Published online Feb 6, 2023. doi: 10.12998/wjcc.v11.i4.821
Peer-review started: October 27, 2022
First decision: November 30, 2022
Revised: December 12, 2022
Accepted: January 16, 2023
Article in press: January 16, 2023
Published online: February 6, 2023
Processing time: 101 Days and 12.7 Hours
The coronavirus disease 2019 (COVID-19) pandemic posed new challenges in patient care worldwide. Vaccinations, which have proven efficacious in lowering the COVID-19 hospital burden, are still avoided by large populations. We, ther
To evaluate whether patient vaccine hesitancy affected the hospital care team (HCT) perceptions.
We performed a prospective clinical study using structured questionnaires. We approached physicians and nurses with previous experience caring for COVID-19 patients from 11 medical centers across Israel during the fourth COVID-19 surge (September and October 2021). The participants completed a questionnaire with the following parts: (1) Sociodemographic characteristics; (2) Assessment of anger (STAXI instrument) and chronic workplace stress (Shirom-Melamed burnout measure); and (3) Three tools to assess the effect of patient vaccine hesitancy on the HCT perceptions (the difficult doctor-patient relation questionnaire, the medical staff perception of patient’s responsibility questionnaire and the characterological derogation questionnaire). Results were evaluated according to each part of the questionnaire and the questionnaire as a whole. Associations between HCT perceptions and their baseline characteristics, anger or chronic workplace stress were assessed.
The HCT experienced their relationship with unvaccinated patients as more difficult (P < 0.001, Cohen’s d = 0.85), perceived unvaccinated patients as responsible for their medical condition (P < 0.001, d = 1.39) and perceived vaccinated patients as having a higher character value (P < 0.001, d = 1.03). Unvaccinated patients were considered selfish (P < 0.001), less mature (P < 0.001) and less satisfying to care for (P < 0.001). The relationship with unvaccinated patients was more difficult among HCT with higher burnout (r = 0.37, n = 66, P = 0.002). No correlations with baseline characteristics were found. All three study tools showed high internal consistency (α between 0.72 and 0.845).
Our results should raise awareness of the possible effects of vaccine hesitancy on HCT perceptions regarding unvaccinated patients. In order to minimize the potential negative impact on patient care, designated departments should promote specific patient-centered preparations. Further investigations should assess whether vaccine hesitancy directly affects patient quality of care.
Core Tip: Coronavirus disease 2019 (COVID-19) vaccine hesitancy is common around the world. We considered that patient vaccine hesitancy could affect the hospital care team perceptions. To test that possibility, we implemented a questionnaire during the Delta variant surge among physicians and nurses with prior experience in caring for COVID-19 patients. We found that patient vaccine hesitancy negatively affected how the medical care team perceived these patients and their care. Vaccine hesitancy can negatively affect the physician-patient relationship and raising awareness of this important issue is crucial for proper interventions.
- Citation: Caspi I, Freund O, Pines O, Elkana O, Ablin JN, Bornstein G. Effect of patient COVID-19 vaccine hesitancy on hospital care team perceptions. World J Clin Cases 2023; 11(4): 821-829
- URL: https://www.wjgnet.com/2307-8960/full/v11/i4/821.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i4.821
Medical care team beliefs and practices are impacted by patient characteristics[1]. Such characteristics also have the potential to intervene with the shared decision-making process by changing physicians’ perceptions of their patients[2,3]. The coronavirus disease 2019 (COVID-19), which continues to affect millions of people globally since 2019, poses new challenges regarding patient care[4,5]. Severe COVID-19 infection has the potential for hospitalization due to possible complications that result in a high burden on the hospital care team (HCT)[6]. Caring for hospitalized COVID-19 patients requires functioning with full personal protective equipment and caring for patients who may rapidly deteriorate. This environment creates obvious stressful triggers.
The introduction of the mRNA COVID-19 vaccines was a crucial step in preventing the spread of the virus, limiting disease transmission and infectivity[7,8]. COVID-19 vaccines dramatically reduced the rate of hospitalizations due to severe disease as well as complications among hospitalized patients regardless of any comorbidities or age[9,10]. Despite its obvious benefits, several large populations avoided vaccination for various reasons, demonstrating distrust against the vaccines[11]. Therefore, it is not surprising that many studies focused on attitudes toward COVID-19 vaccines themselves and specifically on vaccine hesitancy for both patients and medical teams[11-13]. However, it is still unknown whether patient vaccine hesitancy influences the HCT’s perceptions of them. We hypothesized that HCTs would have negative perceptions towards the characteristics and care of vaccine-hesitant patients. Our aim was to evaluate this hypothesis and to raise awareness in order to promote early intervention, hopefully preventing potential negative effects on patient care.
