Published online Feb 26, 2023. doi: 10.12998/wjcc.v11.i6.1299
Peer-review started: October 21, 2022
First decision: December 13, 2022
Revised: January 3, 2023
Accepted: February 8, 2023
Article in press: February 8, 2023
Published online: February 26, 2023
Processing time: 126 Days and 5.9 Hours
Mandibular retraction is the main etiological mechanism of class II malocclusion in China and the subsequent distal molar relationship can cause functional discomfort in mastication, breathing and the temporomandibular joint. The use of mandibular advancement (MA) devices has recently emerged as an adolescent mandibular retraction treatment; however, current studies regarding the effect thereof are relatively few, and there is lack of sufficient clinical support.
To investigate the clinical effect of invisalign MA on the treatment of mandibular retraction in adolescents.
This study included 30 adolescent patients who underwent treatment with the MA appliances from December 2017 to June 2021. The lateral cephalometric data before and after treatment were collected and imported into Dolphin Imaging software. The changes were measured by linear measurement superimposed with lateral cephalometric trajectory based on the Pancherz technology.
There was no significant difference in the length and position of maxilla before and after the treatment. The position of the mandible moved 3.13 mm, the length increased 4.14 mm, the mandibular ramus length increased 4.09 mm, the body length increased 4.25 mm, and the position of the condyle moved 1.03 mm forward after treatment. Additionally, changes in the incisor sagittal position and labial inclination were observed. The position of the upper incisor point moved back 1.33 mm, without statistical difference, the inclination and tooth angle decreased by 3.44° and 4.06°, respectively; the position of the lower incisor point was moved 2.98 mm, and the inclination and tooth angle increased by 2.62° and 1.23°, respectively. Furthermore, changes in the incisor overjet and molar relationship were seen. Overjet decreased by 4.31 mm, of which 1.78 mm was due to dental factors, accounting for 41.3% of the effect as opposed to 58.7% due to skeletal factors. Molar relationship improved 3.87 mm, with 1.34 mm due to dental factors, and dental and skeletal factors were accounted for 34.6% and 65.4% of the effect, respectively.
For adolescent patients with mandible retraction, invisalign MA can effectively promote the mandible growth, and it was proven to be mainly due to skeletal effects.
Core Tip: This study aimed to investigate the clinical effect of invisalign mandibular advancement (MA) in the treatment of mandibular retraction in adolescents. In addition to the conventional cephalometric analysis method, Pancherz analysis was used to separate the skeletal and dental effects. The results of this study show that invisalign MA can effectively promote the adolescent mandible growth, improve the incisor overjet and molar relationship, and it was proven to be mainly due to skeletal effects.
- Citation: Kong L, Liu XQ. Efficacy of invisible advancement correction for mandibular retraction in adolescents based on Pancherz analysis. World J Clin Cases 2023; 11(6): 1299-1309
- URL: https://www.wjgnet.com/2307-8960/full/v11/i6/1299.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i6.1299
Skeletal II malocclusion is a common deformity in clinical orthodontics, usually manifesting clinically as maxillary protrusion, mandibular retraction, and deep overjet. The subsequent distal molar relationship can cause functional discomfort in mastication, breathing, and the temporomandibular joint[1]. Studies have shown that mandibular retraction is the main etiological mechanism of class II malocclusion in China[2,3]. Therefore, early intervention should be carried out for these patients, and facial shape and function should be improved through functional orthodontics to guide the mandible forward[2]. The best time for this intervention is at the peak of youth growth and development[4].
Commonly used functional appliances include Twin-Block, Activator, and Herbst. Although these have been proven to be effective, they all have various problems, such as large volumes, heavy foreign body sensation, and a long course for the second fixed treatment for fine adjustment[5,7]. In 2016, a mandibular advancement (MA) device (Figure 1) was developed to combine the concept of growth regulation with tooth movement to support simultaneous dental arch expansion, tooth alignment, and mandibular advancement[3,8,9]. MA has recently emerged as an adolescent mandibular retraction treatment[5,10]; however, current studies regarding the effect thereof are relatively few, and there is lack of sufficient clinical support. We aimed to accurately measure and analyse the differences of skeletal and dental changes before and after MA appliance treatment using Dolphin Imaging software 3D fixed point and Pancherz overlap analysis[8,11]. These were combined with traditional methods to evaluate clinical efficacy in the treatment of skeletal class II mandibular retrogression patients.
