Published online Mar 16, 2023. doi: 10.12998/wjcc.v11.i8.1830
Peer-review started: December 15, 2022
First decision: January 17, 2023
Revised: February 25, 2023
Accepted: February 22, 2023
Article in press: February 22, 2023
Published online: March 16, 2023
Processing time: 82 Days and 2.4 Hours
Vascular injury during thoracoscopic surgery for esophageal cancer is a rare but life-threatening complication that can lead to severe hypotension and hypoxemia. Anesthesiologists need to provide rapid and effective treatment to save patients' lives.
A 54-year-old male patient was scheduled to undergo a thoracoscopic-assisted radical resection of esophageal cancer through the upper abdomen and right chest. While dissociating the esophagus from the carina through the right chest, unexpected profuse bleeding occurred from a suspected pulmonary vascular hemorrhage. While the surgeon attempted to achieve hemostasis, the patient developed severe hypoxemia. The anesthesiologist implemented continuous positive airway pressure (CPAP) using a bronchial blocker (BB), which effectively improved the patient’s oxygenation and the operation was completed success
CPAP using a BB can resolve severe hypoxemia caused by accidental injury of the left inferior pulmonary vein during surgery.
Core Tip: Although hypoxemia caused by pulmonary vein injury is a rare complication, it is life-threatening. We report such a rare case, successfully managed by continuous positive airway pressure using a bronchial blocker. We hope that this case report helps other specialists to promptly manage similar incidents and avoid treatment delays and death.
- Citation: Zhou C, Song S, Fu JF, Zhao XL, Liu HQ, Pei HS, Guo HB. Continuous positive airway pressure for treating hypoxemia due to pulmonary vein injury: A case report. World J Clin Cases 2023; 11(8): 1830-1836
- URL: https://www.wjgnet.com/2307-8960/full/v11/i8/1830.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i8.1830
The esophagus is adjacent to major blood vessels such as the aorta and pulmonary vessels. Injury to these blood vessels during thoracoscopic surgery for esophageal cancer is a rare but life-threatening complication[1], which can lead to severe hypotension and hypoxemia. Thus, anesthesiologists need to provide rapid and effective treatment to save the affected patient’s life. Here, we report a special case wherein the surgeon accidentally injured the left inferior pulmonary vein while dissociating the esophagus during thoracoscopic surgery for esophageal cancer. The patient developed severe hypoxemia during hemostasis. Continuous positive airway pressure (CPAP) was administered through a bronchial blocker (BB), significantly improving oxygenation, and thereby preventing life-threatening complications.
A 54-year-old man undergoing elective resection of esophageal cancer.
The patient was diagnosed with middle thoracic esophageal cancer in January 2022 after presenting to the hospital with dysphagia. He underwent two cycles of neoadjuvant chemotherapy and was scheduled for esophageal cancer resection.
The patient had no previous history of any major illness and no other underlying illnesses.
The patient denied any family or genetic history of similar diseases.
173 cm tall, weighing 72 kg, ASA II.
The patient’s laboratory test results, including the full blood count and liver and renal function tests, were normal.
Electronic gastroscope results: Canker-like new organisms were observed 30-37 cm away from the local incisors. Pathology results: Squamous cell carcinoma. Chest computed tomography results: Thickening of the middle and lower esophageal wall.
The patient was scheduled to undergo thoracoscopic-assisted radical resection of esophageal cancer through the upper abdomen and right chest. The abdominal operation was successful, after which the patient was placed in the supine position on his left side, and a BB was inserted into the right main bronchus. While dissociating the esophagus from the carina through the right chest, unexpected profuse bleeding occurred, which resulted in an emergency thoracotomy due to a possible pulmonary vascular hemorrhage. The rate of blood loss from an unknown source was approximately 1000 mL/3 min.