This is a prospective clinical study conducted at 11 medical centers throughout Israel between September and October 2021 using standardized questionnaires. We held the study during the fourth surge of the COVID-19 pandemic when the Delta variant was predominant, and the hospital disease burden reached its peak. We approached physicians and nursing staff that treated COVID-19 patients to participate in the study. Invitations to participate in the study were offered personally or via social networks and whenever needed were followed by a text message with an active link to the questionnaire. Consenting participants were enrolled using an online interface. All participants accepted an informed consent form, agreed to participate by pressing “continue” within the questionnaire electronically and had the ability to drop out at any stage. Only participants who completed at least one of the three study tools (described below) were included in our final cohort. The study was approved by the ethics committee of The Academic College of Tel Aviv-Yaffo (Authorization number 2021142).
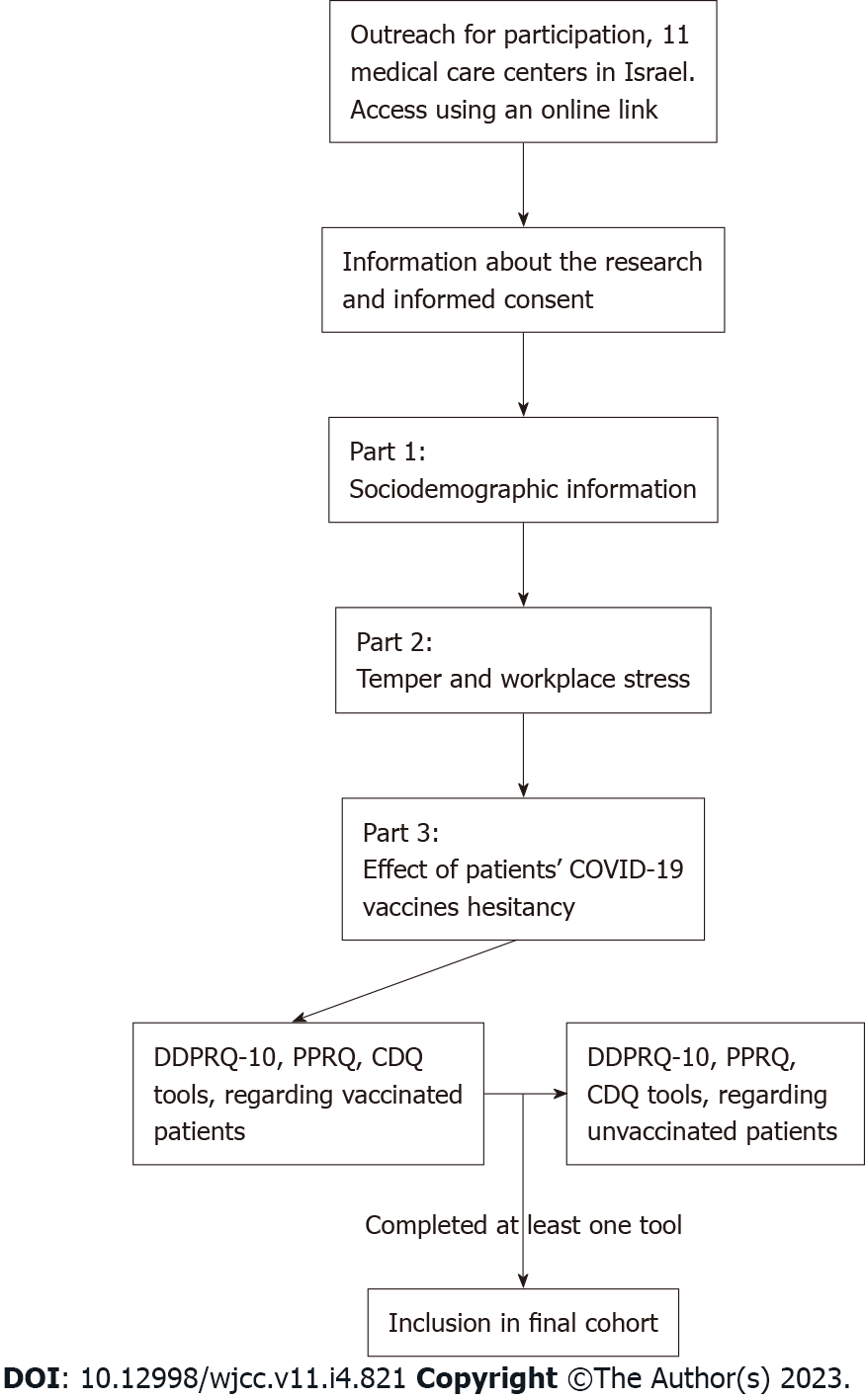
We created a computerized questionnaire via the Qualtrics platform. The design of our study instrument appears in Figure 1. The first set of questions discussed sociodemographic information, such as age, sex, profession (physician, nurse, etc.) and prior experience with treating COVID-19. The second part included questions about participant anger (4-point Likert scale, using the STAXI instrument[14]) and their chronic workplace stress (7-point Likert scale, using the Shirom-Melamed Burnout Measure[15]). The third part of the questionnaire assessed the effect of patient COVID-19 vaccine hesitancy on the participants. To properly assess this aspect, we used three validated tools that together created a comprehensive review of the topic. For comparison purposes, the third part (including the three tools) appeared twice, first regarding unvaccinated patients and second regarding vaccinated patients. The three selected tools used were as follows.