From December 2017 to June 2021, adolescents with skeletal II mandibular retraction treated with an MA appliance in the Department of Orthodontics, the Affiliated Hospital of Qingdao University were analysed. Thirty patients were screened according to the inclusion and exclusion criteria as study samples. This study was reviewed and approved by the Medical Ethics Committee of the Affiliated Hospital of Qingdao University (authorisation number: QYFYWZLL26729). Initially, an information letter and informed consent forms were sent to caregivers of all participants. They were asked to carefully read the study objectives and procedures, fill out their contact information, and sign the consent form if they agreed to participate. Adolescents whose parents did not agree to participate were excluded from the study.
We included participants who[4,12-14]: Were at early peak of youth growth and development or peak of youth growth and development [cervical vertebral maturation stage (CVMS) between CVMS1 and CVMS3]; with convex type, retraction of the mandible, the angle between SN and NB (SNB) ≤ 78°, maxillary normal or mild protrusion, the angle between SN and NA (SNA) = 80° ± 2°; stable late mixed dentition or early permanent dentition; mixed dentition the angle between NA and NB (ANB) ≥ 6°, permanent dentition ANB ≥ 5°; and horizontal growth or average growth, SN/MP ≤ 37°. We excluded those with combined severe facial deviation; substantial disease of the temporomandibular joint; previous history of trauma and cleft lip and palate surgery; and previous orthodontic treatment history.
The treatment process of invisalign MA generally consists of three stages: Pre-MA; MA; and post-MA. In the pre-MA stage, the curve of spee is mainly level, the positional relationship between the upper and lower dental arches is adjusted using the expansion arch, the anterior teeth are aligned or adducted with the space, the posterior teeth are repositioned, and the reverse is removed. During the MA phase, there is coordinated further levelling of the dentition, leading to skeletal advancement to correct the class II molar relationship. This stage requires at least 26 steps, often increasing by 2 mm every seven days and eight steps (approximately two months). The final stage may be more than eight steps to achieve balance and stability and can be combined with class II traction when necessary. After reaching the target site and stabilization, an oral scan was performed, followed by post-MA to complete fine adjustment. Stage T0 and stage T1 radiographs were taken at the beginning and end of the treatment, respectively. For image data acquisition, lateral cranial radiographs taken at T0 and T1 stages on 30 patients meeting the inclusion criteria were collected for comparative analysis.
The lateral radiographs were imported into Dolphin Imaging software for data measurement, mainly using Pancherz analysis, combined with conventional measurement methods such as Down analysis and Wits analysis. Sagittal changes were studied using linear measurements superimposed on lateral cranial radiographs based on the Pancherz method.
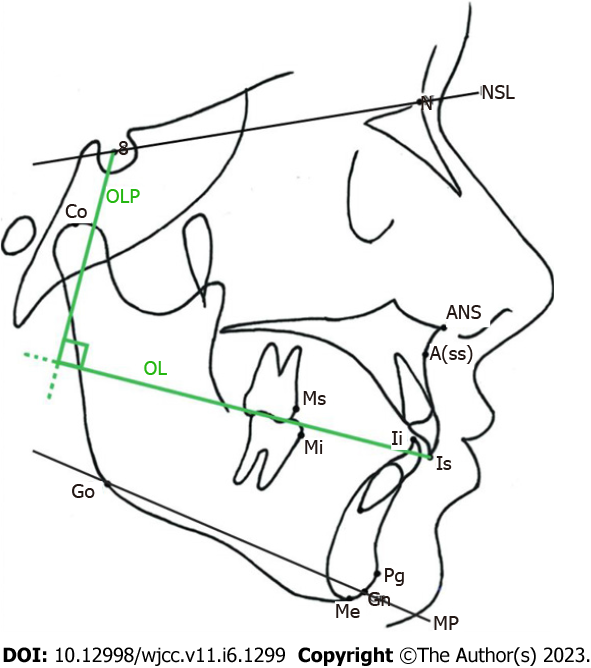
We established the Pancherz analysis method as follows: The occlusal plane (OL) was made on the lateral cephalic radiograph before treatment (through the convex incisal edge point in the upper incisor and distal buccal cusps in the maxillary first molar) as the horizontal reference axis. We used the sella point (S) to OL vertical plane (OLP) as the vertical reference axis and formed a line between the OL and OLP coordinates. S was used as the overlap point, the SN plane, the line connecting the S point and N point line (Figure 2) was overlapped, and its coordinates were transferred to the lateral cranial radiographs after treatment. The post-treatment data were measured. All linear measurements were made on lines parallel to OLP. A total of 22 measurement markers and reference planes, as well as 28 skeletal and dental measurements, were selected to measure and analyse the lateral radiographs of patients before and after treatment (Figure 2 and Table 1).
