disappeared quickly, the skin redness disappeared, the body temperature returned to normal, the WBC and the percentage of neutrophils returned to normal, and the changes of mastitis and breast abscess disappeared under B-ultrasound.
In the treatment of this case, after the patient’s clinical symptoms subsided and the routine blood routine work, CRP, PCT and ultrasound returned to normal, the bacteria in the milk were still cultured (Staphylococcus aureus and Staphylococcus epidermidis were alternately cultured), leading us to hypothesize that there may be a disparity between the types and numbers of bacteria infecting the breast and the severity of the disease.
Carmichael and Dixon[20] and Fetherston[21] also reported that there was an inconsistency between the bacterial load and the severity of lactation mastitis and breast abscess. Compared to the infection itself, the immune system response to injury appeared to correlate more strongly with the severity of the sickness, and the bacteria were not sufficient to cause the disease on their own. In addition, mastitis is frequently characterized by an absence of dangerous bacteria, prompting some clinical researchers to suggest the terms “infectious” and “non-infectious” mastitis[22,23]. Many women with potentially harmful bacteria on their skin or breast milk will not develop mastitis. However, many mastitis-afflicted mothers do not have pathogenic bacteria in their milk[3]. It was expected that the recent Cochrane systematic review emphasized the uncertainty around the use of antimicrobial medicines in the treatment of mastitis in light of these findings. Therefore, the prophylactic use of antibiotics to prevent mastitis is ineffective[24], and there is not enough evidence to support the use of antibiotics to treat mastitis and breast abscesses[24]. According to some researchers, the host’s inflammatory mediators are the primary cause of mastitis, and these same inflammatory mediators may contribute to inadequate breastfeeding in clinical and subclinical mastitis[25].
Gualou Xiaoyong decoction is an often-prescribed treatment regimen in our department. It has a highly effective clinical effect in the treatment of lactation mastitis and lactation breast abscesses. It is composed of the following drugs: Bupleurum chinense, pericarpium trichosanthis, fructus arctii, luffa, lobelia, dandelion, red peony root, herb, peach kernel, coix seed, red bean, angelica, fried atractylodes macrocephala, honeysuckle and forsythia suspensa. In the prescription, bupleurum and trichosanthes peel are used to soothe the liver and regulate qi. Stir fried atractylodes macrocephala with bran strengthens the spleen and stomach. Arctium lappa L, scutellaria barbata L, dandelion, honeysuckle, forsythia suspensa L, angelica, paeonia lactiflora and peach kernel cool the blood, nourish the blood, promote blood circulation and remove blood stasis. Coix seed and adzuki bean detoxify and discharge pus. The entire prescription has the effects of soothing the liver and stomach, dispersing phlegm, softening the body, eliminating heat, detoxification and pus and dredging the breast.
Wu et al[26] studied the Trichosanthes and Arctium decoction (containing 12 Chinese medicines, including trichosanthes kirilowii, arctium fruit, trichosanthes root, scutellaria baicalensis, cape jasmine, forsythia, honeysuckle, licorice, dried tangerine peel, green tangerine orange peel, radix bupleuri, which are similar to the Gualou Xiaoyong decoction in this study), and found that quercetin, luteolin, fisetin, kaempferol and urushiflavin are the main active ingredients. Quercetin has anti-inflammatory, antioxidant and antifungal properties and can inhibit nuclear factor-kappa B (NF-κB) signaling pathway to enhance the transcriptional activity of NRF2-ARE, thus playing a role in controlling bovine mastitis. It can reduce the expression of inducible nitric oxide synthase and regulate the production of inflammatory precursor nitric oxide.
Luteolin has a significant systemic anti-inflammatory effect. It can regulate the toll-like receptor 2 and toll-like receptor 4 signal pathways induced by Staphylococcus aureus and inhibit IκBα and NF-κB. The phosphorylation of BP65 regulates the expression of matrix metallopeptidase 2 and matrix metal
Kaempferol can reduce interleukin 6, tumor necrosis factor and the expression of ANGPTL2 in cells to prevent the occurrence of mastitis in mice. It can inhibit NF-κB phosphorylation and the BP65 subunit IκBα, thus playing a therapeutic role in mastitis. Urushiflavin has a good anti-inflammatory effect on nephritis, endometritis and airway inflammation in vivo and inflammatory skin disease in vitro. Ye et al[27] found that the extract from scutellaria baicalensis georgi-safflower-dandelion-honeysuckle had a dose-dependent antibacterial effect on Staphylococcus aureus, Escherichia coli and Streptococcus agalactis.