Tool 1-difficult doctor-patient relation questionnaire: A well-established questionnaire, consisting of 10 items answered on a 6-point Likert scale, with values ranging from 1 (“Not at all”) to 6 (“A great deal”)[16]. Higher scores indicate that the physician experiences the relationship with the patient as more difficult. In our study, we made a minor modification by using a 1 to 7 scale, to give participants an option of expressing a neutral (middle range) opinion, which is achieved by an uneven number of items.
Tool 2-medical staff perception of patient's responsibility questionnaire: This questionnaire was previously used in similar studies evaluating physician perception of illness, with a variety of patient populations[17,18]. It is written as a 10-item questionnaire, answered on a 7-point Likert scale, with values ranging from 1 (“Not at all”) to 7 (“A great deal”). A higher score indicates that the participant perceives the patient as more responsible for his own medical condition.
Tool 3-characterological derogation questionnaire: This questionnaire was written by Brouns[19], as part of a thesis regarding negative attitudes towards refugees and based on previous questionnaires by Correia et al[20]. It is a nine-item questionnaire, relating to the question: “In your opinion, what represents ‘X’ best?”. Five items include positive characteristics, e.g., polite, responsible, mature, warm and nice, and four items include negative characteristics e.g., stupid, selfish, untrue and unaware. The scoring was by a 7-point Likert scale, with values ranging from 1 (“Not at all”) to 7 (“A great deal”). A high score indicates that the participant perceives the patient’s character as a high-value character.
Categorical variables were described using frequencies and percentages. Continuous variables were described by mean and standard deviation. Comparison between answers regarding vaccinated and unvaccinated patients was utilized using paired samples t-test. P < 0.05 was defined as statistically significant. The effect size of significant results was calculated using Cohen’s d test. The internal consistency of each tool in the study instrument was measured using the alpha Cronbach score (alpha above 0.7 is considered high). Correlations were examined using the Pearson correlation coefficient. The analysis was performed using SPSS 26.0 for Windows.
During the study period, we approached more than 500 active physicians and nursing staff from 11 different medical centers. In total, 138 participants agreed to enroll in the study, and of them 66 (48%) completed at least one of the three study tools and were included in our cohort. Participant characteristics are presented in Table 1. In total, 38 (58%) participants were women, mean age was 40.5 ± 10, 37 (56%) were physicians (senior doctors, residents and interns), and 29 (44%) participants were staff of internal medicine departments. All but two were vaccinated (97%), and 12 (18%) had prior COVID-19.
| Variable | Study cohort |
| Age, mean ± SD | 40.5 ± 10.1 |
| Male sex | 28 (42) |
| Occupation | |
| Physicians | 37 (56) |
| Nursing staff | 22 (33) |
| Department managers/vice | 7 (11) |
| Medical field | |
| Internal or general medicine | 36 (54) |
| Psychiatry | 7 (11) |
| Intensive care unit | 4 (6) |
| Emergency department | 5 (8) |
| Other | 14 (21) |
| Vaccinated to COVID-19 | 64 (97) |
| Prior COVID-19 disease | 12 (18) |
| Anger, mean ± SDa | 1.8 ± 0.4 |
| Workplace stress, mean ± SDb | 3.1 ± 1 |
The three tools used for this study [difficult doctor-patient relation questionnaire (DDPRQ-10), medical staff perception of patient’s responsibility questionnaire (PPRQ) and characterological derogation questionnaire (CDQ)] showed a high internal consistency based on our results (α between 0.72 and 0.845). Table 2 presents the mean scores of selected questions from each tool comparing vaccinated and unvaccinated patients. Based on tool 1 (DDPRQ-10), the HCT considered caring for unvaccinated patients to be more frustrating (P < 0.001), time-consuming (P < 0.001) and less satisfying (P < 0.001). Answers in tool 2 (PPRQ) revealed that the HCT perceived unvaccinated patients to be responsible for their illness (P < 0.001), to consciously endanger their surroundings (P < 0.001) and as less deserving of occupying beds in the intensive care unit than vaccinated patients (P = 0.002). The HCT also believed that social and economic sanctions should be imposed on unvaccinated people (mean scores 4.2 and 4.1, respectively, P < 0.001 for both). Tool 3 (CDQ) indicated that unvaccinated patients were perceived as less mature, more selfish and more ignorant (P < 0.001).