| Measurement | Definition |
| ss/OLP (mm) | Maxillary position, vertical distance from ss point to OLP |
| Pg/OLP (mm) | Mandibular position, vertical distance from Pg point to OLP |
| Co/OLP (mm) | Condyle position, vertical distance from Co point to OLP |
| Pg/OLP + Co/OLP (mm) | Mandibular length |
| Co-Go (mm) | Length of mandibular ascending ramus |
| Go-Pg (mm) | Length of mandibular body |
| Co-Pg (mm) | The total length of the mandible |
| SNA (°) | Sagittal relationship of anterior maxilla to basal bone |
| SNB | Sagittal relationship of anterior mandibular to basal bone |
| ANB | Sagittal position relationship between upper and lower basal bone |
| Wits | The distance between upper and lower alveolar points and occlusal plane |
| SN-MP | The plane angle of the mandible, the plane tangent to the lower edge of the mandible through the point Me |
| S-Go/N-Me | Posterior height/anterior height |
| ANS-Me/N-Me | Anterior inferior height/anterior height |
| is/OLP | Position of upper central incisor |
| ii/OLP | Position of lower central incisor |
| ms/OLP | Position of maxillary first molar |
| mi/OLP | Position of the lower first molar |
| U1-NA | Inclination of maxillary central incisor |
| U1-SN | Upper central incisor angle |
| L1-NB | Inclination of lower central incisor |
| L1-MP | Lower central incisor angle |
| is/OLP-ii/OLP | The distance from is point to OLP minus the distance from ii point to OLP is used to represent overjet |
| ms/OLP-mi/OLP | The distance from ms point to OLP minus the distance from mi point to OLP is used to describe molars |
| is/OLP-ss/OLP | Changes in the position of the upper central incisor relative to the maxilla |
| ii/OLP-pg/OLP | Changes in the position of the lower central incisor relative to the mandible |
| ms/OLP-ss/OLP | The position change of maxillary first permanent molars relative to maxilla |
| mi/OLP-pg/OLP | Change in the position of the first permanent molars relative to the mandible |
The same researcher conducted three measurements on the patient’s cranial lateral radiographs, on the same computer, at an interval of more than two weeks before and after treatment; the average of the three measurements was taken as the final research data. Paired samples t test was used to study the changes before and after treatment for all variables within the same group. All data were analysed using the by SPSS 23.0 software, and the significance level was set as P < 0.05[15].
In this experiment, Pg/OLP was used as the main analysis index, and the hypothesis test of the population mean of the two groups was used. According to the results of published literature, α = 0.05 (bilateral test), degree of assurance 1 - β = 0.8 were selected, and the sample sizes of the experimental group and the control group were equal. The following formula was used (Figure 3). A sample size of 25 patients in each group was calculated using Pg/OLP, 25 patients in each group. Considering that the shedding rate was 10%, 28 cases were required for the experimental and control groups to ensure the scientific design of the study. Considering the actual number of patients who had completed clinical work and met the inclusion criteria, 30 patients were finally selected, including 15 males and 15 females. The ages of participants ranged from 10 to 13 years, with an average of 11.6 ± 0.9 years.
ss/OLP value representing maxillary length did not change significantly (P > 0.05). The Pg/OLP of the mandible and Co-OLP of the condyle increased by 3.13 mm and 1.03 mm, respectively (P < 0.05), indicating that the mandible moved forward and down after MA treatment. The average increase of Pg/OLP + Co/OLP in mandibular length was 4.14 mm, the average increase of Co-Go in mandibular ramus length was 4.09 mm, and the average increase of Go-Pg in mandibular body length was 4.25 mm. The differences were statistically significant (P < 0.05).
SNA decreased slightly after MA appliance treatment, but the difference was not statistically significant (P > 0.05), indicating that the sagittal direction of the maxilla was not significantly restricted. After treatment, the mean value of SNB increased by 1.96°, ANB decreased by 2.03°, and Wits decreased by 2.90 mm, which were statistically significant compared with T0 (P < 0.05), indicating that the sagittal relationship of the mandible was significantly improved.