After finger pressure suppressed the bleeding, the surgeon dissected the structures around the bleeding source with the aid of video-assisted thoracoscopy. Rapid fluid replacement and vasoactive drugs were administered to maintain blood pressure, along with other treatments, while 2 units of red blood cells were being prepared.
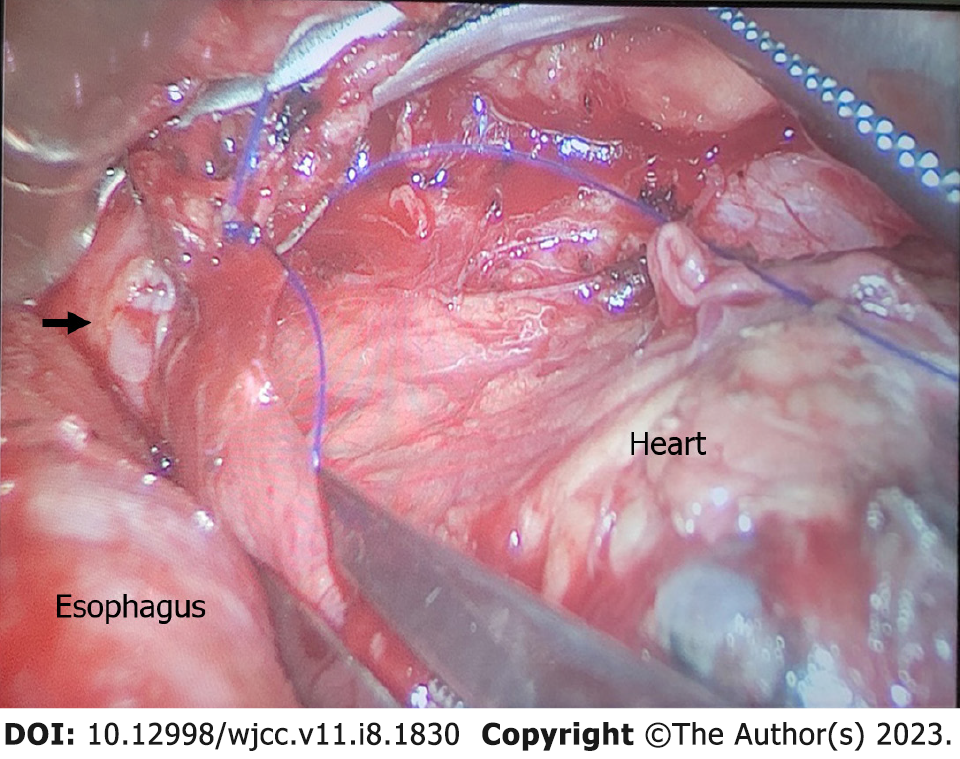
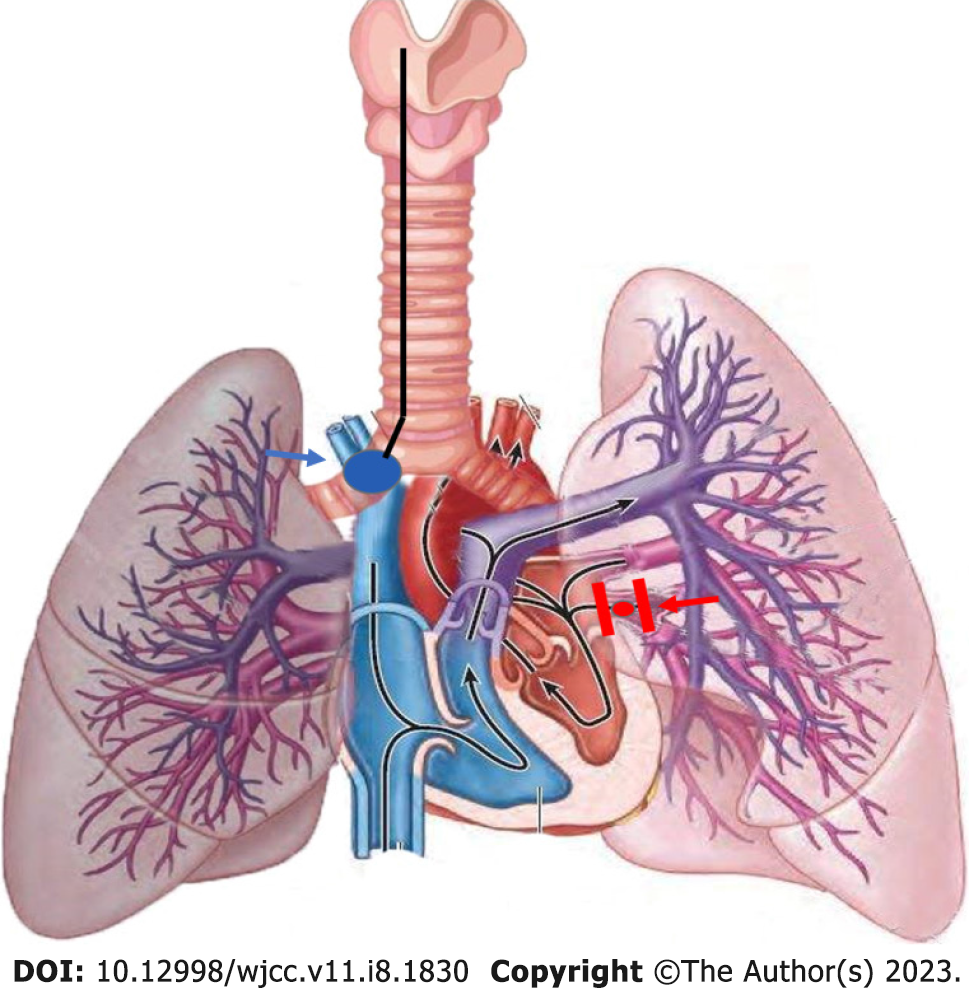
Following dissection, the surgeon clamped both ends of the ruptured blood vessel in preparation for suturing (Figure 1). Following vascular occlusion, the patient's pulse oxygen saturation (SpO2) suddenly decreased from 97% to 87% over 5 min, followed by a further decrease from 87% to 66% over the next 10 min (Table 1). We quickly ruled out possible anesthesia-related factors, including the respiratory circuit falling off and BB displacement. Manual ventilation was concurrently initiated to increase the respiratory rate and improve blood oxygenation. Additionally, correct BB positioning was confirmed using a fiberoptic bronchoscope (Figure 2). The surgeon confirmed that the rupture was located in the left inferior pulmonary vein, thereby identifying the cause of the patient's hypoxemia. The patient's respiratory status was as follows: the right lung was unable to complete gas exchange as there was blood flow without ventilation during the time in which the BB was inserted into the right main bronchus; whilst for the left lung, only the upper lobe could complete gas exchange as the lower lobe was ventilated without blood flow while the left lower pulmonary vein was clamped (Figure 3).
| Immediately after blocking the pulmonary vein | 5 min after blocking the pulmonary vein | 10 min after blocking the pulmonary vein, start CPAP | 5 min after CPAP | 25 min after CPAP | |
| SpO2, % | 97 | 87 | 66 | 84 | 90 |
| PaO2 (mmHg) | - | - | - | 63.4 | 79.2 |
| PaCO2 (mmHg) | - | - | - | 63.2 | 71 |
| PETCO2 (mmHg) | 34 | 32 | 39 | 31 | 43 |
Hypoxemia secondary to injury of the left inferior pulmonary vein during thoracoscopic surgery for esophageal cancer.
There was a challenge: If the clamp was released, the blood supply to the left lung would be restored, allowing the patient to be ventilated; however, bleeding would resume. Due to the position of the rupture on the left side of the protuberance, ventilation of the right lung would affect the surgeon’s ability to conduct the operation.