| Questionsa | Unvaccinated, mean ± SD | Vaccinated, mean ± SD | P value |
| Tool 1-difficult doctor-patient relation questionnaire (7-point Likert scale)b | |||
| Do you expect to see clinical improvement in a COVID-19 patient? | 3.8 ± 1.6 | 5.5 ± 1.3 | < 0.001 |
| How frustrating is a patient with COVID-19? | 4.8 ± 2.0 | 3.2 ± 2.0 | < 0.001 |
| How frustrated are you with treating a COVID-19 patient? | 4.7 ± 2.0 | 2.8 ± 1.8 | < 0.001 |
| Are you satisfied when you care for COVID-19 patients? | 3.9 ± 2.0 | 4.6 ± 1.8 | 0.001 |
| How time consuming is caring for COVID-19 patients? | 5.0 ± 1.6 | 4.1 ± 1.5 | < 0.001 |
| How enthusiastic do you feel about caring for a COVID-19 patient? | 2.8 ± 1.8 | 3.2 ± 1.8 | 0.09 |
| How difficult is it to communicate with a COVID-19 patient? | 3.4 ± 1.8 | 2.4 ± 1.5 | < 0.001 |
| Tool 2-perception of patient’s responsibility questionnaire (7-point Likert scale)b | |||
| I believe a COVID-19 patient is responsible for his illness | 5.1 ± 1.8 | 2.1 ± 1.5 | < 0.001 |
| COVID-19 patients consciously endanger their family and environment | 5.4 ± 1.9 | 2.3 ± 1.7 | < 0.001 |
| COVID-19 patients have a bad influence on my personal life | 3.6 ± 2.2 | 1.6 ± 1.2 | < 0.001 |
| COVID-19 patients deserve to occupy beds in the ICU | 5.1 ± 1.9 | 5.9 ± 1.8 | 0.002 |
| I believe that social sanctions should be imposed on people un/vaccinated to COVID-19 | 4.2 ± 2.1 | 1.4 ± 1.1 | < 0.001 |
| I believe that economic sanctions should be imposed on people un/vaccinated to COVID-19 | 4.1 ± 2.2 | 1.4 ± 1.0 | < 0.001 |
| Un/vaccinated COVID-19 patients make it impossible to eradicate the pandemic | 5.0 ± 2.2 | 1.8 ± 1.2 | < 0.001 |
| Tool 3-characterological derogation questionnaire (7-point Likert scale)b | |||
| A patient with COVID-19 is polite | 3.4 ± 1.4 | 3.9 ± 1.3 | 0.001 |
| A patient with COVID-19 is responsible | 2.5 ± 1.6 | 5.2 ± 1.8 | < 0.001 |
| A patient with COVID-19 is mature | 2.7 ± 1.6 | 4.9 ± 1.7 | < 0.001 |
| A patient with COVID-19 is nice | 3.4 ± 1.4 | 3.9 ± 1.4 | 0.01 |
| A patient with COVID-19 is selfish | 4.6 ± 2.1 | 2.4 ± 1.7 | < 0.001 |
| A patient with COVID-19 is ignorant | 4.8 ± 1.9 | 2.6 ± 1.7 | < 0.001 |
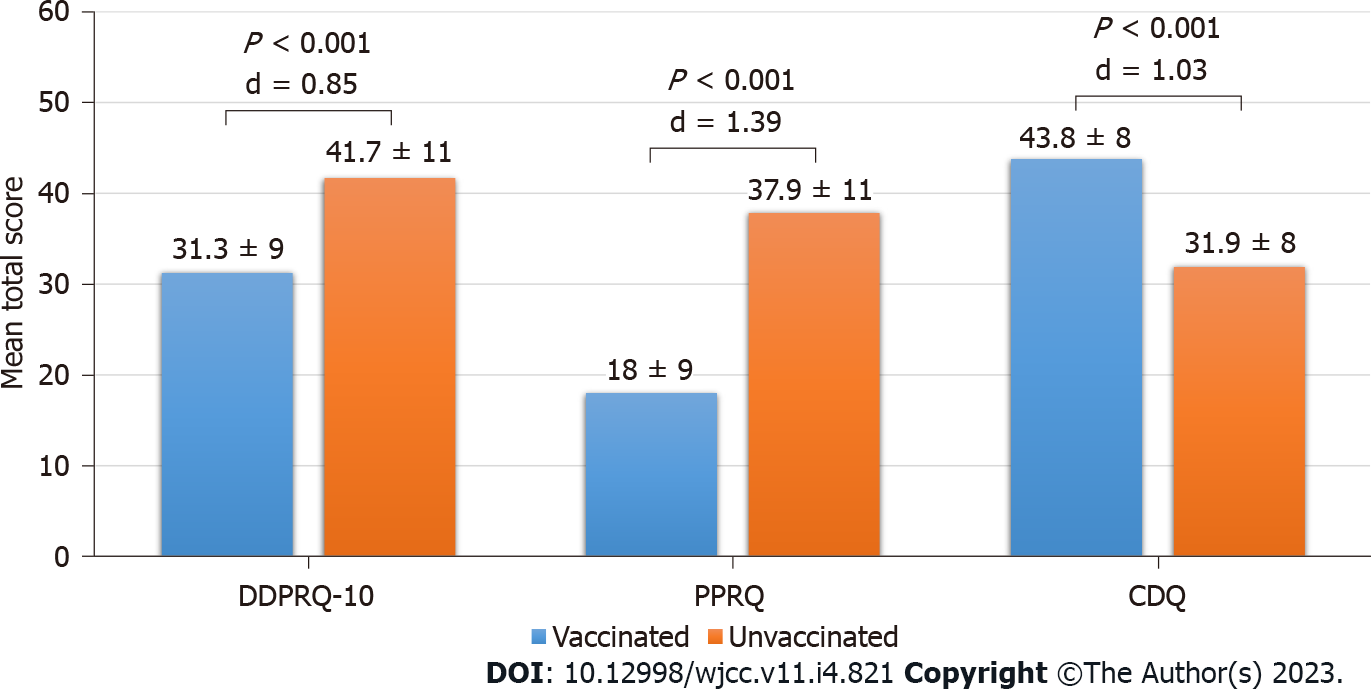
The mean total scores for each tool are presented in Figure 2. Based on these results, the HCT experienced their relationship with unvaccinated patients as more difficult (DDPRQ-10 tool, P < 0.001, Cohen’s d = 0.85), perceived unvaccinated patients as more responsible for their medical condition (PPRQ tool, P < 0.001, Cohen’s d = 1.39) and perceived the character of vaccinated patients as a higher value character (CDQ tool, P < 0.001, Cohen’s d = 1.03).
None of the participants’ baseline characteristics correlated with results in any of the above tools. HCTs with higher workplace burnout (Shirom-Melamed Burnout Measure tool) perceived the relationship with unvaccinated patients as more difficult (DDPRQ-10 tool, r = 0.37, n = 66, P = 0.002). No other correlations were found between workplace burnout or anger (STAXI tool) and any of the other tools.
This study explored our hypothesis that patient COVID-19 vaccine hesitancy can have a negative effect on HCT perceptions. Our results showed that vaccine hesitancy had a negative impact on how the HCT perceived patients’ character, their care and their responsibility for their disease. We specifically addressed active physicians and nursing staff working in medical centers that treated COVID-19 patients, as they were directly affected by the pandemic. By approaching 11 different centers, our results may reflect the effect on HCT perceptions on a national scale. As stated above, several previous studies described the attitude of patients and medical personnel toward COVID-19 vaccines[12,13,21]. However, whether patients’ beliefs on this issue affect their treating team have yet to be described.
Our study was conducted during the fourth surge of the COVID-19 pandemic. Despite multiple studies demonstrating the safety and efficacy of mRNA vaccines[7,9,22], large populations still refuse to get vaccinated. Vaccination hesitancy continues to be a serious concern worldwide[23,24], with amplification of the discussion in social media settings[25]. During the fourth surge, most hospitalized patients were unvaccinated, showing worse clinical outcomes[10]. This situation created a fertile ground for the development of frustration among medical staff, particularly in the context of the highly stressful work environment in COVID-19 departments. We hypothesized that this confluence of factors might aggravate negative feelings while taking care of unvaccinated patients, as presented in our results. This trend was reflected in our study by the strong correlation between higher workplace burnout and the perception of more difficult relationships with unvaccinated patients.
In Israel, vaccines were free for every citizen and available in multiple centers all over the country with the option for home visits when needed. Therefore, it is not surprising that the unvaccinated COVID-19 patients in our study were considered responsible for their own medical predicament (P < 0.001) and were blamed for allowing the pandemic to spread, thus endangering others (P < 0.001). This dynamic can conceivably lead to more strain on the doctor-patient relationship. The results of the current study demonstrated the strong effect that vaccine status has on the HCT perceptions of their patients.
The use of three different study tools emphasized the internal consistency of the results since the negative attitude was consistent in three independent instruments. Additionally, the results of all three questionnaires were statistically significant, demonstrating a large effect, despite a relatively small sample size. It is important to note that 97% of the participants were vaccinated for COVID-19. While it may seem like a potential selection bias, it is important to remember that in Israel vaccination was obligatory for hospital medical teams, and therefore the vaccine status does not reflect the participants’ attitudes towards the COVID-19 vaccines[21].
Throughout the history of medicine, physicians have handled situations in which the patient may be held responsible for his condition due to various health behavior (e.g., obesity, diabetes, chronic obstructive pulmonary disease). Some medical conditions have even been stigmatized due to moral failure (e.g., venereal disease). Although it remains difficult to establish whether such perceptions play a role in the doctor–patient relationship, in all such cases medical professionalism and ethics call for a non-judgmental and unbiased approach toward patients. Additionally, the treating HCT must be familiar with variables that might influence their perceptions or interaction with their patients[26,27]. As shown by Mateo et al[28], there is a high prevalence of harmful bias and discrimination within the health professions, with a proven negative impact on patient care. It was argued that addressing these biases is the professional responsibility of every provider and essential to effective and equitable care. In light of this, we assumed that ongoing negative perceptions can eventually lead to a harmful effect on the quality of care of unvaccinated patients. We believe that our findings should raise awareness for potentially harmful biases in medical practice and hopefully lead to the establishment of specific measures in designated COVID-19 departments to combat this issue. For example, departments should be able to offer the staff a reassuring environment to express their feelings and prevent their aggravation.
This study has several limitations. We used questionnaires, which can cause report bias. Only participants who completed the questionnaire were included, which can cause selection bias. To avoid those biases, further research should aim to assess the effect of patient COVID-19 vaccine hesitancy on HCT perceptions in a direct manner. Observational prospective studies with consecutive patients are needed for this purpose and to assess any effect on patient quality of care. Furthermore, it can be assumed that since the reporting bias is a concern in both study groups, it has a relatively negligible influence on our results. Although we approached a variety of medical personnel in multiple centers, our cohort size is relatively small. A potential reason could be the timing of the study during the peak of an outbreak, finding the medical staff extremely busy and therefore less responsive to participate in online surveys, especially considering the multiple tools included in our questionnaire. Furthermore, even though the survey was anonymous, medical staff might have been hesitant to reveal negative attitudes toward patients. This study was designed as a “snapshot” study, capturing the essence of medical staff perceptions of COVID-19 patients during the peak of the outbreak.
Our study demonstrated that patient vaccine hesitancy had a strong negative effect on the HCT perceptions regarding these patients. We aimed to raise awareness and promote preventive interventions. Early detection might prevent negative feelings from escalating and mitigate the feared consequence of harming patient care.
Patient characteristics can affect their medical care team practice and intervene in the shared decision-making process. The coronavirus disease 2019 (COVID-19) pandemic posed new challenges to patient care, especially severe infections with high rates of deterioration and adverse outcomes. COVID-19 vaccines have proven highly efficacious in reducing the disease severity and as a result its burden. We, therefore, hypothesized that patient vaccine hesitancy would influence the hospital care team (HCT) perceptions.
Many studies focused on the attitudes toward COVID-19 vaccines themselves and specifically on vaccine hesitancy for both patients and medical teams. However, it is still unknown whether patient vaccine hesitancy influences HCT perceptions.
To study the effect of patient vaccine hesitancy on HCT perceptions towards these patients’ characteristics and care.
We conducted a prospective study at 11 medical centers during the Delta variant surge using standardized questionnaires. Hospital physicians and nursing staff treating COVID-19 patients (n = 66) were recruited and completed a questionnaire, which included three validated tools to assess the effect of patient vaccine hesitancy. We analyzed the questionnaire results in all different items and evaluated their associations with patients’ characteristics.
Our data demonstrated that HCT experienced their relationship with vaccine-hesitant patients as more difficult, perceived them as responsible for their disease and as having a lower character. The relationship with unvaccinated patients was more difficult among HCTs with higher workplace burnout.
We concluded that patient vaccine hesitancy had a negative impact on how the HCT perceived patient character, their care and their responsibility for their disease.
Our results should raise awareness of the potentially harmful biases in medical practice and hopefully lead to the establishment of specific measures in designated COVID-19 departments to combat this issue. Early detection might prevent negative feelings from escalating and mitigate the feared consequence of harming patient care.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, general and internal
Country/Territory of origin: Israel
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Lee S, South Korea; Tiejun W, China S-Editor: Zhang H L-Editor: Filipodia P-Editor: Zhang H
| 1. | van Ryn M, Burke J. The effect of patient race and socio-economic status on physicians' perceptions of patients. Soc Sci Med. 2000;50:813-828. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 945] [Cited by in RCA: 941] [Article Influence: 37.6] [Reference Citation Analysis (0)] |
| 2. | Keij SM, de Boer JE, Stiggelbout AM, Bruine de Bruin W, Peters E, Moaddine S, Kunneman M, Pieterse AH. How are patient-related characteristics associated with shared decision-making about treatment? BMJ Open. 2022;12:e057293. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 21] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 3. | Shepherd HL, Butow PN, Tattersall MH. Factors which motivate cancer doctors to involve their patients in reaching treatment decisions. Patient Educ Couns. 2011;84:229-235. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 36] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 4. | Wu JT, Leung K, Leung GM. Nowcasting and forecasting the potential domestic and international spread of the 2019-nCoV outbreak originating in Wuhan, China: a modelling study. Lancet. 2020;395:689-697. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3012] [Cited by in RCA: 2504] [Article Influence: 500.8] [Reference Citation Analysis (0)] |
| 5. | Krishnan A, Hamilton JP, Alqahtani SA, Woreta TA. COVID-19: An overview and a clinical update. World J Clin Cases. 2021;9:8-23. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 41] [Cited by in RCA: 31] [Article Influence: 7.8] [Reference Citation Analysis (1)] |
| 6. | Çelik MY, Kiliç M. Family relationship of nurses in COVID-19 pandemic: A qualitative study. World J Clin Cases. 2022;10:6472-6482. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 5] [Cited by in RCA: 8] [Article Influence: 2.7] [Reference Citation Analysis (4)] |
| 7. | Haas EJ, Angulo FJ, McLaughlin JM, Anis E, Singer SR, Khan F, Brooks N, Smaja M, Mircus G, Pan K, Southern J, Swerdlow DL, Jodar L, Levy Y, Alroy-Preis S. Impact and effectiveness of mRNA BNT162b2 vaccine against SARS-CoV-2 infections and COVID-19 cases, hospitalisations, and deaths following a nationwide vaccination campaign in Israel: an observational study using national surveillance data. Lancet. 2021;397:1819-1829. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1377] [Cited by in RCA: 1143] [Article Influence: 285.8] [Reference Citation Analysis (0)] |
| 8. | Chen LP, Zeng QH, Gong YF, Liang FL. Should people with chronic liver diseases be vaccinated against COVID-19? World J Clin Cases. 2021;9:7959-7962. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (2)] |
| 9. | Bar-On YM, Goldberg Y, Mandel M, Bodenheimer O, Freedman L, Kalkstein N, Mizrahi B, Alroy-Preis S, Ash N, Milo R, Huppert A. Protection of BNT162b2 Vaccine Booster against Covid-19 in Israel. N Engl J Med. 2021;385:1393-1400. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 826] [Cited by in RCA: 820] [Article Influence: 205.0] [Reference Citation Analysis (0)] |
| 10. | Freund O, Tau L, Weiss TE, Zornitzki L, Frydman S, Jacob G, Bornstein G. Associations of vaccine status with characteristics and outcomes of hospitalized severe COVID-19 patients in the booster era. PLoS One. 2022;17:e0268050. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 19] [Article Influence: 6.3] [Reference Citation Analysis (1)] |
| 11. | Vergara RJD, Sarmiento PJD, Lagman JDN. Building public trust: a response to COVID-19 vaccine hesitancy predicament. J Public Health (Oxf). 2021;43:e291-e292. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 77] [Cited by in RCA: 115] [Article Influence: 28.8] [Reference Citation Analysis (0)] |
| 12. | Pogue K, Jensen JL, Stancil CK, Ferguson DG, Hughes SJ, Mello EJ, Burgess R, Berges BK, Quaye A, Poole BD. Influences on Attitudes Regarding Potential COVID-19 Vaccination in the United States. Vaccines (Basel). 2020;8. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 318] [Cited by in RCA: 301] [Article Influence: 60.2] [Reference Citation Analysis (0)] |
| 13. | El-Elimat T, AbuAlSamen MM, Almomani BA, Al-Sawalha NA, Alali FQ. Acceptance and attitudes toward COVID-19 vaccines: A cross-sectional study from Jordan. PLoS One. 2021;16:e0250555. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 254] [Cited by in RCA: 247] [Article Influence: 61.8] [Reference Citation Analysis (0)] |
| 14. | Lievaart M, Franken IH, Hovens JE. Anger Assessment in Clinical and Nonclinical Populations: Further Validation of the State-Trait Anger Expression Inventory-2. J Clin Psychol. 2016;72:263-278. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 49] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 15. | Lundgren-Nilsson Å, Jonsdottir IH, Pallant J, Ahlborg G Jr. Internal construct validity of the Shirom-Melamed Burnout Questionnaire (SMBQ). BMC Public Health. 2012;12:1. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 283] [Cited by in RCA: 412] [Article Influence: 31.7] [Reference Citation Analysis (0)] |
| 16. | Hahn SR, Kroenke K, Spitzer RL, Brody D, Williams JB, Linzer M, deGruy FV 3rd. The difficult patient: prevalence, psychopathology, and functional impairment. J Gen Intern Med. 1996;11:1-8. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 227] [Cited by in RCA: 226] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 17. | Aloush V, Niv D, Ablin JN, Yaish I, Elkayam O, Elkana O. Good pain, bad pain: illness perception and physician attitudes towards rheumatoid arthritis and fibromyalgia patients. Clin Exp Rheumatol. 2021;39 Suppl 130:54-60. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 12] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 18. | Kelly JA, St Lawrence JS, Smith S Jr, Hood HV, Cook DJ. Stigmatization of AIDS patients by physicians. Am J Public Health. 1987;77:789-791. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 223] [Cited by in RCA: 204] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 19. | Brouns M. To what extent does the Belief in a Just World Theory offer insight in prevailing positive and negative attitudes toward Islamic and non-Islamic refugees in the Netherlands? Master Thesis Victomology Criminal Justice. 2016;. |
| 20. | Correia I, Vala J, Aguiar P. The Effects of Belief in a Just World and Victim's Innocence on Secondary Victimization, Judgements of Justice and Deservingness. Soc Justice Res. 2001;14:327-342. [DOI] [Full Text] |
| 21. | Gesser-Edelsburg A, Badarna Keywan H. Physicians' Perspective on Vaccine-Hesitancy at the Beginning of Israel's COVID-19 Vaccination Campaign and Public's Perceptions of Physicians' Knowledge When Recommending the Vaccine to Their Patients: A Cross-Sectional Study. Front Public Health. 2022;10:855468. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 14] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 22. | Tartof SY, Slezak JM, Fischer H, Hong V, Ackerson BK, Ranasinghe ON, Frankland TB, Ogun OA, Zamparo JM, Gray S, Valluri SR, Pan K, Angulo FJ, Jodar L, McLaughlin JM. Effectiveness of mRNA BNT162b2 COVID-19 vaccine up to 6 months in a large integrated health system in the USA: a retrospective cohort study. Lancet. 2021;398:1407-1416. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 959] [Cited by in RCA: 820] [Article Influence: 205.0] [Reference Citation Analysis (0)] |
| 23. | Khubchandani J, Sharma S, Price JH, Wiblishauser MJ, Sharma M, Webb FJ. COVID-19 Vaccination Hesitancy in the United States: A Rapid National Assessment. J Community Health. 2021;46:270-277. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 779] [Cited by in RCA: 726] [Article Influence: 181.5] [Reference Citation Analysis (0)] |
| 24. | Yang R, Penders B, Horstman K. Addressing Vaccine Hesitancy in China: A Scoping Review of Chinese Scholarship. Vaccines (Basel). 2019;8. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 55] [Cited by in RCA: 44] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 25. | Jiang X, Su MH, Hwang J, Lian R, Brauer M, Kim S, Shah D. Polarization Over Vaccination: Ideological Differences in Twitter Expression About COVID-19 Vaccine Favorability and Specific Hesitancy Concerns. Soc Media Soc. 2021;7. [DOI] [Full Text] |
| 26. | Hall JA, Stein TS, Roter DL, Rieser N. Inaccuracies in physicians' perceptions of their patients. Med Care. 1999;37:1164-1168. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 77] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 27. | Street RL Jr, Haidet P. How well do doctors know their patients? J Gen Intern Med. 2011;26:21-27. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 136] [Cited by in RCA: 146] [Article Influence: 10.4] [Reference Citation Analysis (0)] |
| 28. | Mateo CM, Williams DR. Addressing Bias and Reducing Discrimination: The Professional Responsibility of Health Care Providers. Acad Med. 2020;95:S5-S10. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 34] [Article Influence: 6.8] [Reference Citation Analysis (0)] |