The SN-MP of the mandibular plane angle increased by 1.65° on average before treatment, and the difference was statistically significant (P < 0.05). The ratio of S-Go/N-Me between posterior height and anterior height decreased by 2.04% on average (P < 0.05). The ratio of anterior-inferior height to anterior-inferior height (ANS-Me/N-Me) increased by 1.45% on average (P < 0.05). The results showed that the sub facial 1/3 height of patients increased significantly after MA appliance treatment (Table 2).
| Measurement | Pre-treatment T0 | Post treatment T1 | Difference T1-T0 | T value | P value |
| ss/OLP (mm) | 71.42 ± 3.76 | 72.02 ± 4.05 | 0.60 ± 0.82 | -0.532 | 0.258 |
| Pg/OLP (mm) | 72.55 ± 3.25 | 75.68 ± 4.53 | 3.13 ± 0.89 | -1.561 | 0.029a |
| Co-OLP (mm) | -8.57 ± 0.65 | -9.60 ± 0.45 | -1.03 ± 0.79 | -1.349 | 0.000c |
| Pg/OLP + Co/OLP (mm) | 82.01 ± 1.57 | 86.25 ± 2.05 | 4.14 ± 2.18 | -1.687 | 0.000c |
| Co-Go (mm) | 50.03 ± 4.15 | 54.12 ± 3.65 | 4.09 ± 1.58 | -3.037 | 0.018a |
| Go-Pg (mm) | 76.18 ± 5.43 | 80.43 ± 3.90 | 4.25 ± 2.87 | -4.581 | 0.001b |
| Co-Pg (mm) | 108.58 ± 7.08 | 113.60 ± 6.58 | 5.02 ± 1.83 | -3.803 | 0.038a |
| SNA (°) | 80.95 ± 1.90 | 80.67 ± 1.54 | -0.28 ± 0.04 | 1.915 | 0.166 |
| SNB (°) | 74.89 ± 1.78 | 76.85 ± 1.65 | 1.96 ± 2.56 | 3.218 | 0.000c |
| ANB (°) | 6.11 ± 1.06 | 4.08 ± 1.34 | -2.03 ± 1.32 | 18.370 | 0.000c |
| Wits (mm) | 6.41 ± 2.45 | 3.51 ± 1.18 | -2.90 ± 1.72 | 7.138 | 0.000c |
| SN-MP (°) | 31.20 ± 3.62 | 32.85 ± 3.51 | 1.65 ± 1.37 | -1.478 | 0.043a |
| S-Go/N-Me | 64.12 ± 2.68 | 62.08 ± 3.09 | -2.04 ± 1.68 | 1.386 | 0.035a |
| ANS-Me/N-Me | 54.40 ± 1.89 | 55.85 ± 2.18 | 1.45 ± 1.37 | -2.087 | 0.045a |
| is/OLP | 77.98 ± 6.07 | 76.65 ± 5.71 | -1.33 ± 3.08 | 1.657 | 0.353 |
| ii/OLP | 71.11 ± 5.04 | 74.09 ± 4.76 | 2.98 ± 1.08 | -1.709 | 0.071 |
| ms/OLP | 46.86 ± 5.34 | 45.67 ± 4.87 | -1.19 ± 0.39 | 1.687 | 0.205 |
| mi/OLP | 45.30 ± 3.28 | 47.80 ± 5.18 | 2.50 ± 1.04 | -1.560 | 0.082 |
| U1-NA | 28.89 ± 7.51 | 25.45 ± 5.40 | -3.44 ± 6.89 | -7.760 | 0.010a |
| U1-SN | 108.04 ± 3.01 | 103.98 ± 4.78 | -4.06 ± 4.88 | 4.673 | 0.000c |
| L1-MP | 95.20 ± 2.93 | 96.43 ± 2.86 | 1.23 ± 0.40 | -0.318 | 0.000c |
| L1-NB | 22.78 ± 4.08 | 25.40 ± 3.32 | 2.62 ± 1.63 | -3.341 | 0.030a |
| is/OLP-ii/OLP | 6.87 ± 1.51 | 2.56 ± 0.76 | -4.31 ± 1.43 | 16.30 | 0.000c |
| ms/OLP-mi/OLP | 2.13 ± 1.20 | -1.74 ± 1.31 | -3.87 ± 0.78 | 10.61 | 0.000c |
| is/OLP-ss/OLP | 7.04 ± 1.07 | 6.48 ± 2.09 | -0.61 ± 1.71 | 4.25 | 0.089 |
| ii/OLP-pg/OLP | -1.12 ± 1.65 | 0.05 ± 1.70 | 1.17 ± 0.83 | 1.75 | 0.005b |
| ms/OLP-ss/OLP | -23.18 ± 2.69 | -24.34 ± 1.98 | -1.16 ± 1.78 | -15.68 | 0.000c |
| mi/OLP-pg/OLP | -26.98 ± 2.45 | -26.80 ± 2.78 | 0.18 ± 1.57 | 3.05 | 0.185 |
After treatment, the position of upper central incisor point is/OLP decreased by 1.33 mm on average, indicating that the incisor end of upper central incisor moved to the palate by 1.33 mm, while the inclination of upper central incisor U1-NA decreased by 3.44° on average (P < 0.05), and the angle of upper central incisor U1-SN decreased by 4.06° (P < 0.05). The results showed that the upper anterior teeth were adducted after treatment.
After treatment, the position of the lower central incisor point ii/OLP increased 2.98 mm on average, indicating that the incisal of the lower central incisor moved 2.98 mm to the labial, while the inclination of the lower central incisor increased 2.62° on average (P < 0.05), and the angle of the lower central incisor increased 1.23° (P < 0.05). Compared with T0, there was a certain degree of labial inclination in the lower anterior teeth at T1 stage (Table 2).
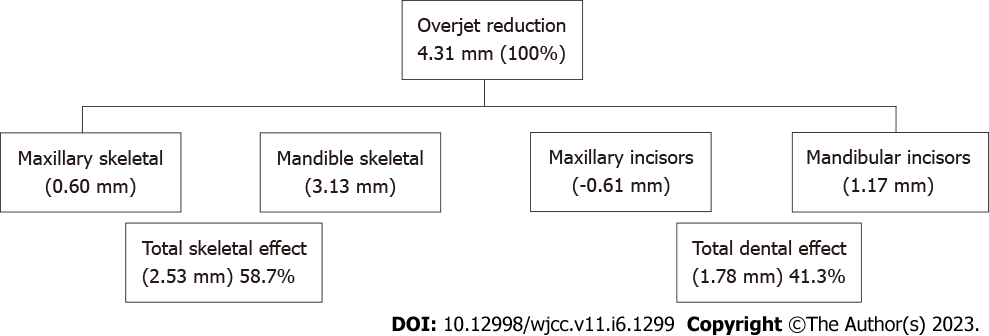
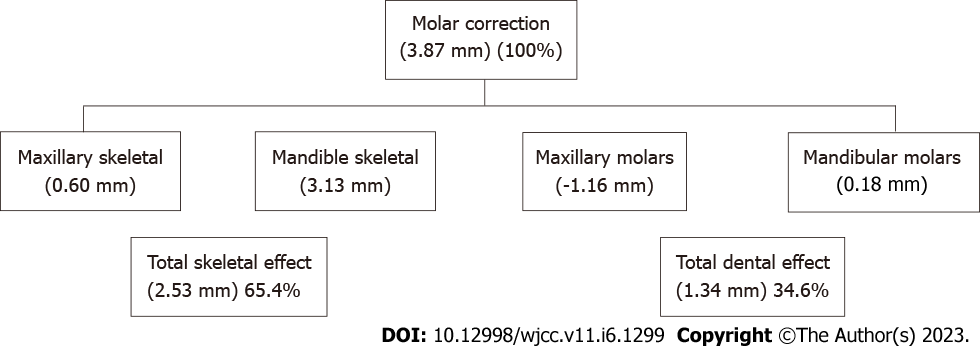
Compared with the T0 period before treatment, the anterior tooth overjet is/OLP-ii/OLP decreased by 4.31 mm (P < 0.05) and molar relationship ms/OLP-mi/OLP increased by 3.87 mm. The difference was statistically significant (P < 0.05), and the upper central incisors moved 0.61 mm compared with the maxillary to lingual side. The difference was not statistically significant (P > 0.05).
The lower central incisor migrated 1.17 mm significantly (P < 0.05) compared with the mandible lip side. The maxillary first molars migrated 1.16 mm significantly (P < 0.05) compared with the mandible to the bistal surface. The mandible first molars moved 0.18 mm compared with the mandible, but this difference was not significant (P > 0.05) (Table 2).
After treatment, dental and skeletal overjet changed by an average of 4.31 mm. The total change was due to an upper incisor adduction improvement of 0.61 mm and lower incisor labial inclination improvement of 1.17 mm. Tooth factors were responsible for a total of 1.78 mm, with the remainder due to skeletal factors. Regarding the calculation of cause of overjet change, skeletal factors accounted for 58.7%, and dental factors accounted for 41.3%. The total change of molar relationship was improved by 3.87 mm on average, of which 1.16 mm was contributed to by maxillary molar distal displacement. A total of 0.18 mm was increased by mandibular molar mesial displacement, dental factors totalled 1.34 mm, and skeletal and dental factors accounted for 65.4% and 34.6%, respectively (Figures 4 and 5).
In the treatment of adolescent patients with skeletal retraction of the mandible, invisalign MA can effectively promote the growth and development of the mandible and improve the appearance of the mandible. The treatment effect has both dental effect and skeletal effects, and the skeletal effect is of primary importance.
Pancherz analysis was mainly used[8,16]. Firstly, the OL line, OL, on the lateral cranial radiographs before treatment was taken as the X-axis, and a vertical line, OLP passing point S, was made as the Y-axis to establish the rectangular coordinate system. The main reason for choosing the coordinate plane is that it has little change before and after treatment; therefore, the coordinate system is relatively stable; the reference line coincidence is good before and after treatment; and the measurement data is easy to compare. During treatment, it is necessary to select a stationary point, S, as the coincidence point; then select a steady SN plane before growth peak to overlap the datum plane. Coordinates should be moved per slice to the head before and after the treatment side, and a unified coordinate system calculating and analysing the measurements in all types of linear results can use a linear OLP record. The skeletal and dental change, and change in correlation between them, should be analysed so that before and after treatment sagittal direction changes reflect directly on the overlap line spacing. This vividly and accurately expresses the before and after treatment in patients, and we can adopt the formula calculation to determine the proportion of bone and teeth changes, to determine a treatment, the changes of bone and the separation of teeth before and after treatment clearly reflect the curative effect. However, Pancherz analysis is limited in that it usually only focuses on the changes of the mandible and alveola in the sagittal direction, but not the vertical and plane rotation. In addition, the Pancherz analysis method does not involve the change of labial-lingual inclinations and other angles of the incisor, because it uses line distance measurement. Therefore, we combined traditional X-ray cephalometric analysis methods, such as Downs and Wits analysis, to comprehensively analyse the effect of the MA appliance before treatment.
Whether functional appliances can actually inhibit the growth and development of the maxilla has long been debated[7,17,18]. One theory is that functional orthotics inhibit the growth and development of the maxilla by generally making the maxilla grow backward and downward and rotate, while reducing the ability to grow. The other view is that the functional appliance has no effect on the position and growth direction of the maxilla but causes upper alveolar remodelling with the distal movement of the maxillary dentition. Some researchers believe that the functional appliance needs to be combined with traction of an external force to the mouth to form effective maxillary development. In this study, the distance from ss to the OLP plane increased by 0.60 mm on average after MA treatment, indicating an increase in sagittal basal bone length of the maxilla that would be predictable in growing adolescents. The results show that the MA appliance had no significant inhibition on the growth and development of the maxilla.
The key to the function of the advancement appliance is to initiate the response mechanism of adaptive remodelling of the mandibular condyle by guiding the retraction of the mandible forward, so as to maintain the stable position of the mandible and rebuild its relationship with the maxilla. In the study, Pg-OLP distance increased after treatment. Furthermore, Go-Pog of mandibular body length, Pg/OLP + Co/OLP of full mandibular body, Co-OLP of mandibular ramus, and SNB angle all increased, with statistical significance, confirming that the growth and development of the mandible was significantly improved after treatment, and the sagittal relationship between the mandible and maxilla was improved and coordinated. In the leading process, the previously restricted growth space of the mandible is released, which stimulates the downward reconstruction of the growth cent of the condyle and increases the height of the mandibular ascending ramus[19]. After treatment, the effect of mandibular growth is mainly considered to be the sagittal forward movement of the jaw promoted by the function of the appliance, and the growth of the mandible is considered to be due to normal growth and development[20].
In this study, after MA treatment, the ascending ramus height, the ratio of anterior-inferior height to posterior-inferior height, and the mandibular plane angle all increased, while the ratio of posterior-anterior height to anterior-inferior height decreased. The results showed that the lower 1/3 height and mandibular plane angle increased after the use of the invisible appliance to guide the mandible forward, and the mandible may have a certain degree of backward and downward rotation.
The removed mandibular natural growth trend may be due to the process of leading, when the mandible moves forward, the upper and lower teeth form a wedge space at the back and the molars elongate to compensate which causes compensatory mandibular growth and, thus, mandibular clockwise rotation. In addition, the mandible is forced to be in a new jaw position during the extension process, which releases the growth space of the mandible, promotes downward reconstruction of the growth centre of the condyle, and causes elevation of the mandibular ramus to accelerate[19]. As all the cases included in this study were horizontal and average growth types of mandibular retraction, the lower 1/3 height of the patient’s face was effectively improved through treatment and the lateral appearance was more beautiful.