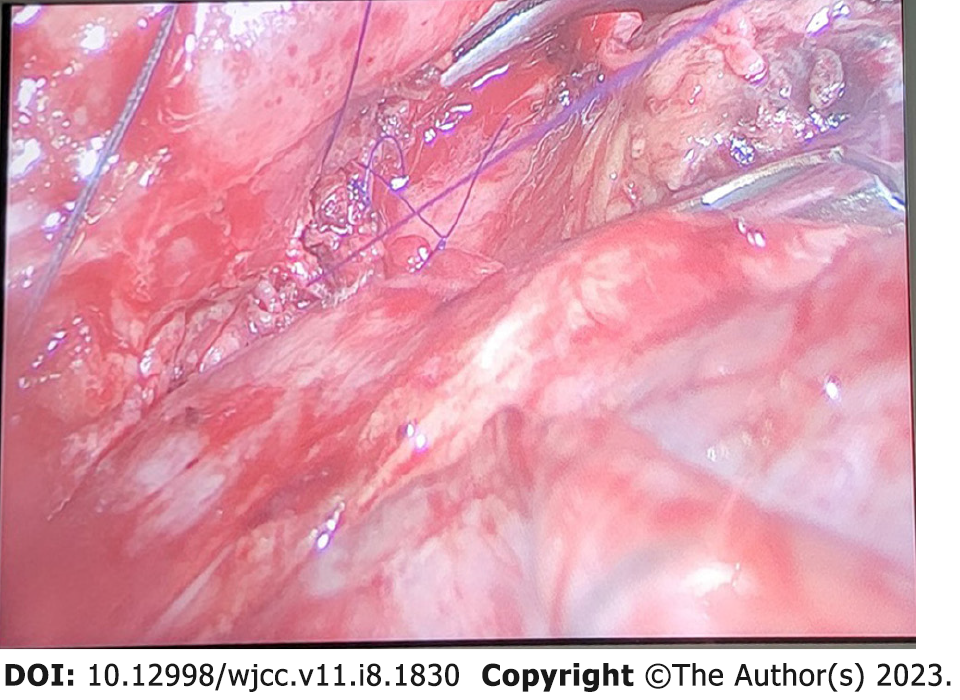
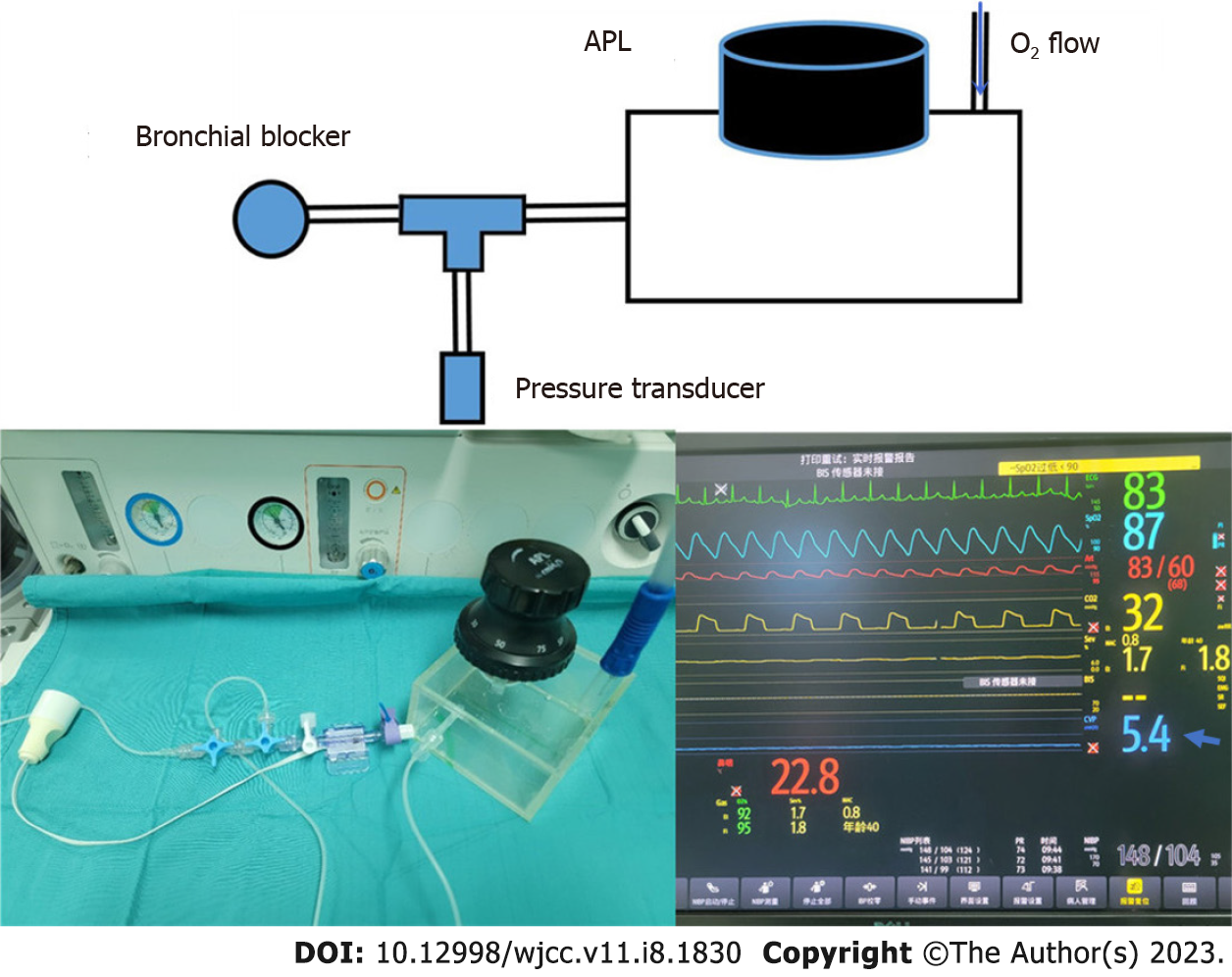
After consultation, we decided to administer 5 mmHg CPAP to the right lung to improve oxygenation by precisely controlling the CPAP pressure through the BB suction hole. After administering CPAP, the patient's SpO2 increased gradually, from 66% to 84% over 5 min, and the blood SpO2 gradually increased to 90%. After the patient was stabilized, the surgeon anastomosed the blood vessels (Figure 4) and the patient underwent ventilation for both lungs. The respiratory parameters were then adjusted, and the end tidal carbon dioxide decreased to 33 mmHg, with a partial pressure of carbon dioxide in the artery (PaCO2) of 40 mmHg.
The endotracheal tube was removed 15 min after surgery and the patient was discharged seven days later with no further complications.
In the present case, common hypoxemia management methods would not have been able to improve the patient's oxygenation levels (Table 2). Although the use of CPAP through a BB to treat hypoxemia during one-lung ventilation has been reported[2,3], a system to monitor and accurately adjust CPAP pressure in real time has not been reported. This case required accurate control of CPAP pressure due to the fact that excessively low CPAP pressure would not have improved oxygenation and excessively high CPAP would have caused lung expansion, affecting the surgical procedure[4]. The anesthetic machine APL valve was used for pressure adjustment and a pressure sensor was added to continuously monitor the CPAP in real-time (Figure 5).