Milk buildup is a significant factor in the incidence of mastitis during breastfeeding. The collected milk not only causes breast pain and discomfort and a decrease in milk volume but is also an excellent medium for bacterial growth, exacerbating and recurring breast inflammation[28]. Therefore, it is essential to empty the breast entirely. The non-painful breast opening method has a speedy impact, and the patient experiences no discomfort or negative effects. This technique combines the massage of distant acupoints along the meridians with local breast massage, which has a positive effect on breast opening. With the help of the Gualou Xiaoyong decoction, it can soothe the liver and stomach, expel phlegm, soften and firm the body, clear away heat, detoxify and expel pus and promote lactation. The patients’ clinical symptoms greatly decrease and diminish within a short time. The total amount of leukocytes, neutrophils, CRP, PCT and other inflammatory markers rapidly return to normal, and the flaky, low-echo region of the breast dissipates rapidly with ultrasound. Therefore, we consider this method to be a superior means of treating the disease and deserving of further clinical investigation.
The combination of Gualou Xiaoyong decoction and painless breast opening manipulation has a positive clinical effect on breast abscess during lactation and has the advantages of a short treatment course, no effect on milk secretion, no effect on breastfeeding, no toxic side effects and no pain for patients. This method is worthy of further investigation.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Mao ZM, China; Watanabe T, Japan S-Editor: Fan JR L-Editor: Filipodia P-Editor: Fan JR
| 1. | World Health Organization (WHO). Global strategy for infant and young child feeding. Geneva: WHO, 2003. Available from: https://www.who.int/. |
| 2. | NHMRC. Infant Feeding Guidelines. Canberra: National Health and Medical Research Council; 2012. |
| 3. | World Health Organization (WHO). Mastitis: Causes and management. Geneva, Switzerland: WHO, 2000. Available from: https://www.who.int/. |
| 4. | Ingman WV, Glynn DJ, Hutchinson MR. Inflammatory mediators in mastitis and lactation insufficiency. J Mammary Gland Biol Neoplasia. 2014;19:161-167. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 55] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 5. | Foxman B, D'Arcy H, Gillespie B, Bobo JK, Schwartz K. Lactation mastitis: occurrence and medical management among 946 breastfeeding women in the United States. Am J Epidemiol. 2002;155:103-114. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 192] [Cited by in RCA: 181] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 6. | Patel SH, Vaidya YH, Patel RJ, Pandit RJ, Joshi CG, Kunjadiya AP. Culture independent assessment of human milk microbial community in lactational mastitis. Sci Rep. 2017;7:7804. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 89] [Cited by in RCA: 120] [Article Influence: 15.0] [Reference Citation Analysis (0)] |
| 7. | Li D, Li J, Yuan Y, Zhou J, Xiao Q, Yang T, Li Y, Jiang L, Gao H. Risk factors and prognosis of acute lactation mastitis developing into a breast abscess: A retrospective longitudinal study in China. PLoS One. 2022;17:e0273967. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 8] [Reference Citation Analysis (0)] |
| 8. | Haifeng G, Yi Z, Ying C, Xin L, Yan L, Songtao D, Yajun G, Xiangping H, Si C, Xingxing L. Exploring the Efficacy of Comprehensive Management of Breast Abscesses in Restoring Milk Volume. J Hum Lact. 2022;38:171-176. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 9. | Jackson VP. The role of US in breast imaging. Radiology. 1990;177:305-311. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 175] [Cited by in RCA: 154] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 10. | Spencer JP. Management of mastitis in breastfeeding women. Am Fam Physician. 2008;78:727-731. [PubMed] |
| 11. | Lawrence RA, Lawrence RM. Breastfeeding: a guide for the medical profession. 6th ed. St. Louis: Elsevier Mosby, 2005. |
| 12. | Branch-Elliman W, Lee GM, Golen TH, Gold HS, Baldini LM, Wright SB. Health and economic burden of post-partum Staphylococcus aureus breast abscess. PLoS One. 2013;8:e73155. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 23] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 13. | Lou L, Ma W, Liu X, Shen H, Wang H, Lv H. Application of arthroscopic system in the treatment of lactational breast abscess. BMC Surg. 2022;22:397. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 15. | Kang YD, Kim YM. Comparison of needle aspiration and vacuum-assisted biopsy in the ultrasound-guided drainage of lactational breast abscesses. Ultrasonography. 2016;35:148-152. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 16. | Lam E, Chan T, Wiseman SM. Breast abscess: evidence based management recommendations. Expert Rev Anti Infect Ther. 2014;12:753-762. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 46] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 17. | Chuwa EW, Wong CM, Tan YY, Hong GS. MRSA breast abscesses in postpartum women. Asian J Surg. 2009;32:55-58. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 18. | Li Y, Ma XJ, He XP. Clinical characteristics of lactational breast abscess caused by methicillin-resistant Staphylococcus aureus: hospital-based study in China. Int Breastfeed J. 2021;16:80. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 19. | Pileri P, Sartani A, Mazzocco MI, Giani S, Rimoldi S, Pietropaolo G, Pertusati A, Vella A, Bazzi L, Cetin I. Management of Breast Abscess during Breastfeeding. Int J Environ Res Public Health. 2022;19. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 20. | Carmichael AR, Dixon JM. Is lactation mastitis and shooting breast pain experienced by women during lactation caused by Candida albicans? Breast. 2002;11:88-90. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 21. | Fetherston C. Mastitis in lactating women: physiology or pathology? Breastfeed Rev. 2001;9:5-12. [PubMed] |
| 22. | Thomsen AC, Espersen T, Maigaard S. Course and treatment of milk stasis, noninfectious inflammation of the breast, and infectious mastitis in nursing women. Am J Obstet Gynecol. 1984;149:492-495. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 142] [Cited by in RCA: 108] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 23. | Thomsen AC, Hansen KB, Møller BR. Leukocyte counts and microbiologic cultivation in the diagnosis of puerperal mastitis. Am J Obstet Gynecol. 1983;146:938-941. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 51] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 24. | Crepinsek MA, Taylor EA, Michener K, Stewart F. Interventions for preventing mastitis after childbirth. Cochrane Database Syst Rev. 2020;9:CD007239. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 11] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 25. | Jahanfar S, Ng CJ, Teng CL. Antibiotics for mastitis in breastfeeding women. Cochrane Database Syst Rev. 2013;CD005458. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 33] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 26. | Wu Z, Yang Q, Ma H. Study the Mechanism of Gualou Niubang Decoction in Treating Plasma Cell Mastitis Based on Network Pharmacology and Molecular Docking. Biomed Res Int. 2022;2022:5780936. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 4] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 27. | Ye D, Sun J, Li Y. Evaluation of Toxicity, Bacteriostatic, Analgesic, Anti-Inflammatory, and Antipyretic Activities of Huangqin-Honghua-Pugongying-Jinyinhua Extract. Vet Sci. 2021;8. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 5] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 28. | Omranipour R, Vasigh M. Mastitis, Breast Abscess, and Granulomatous Mastitis. Adv Exp Med Biol. 2020;1252:53-61. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 23] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 29. | Colin C, Delov AG, Peyron-Faure N, Rabilloud M, Charlot M. Breast abscesses in lactating women: evidences for ultrasound-guided percutaneous drainage to avoid surgery. Emerg Radiol. 2019;26:507-514. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 17] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 30. | Elagili F, Abdullah N, Fong L, Pei T. Aspiration of breast abscess under ultrasound guidance: outcome obtained and factors affecting success. Asian J Surg. 2007;30:40-44. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 33] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 31. | Hagiya H, Shiota S, Sugiyama W, Otsuka F. Postpartum breast abscess caused by community-acquired methicillin-resistant Staphylococcus aureus in Japan. Breastfeed Med. 2014;9:45-46. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 32. | Wang K, Ye Y, Sun G, Xu Z. The Mammotome biopsy system is an effective treatment strategy for breast abscess. Am J Surg. 2013;205:35-38. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 7] [Article Influence: 0.6] [Reference Citation Analysis (0)] |