Studies have confirmed that the MA appliance can effectively improve the overjet and molar relationship of class II patients. After treatment, the overjet of most patients was significantly improved, and the improvement of the upper and lower first molars was mostly neutral or a mild mesial relationship. The reduction of overjet and the improvement of molar relationship are the results of the changes of bone and teeth in the treatment of class II mandibular retraction. The curative effect is composed of dental and skeletal effects. According to the calculation, the overjet of the front teeth after correction was reduced by 4.31 mm, and the molar relationship was improved by 3.87 mm. Among them, skeletal factors accounted for 58.7% and 65.4% of the total proportion of overjet and molar relationship, respectively. Dental factors accounted for 41.3% and 34.6%, respectively. It is concluded that the MA appliance can be used in the treatment of skeletal II mandibular retraction, and the improvement of the relationship between overjet and molar is more influenced by the skeletal effect.
For adolescent patients with skeletal retraction of the mandible, the correction with invisalign MA can effectively promote growth, development, and improved appears of the mandible. There were both dental and skeletal effects, but the skeletal effect was of primary importance as it may play a role in the reconstruction of the temporomandibular joint.
The clinical retrospective study is summarized and designed on the basis of the existing case data. The integrity of case data are not controlled by the experimental design, and confounding factors and bias are inevitable. Therefore, only sophisticated statistical methods can be used to avoid or minimize the effects. Due to the insufficient sample size of the control group, this study adopted a method of self before and after control.
In the treatment of adolescent patients with skeletal retraction of the mandible, invisalign MA can effectively promote the growth, development, and appearance of the mandible. The treatment effect has both dental and skeletal effects, with skeletal effects having a stronger influence.
In recent years, invisalign treatment with mandibular advancement (MA) has emerged for correcting class II malocclusion in growing teens with patients reporting comfort and satisfaction during the treatment; this approach uses precision wings incorporated into the upper and lower aligners to engage the mandible in an advanced edge-to-edge position while the anterior teeth are being aligned. It was developed to combine the concept of growth regulation with tooth movement to support simultaneous dental arch expansion, tooth alignment and MA. Whether the simultaneous correction of the bite along with dental alignment results in greater efficiency compared to treating the bite relationship and the dental alignment sequentially, there is lack of sufficient clinical research support.
This study aimed to investigate the clinical effect of invisalign MA in the treatment of mandibular retraction in adolescents. Pancherz analysis was used to separate the skeletal and dental effects.
To analyse the dentoskeletal effects of the invisalign MA device in the treatment of skeletal class II malocclusions.
Lateral cranial radiographs before and after treatment of 30 subjects were collected, pre-treatment (T0) and post-treatment (T1) lateral cephalograms were mainly traced using Pancherz’s cephalometric analysis, the differences were assessed with paired samples t-test at the P < 0.05 level.
Improvement in class II relationship resulted from skeletal and dental changes. The position of the mandible moved forward 3.13 mm. There was 4.31 mm overjet reduction of which 58.7% due to skeletal factors, and 3.87 mm molar correction of which skeletal factors were accounted for 65.4%.
The research show the effectiveness of MA in the management of skeletal class II malocclusions due to mandibular retrusion, highlighting an improvement in the sagittal relationships between the upper and lower bases.
Further prospective studies should be conducted with a control group and larger sample size.
I would like to thank my supervisor Xin-Qiang Liu for his guidance through each stage of the process.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Arumugam EAP, India; Rakhshan V, Iran S-Editor: Wang JJ L-Editor: Wang TQ P-Editor: Wang JJ
| 1. | Rédua RB. Different approaches to the treatment of skeletal Class II malocclusion during growth: Bionator versus extraoral appliance. Dental Press J Orthod. 2020;25:69-85. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 7] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 2. | Ajami S, Morovvat A, Khademi B, Jafarpour D, Babanouri N. Dentoskeletal effects of class II malocclusion treatment with the modified Twin Block appliance. J Clin Exp Dent. 2019;11:e1093-e1098. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 3. | Caruso S, Nota A, Caruso S, Severino M, Gatto R, Meuli S, Mattei A, Tecco S. Mandibular advancement with clear aligners in the treatment of skeletal Class II. A retrospective controlled study. Eur J Paediatr Dent. 2021;22:26-30. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 8] [Reference Citation Analysis (0)] |
| 4. | Koçak T, Akan B. Assessment of maturation indicators in individuals with different skeletal malocclusion. J Orofac Orthop. 2021;82:187-197. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 6] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 5. | Azaripour A, Weusmann J, Mahmoodi B, Peppas D, Gerhold-Ay A, Van Noorden CJ, Willershausen B. Braces versus Invisalign®: gingival parameters and patients' satisfaction during treatment: a cross-sectional study. BMC Oral Health. 2015;15:69. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 76] [Cited by in RCA: 119] [Article Influence: 11.9] [Reference Citation Analysis (0)] |
| 6. | Tamer İ, Öztaş E, Marşan G. Orthodontic Treatment with Clear Aligners and The Scientific Reality Behind Their Marketing: A Literature Review. Turk J Orthod. 2019;32:241-246. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 66] [Article Influence: 11.0] [Reference Citation Analysis (0)] |
| 7. | Tripathi T, Singh N, Rai P, Gupta P. Comparison of Dentoskeletal Changes, Esthetic, and Functional Efficacy of Conventional and Novel Esthetic Twin Block Appliances among Class II Growing Patients: A Pilot Study. Turk J Orthod. 2020;33:77-84. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 8. | Ardeshna A, Bogdan F, Jiang S. Class II correction in orthodontic patients utilizing the Mandibular Anterior Repositioning Appliance (MARA). Angle Orthod. 2019;89:404-410. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 10] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 9. | Antonarakis GS, Kiliaridis S. Short-term anteroposterior treatment effects of functional appliances and extraoral traction on class II malocclusion. A meta-analysis. Angle Orthod. 2007;77:907-914. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 52] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 10. | Rossini G, Parrini S, Castroflorio T, Deregibus A, Debernardi CL. Efficacy of clear aligners in controlling orthodontic tooth movement: a systematic review. Angle Orthod. 2015;85:881-889. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 236] [Cited by in RCA: 415] [Article Influence: 37.7] [Reference Citation Analysis (0)] |
| 11. | Pancherz H. A cephalometric analysis of skeletal and dental changes contributing to Class II correction in activator treatment. Am J Orthod. 1984;85:125-134. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 107] [Cited by in RCA: 98] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 12. | Candir M, Kerosuo H. Mode of correction is related to treatment timing in Class II patients treated with the mandibular advancement locking unit (MALU) appliance. Angle Orthod. 2017;87:363-370. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 13. | Ravera S, Castroflorio T, Galati F, Cugliari G, Garino F, Deregibus A, Quinzi V. Short term dentoskeletal effects of mandibular advancement clear aligners in Class II growing patients. A prospective controlled study according to STROBE Guidelines. Eur J Paediatr Dent. 2021;22:119-124. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 14. | Baccaglione G, Rota E, Ferrari M, Maddalone M. Second Class Functional Treatment: Andreasen Activator vs Twin Block. Int J Clin Pediatr Dent. 2020;13:144-149. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 15. | Elfeky HY, Fayed MS, Alhammadi MS, Soliman SAZ, El Boghdadi DM. Three-dimensional skeletal, dentoalveolar and temporomandibular joint changes produced by Twin Block functional appliance. J Orofac Orthop. 2018;79:245-258. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 36] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 16. | Singaraju GS, Vannala V, Ankisetti SA, Mandava P, Ganugapanta VR, Unnam D. Evaluation of Sagittal Changes in Class II Div 2 Patients with Decelerating Phase of Growth by PowerScope Appliance: A Retrospective Cephalometric Investigation. J Pharm Bioallied Sci. 2019;11:S208-S215. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Reference Citation Analysis (0)] |
| 17. | Brito DBA, Henriques JFC, Fiedler CF, Janson G. Effects of Class II division 1 malocclusion treatment with three types of fixed functional appliances. Dental Press J Orthod. 2019;24:30-39. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 18. | Alhammadi MS, Elfeky HY, Fayed MS, Ishaq RAR, Halboub E, Al-Mashraqi AA. Three-dimensional skeletal and pharyngeal airway changes following therapy with functional appliances in growing skeletal Class II malocclusion patients : A controlled clinical trial. J Orofac Orthop. 2019;80:254-265. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 12] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 19. | Souki BQ, Vilefort PLC, Oliveira DD, Andrade I Jr, Ruellas AC, Yatabe MS, Nguyen T, Franchi L, McNamara JA Jr, Cevidanes LHS. Three-dimensional skeletal mandibular changes associated with Herbst appliance treatment. Orthod Craniofac Res. 2017;20:111-118. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 27] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 20. | Perinetti G, Primožič J, Furlani G, Franchi L, Contardo L. Treatment effects of fixed functional appliances alone or in combination with multibracket appliances: A systematic review and meta-analysis. Angle Orthod. 2015;85:480-492. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 68] [Article Influence: 6.8] [Reference Citation Analysis (0)] |