| Ensure that FiO2 = 1 | Already used, but unable to improve |
| Check BB position with a fiberoptic bronchoscope | Already used, but unable to improve |
| Ensure optimal cardiac output and reduce volatile anesthetics (< 1MAC) | Already used, but unable to improve |
| Apply recruitment maneuver to the ventilated lung | Already used, but unable to improve |
| Apply PEEP (5 cmH2O) to the ventilated lung | Already used, but unable to improve |
| Perform intermittent re-expansion on the non-ventilated lung | Unable to apply |
| Mechanically restrict blood flow of the non-ventilated lung | Unable to apply |
During vascular anastomosis, only the left upper lobe of the lung could exchange gas. The decrease in the lung ventilation area leads to an increased PaCO2 and a higher level of PaCO2 than the pressure of endtidal CO2. Foreseeing this possibility, we closely monitored the patient’s vital signs and increased the frequency of blood gas analyses. Patients with pulmonary artery occlusion or severe chronic obstructive pulmonary disease may have similar problems[5,6]. After completion of vascular anastomosis, the patient was adequately ventilated, releasing CO2, and his PaCO2 returned to normal when he awoke.
We believe that the blood supply of the left lower lobe bronchial artery is involved in oxygenation. The lung has a dual blood supply from the bronchial and pulmonary arteries. The bronchial artery generally originates from the thoracic aorta or aortic arch, with two left and right sides, and supplies all bronchus levels above the respiratory bronchus, anastomosing with the capillaries at the end of the pulmonary artery. The bronchial artery accounts for 1%-3% of the pulmonary blood supply[7]. If the left inferior pulmonary vein is blocked, the bronchial artery blood supply may increase and significantly contribute to oxygenation. This has been confirmed in patients with bronchiectasis and other diseases[8].
In conclusion, precise CPAP implementation using a BB could effectively treat severe hypoxemia due to accidental injury of the left inferior pulmonary vein during resection of esophageal cancer.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Anesthesiology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Dilek ON, Turkey; Hu JW, China; Tsujinaka S, Japan S-Editor: Liu JH L-Editor: A P-Editor: Liu JH
| 1. | Javed A, Pal S, Chaubal GN, Sahni P, Chattopadhyay TK. Management and outcome of intrathoracic bleeding due to vascular injury during transhiatal esophagectomy. J Gastrointest Surg. 2011;15:262-266. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 2. | Benumof JL, Gaughan S, Ozaki GT. Operative lung constant positive airway pressure with the Univent bronchial blocker tube. Anesth Analg. 1992;74:406-410. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 16] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 3. | Sasano H, Sasano N, Ito S, Fujita Y, Sugiura T, Morita M, Sobue K. Continuous positive airway pressure applied through a bronchial blocker as a treatment for hypoxemia due to stenosis of the left main bronchus. Anesthesiology. 2009;110:1199-1200. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 4. | El-Tahan MR, Doyle DJ, Hassieb AG. High-frequency jet ventilation using the Arndt bronchial blocker for refractory hypoxemia during one-lung ventilation in a myasthenic patient with asthma. J Clin Anesth. 2014;26:570-573. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 5. | Ward KR, Yealy DM. End-tidal carbon dioxide monitoring in emergency medicine, Part 2: Clinical applications. Acad Emerg Med. 1998;5:637-646. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 50] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 6. | Kartal M, Goksu E, Eray O, Isik S, Sayrac AV, Yigit OE, Rinnert S. The value of ETCO2 measurement for COPD patients in the emergency department. Eur J Emerg Med. 2011;18:9-12. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 12] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 7. | Walker CM, Rosado-de-Christenson ML, Martínez-Jiménez S, Kunin JR, Wible BC. Bronchial arteries: anatomy, function, hypertrophy, and anomalies. Radiographics. 2015;35:32-49. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 106] [Cited by in RCA: 124] [Article Influence: 12.4] [Reference Citation Analysis (0)] |
| 8. | Rojas S, Quintana E, Ortega M, Rodríguez-Baeza A. A case of unusual configuration of the right bronchial arteries combined with cryptogenic severe bilateral hypertrophy. Surg Radiol Anat. 2017;39:1049-1052. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |