Published online Dec 26, 2023. doi: 10.12998/wjcc.v11.i36.8574
Peer-review started: October 17, 2023
First decision: November 20, 2023
Revised: November 26, 2023
Accepted: December 15, 2023
Article in press: December 15, 2023
Published online: December 26, 2023
Processing time: 65 Days and 16.2 Hours
For the past few years, preventive interventional therapy has been widely used domestically and overseas, bringing great benefits to pregnant women at high-risk for complications, such as pernicious placenta previa (PPP) and placenta accreta. Nevertheless, there are still few reports on surgical complications related to interventional therapy, and its safety should be a concern.
We report a 36-year-old pregnant woman with PPP who underwent balloon implantation in the lower segment of the abdominal aorta before caesarean section. However, the balloon shifted during the operation, which damaged the arterial vessels after filling, resulting in severe postpartum haemorrhage in the patient. Fortunately, after emergency interventional stent implantation, the pa
It seems that massive postoperative bleeding has been largely avoided in preventive interventional therapy in high-risk pregnant women with placenta-related diseases, but surgical complications related to intervention therapy can also cause adverse consequences. It is equally important for clinical doctors to learn how to promptly identify and effectively treat these rare complications.
Core Tip: It is well known that postpartum haemorrhage is one of the most serious complications in malignant placenta previa caesarean section, and it is also the most concerning problem for medical staff. Currently, preventive interventional therapy has been able to prevent postpartum haemorrhage to a large extent, but its surgical complications need to be acknowledged, given that they are often overlooked. This article introduces a case of adverse consequences caused by a interventional therapy complication to provide some information for medical staff's clinical work.
- Citation: Gu DF, Deng C. Balloon displacement during caesarean section with pernicious placenta previa: A case report. World J Clin Cases 2023; 11(36): 8574-8580
- URL: https://www.wjgnet.com/2307-8960/full/v11/i36/8574.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i36.8574
Pernicious placenta previa (PPP) is placenta previa that occurs at the uterine scar incision from a previous caesarean section[1]. Uncontrolled and fatal postpartum haemorrhage is the main threat to such pregnant women. Research statistics have shown that[2] it is common for patients with placenta previa undergoing caesarean section to experience intraoperative bleeding of up to 3000 mL, this occurs in up to 90%, and approximately 10% of them even experience bleeding exceeding the rare 10000 mL. Massive postpartum haemorrhage can easily lead to complications such as haemorrhagic shock, disseminated intravascular coagulation, and multiple organ failure, endangering the safety of pregnant women and newborns[3]. Even in severe cases, some patients have to undergo hysterectomy, which can cause great harm to their physical and mental health[4]. In recent years, the use of abdominal aortic balloons to control bleeding has been widely used in caesarean section for placenta previa[5,6]. Temporarily filling the arterial balloon before stripping the placenta not only effectively reduces intraoperative blood loss, and provides a clear surgical field, but also more importantly, reduces the rate of hysterectomy[7]. However, this kind of intervention also has corresponding surgical complications[8], such as vascular injury, pseudoaneurysm, arterial thrombosis[9], ischaemia reperfusion injury, and foetal radiation exposure. We describe a rare complication that occurred during abdominal aortic balloon occlusion combined with caesarean section in a pregnant woman with PPP and give some opinions on this phenomenon.
A 36-year-old woman was admitted to the hospital to terminate her pregnancy due to a recurrence of brucellosis after 20 + 4 wk of pregnancy.
The patient experienced an elevated body temperature two weeks earlier, even reaching a maximum of 41 ℃. She took antibiotics and antipyretic analgesics for symptomatic treatment of her brucellosis. At the same time, this pregnant woman reported that the foetal movement response significantly decreased 10 d ago. Due to fear of medication leading to foetal intrauterine death or abnormalities, after her body temperature returned to normal, she went to our hospital to ask for termination of pregnancy.
The patient was diagnosed with brucellosis 6 mo ago. After symptomatic treatment in other hospitals, her condition improved, and since then, the patient stopped taking the medicine herself.
The patient denied any infectious disease and any relevant family history of placenta previa.
On physical examination, the patient’s vital signs were as follows: Body temperature, 36.1 ℃; blood pressure (BP), 113/79 mmHg; heart rate (HR), 91 beats per min; respiratory rate, 16 breaths per min, height, 165 cm; weight, 70 kg. Specialist inspection: The pregnant woman’s abdomen showed a gestational bulge with an abdominal circumference of 96 cm, and her pelvic floor was at the navel level. At this time, the foetal HR was 148 beats/min, but the contractions were not palpable. In gynaecological diagnosis, the cervical canal was not ruled out, the uterine orifice was not open, and the foetal membrane was not broken.
Routine blood tests showed a haemoglobin level of 85 g/L and a C-reactive protein level of 19.95 mg/L. Blood biochemical analysis indicated an albumin level of 28.5 g/L and a blood alkaline phosphatase level of 189.0 mmol/L.
Prenatal ultrasound examination revealed that the pregnant woman had central placenta previa and currently had subchorionic haemorrhage.
The patient was married at the age of 21 years. She had been pregnant a total of 5 times thus far, with two previous deliveries being caesarean sections (in 2008 and 2017) and two induced abortions.
The patient was diagnosed with placenta accreta without bleeding, central placenta previa, pregnancy with uterine scars, mid-term induced abortion, brucellosis, subchorionic haematoma, pregnancy with liver damage, pregnancy with hypoproteinaemia, pregnancy with anamia and pregnancy 5, delivery 2, and pregnancy 20 + 4 wk.
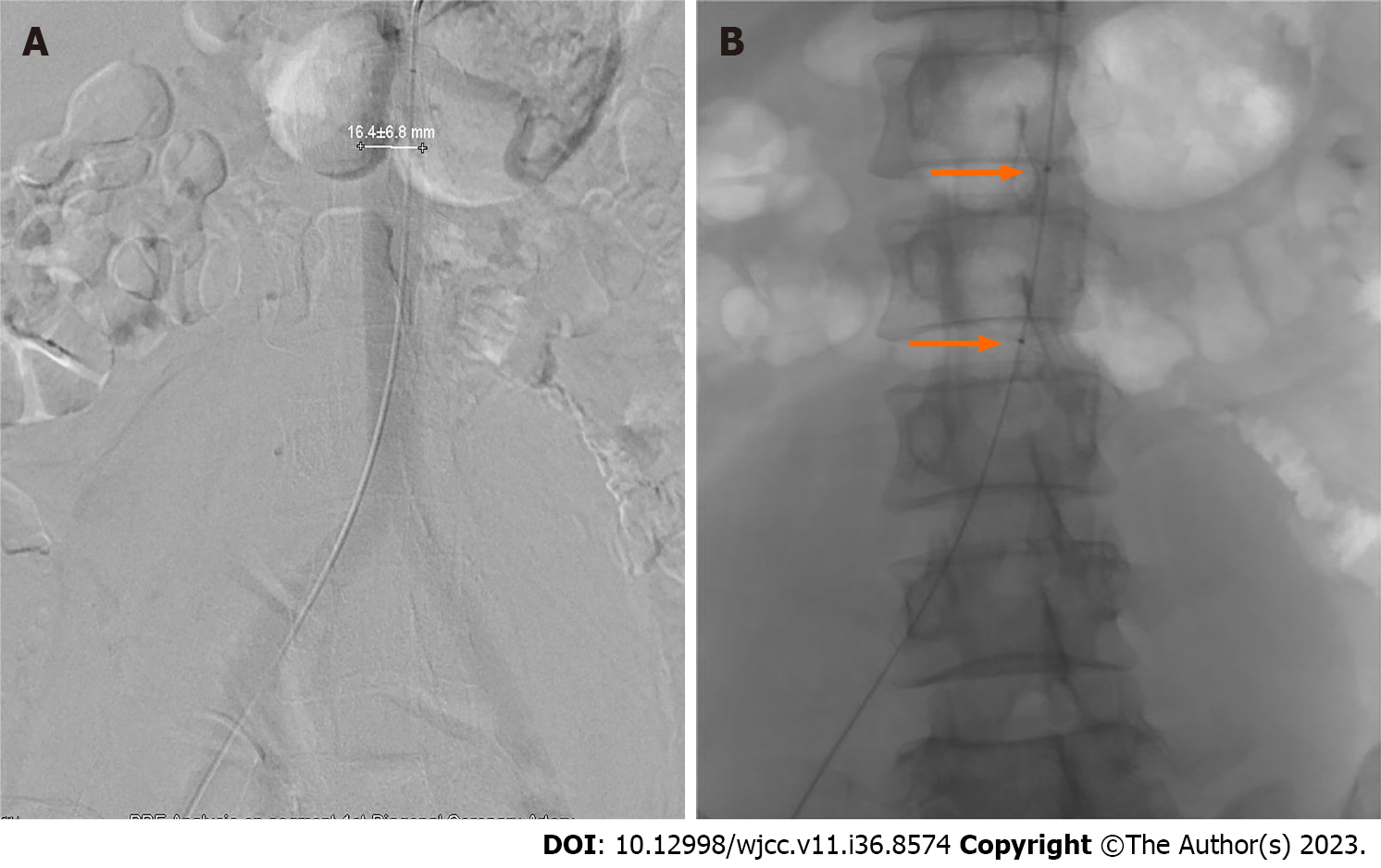
The patient experienced fever again after admission and sustained lower abdominal pain without any underlying cause. Urgent pelvic ultrasound examination revealed local detachment of the placenta. Considering the changes in the patient’s condition, it is recommended to undergo caesarean section and embryo removal surgery. Due to the clear diagnosis of central placenta previa and placenta accreta in the patient, there is a high possibility of acute massive bleeding during surgery. Therefore, to reduce the amount of bleeding, a balloon placement surgery in the lower segment of the abdominal aorta (Figure 1) was performed before the caesarean section, and immediately after the intervention surgery, a “transverse incision caesarean section for embryo retrieval in the lower segment of the uterus” was performed.
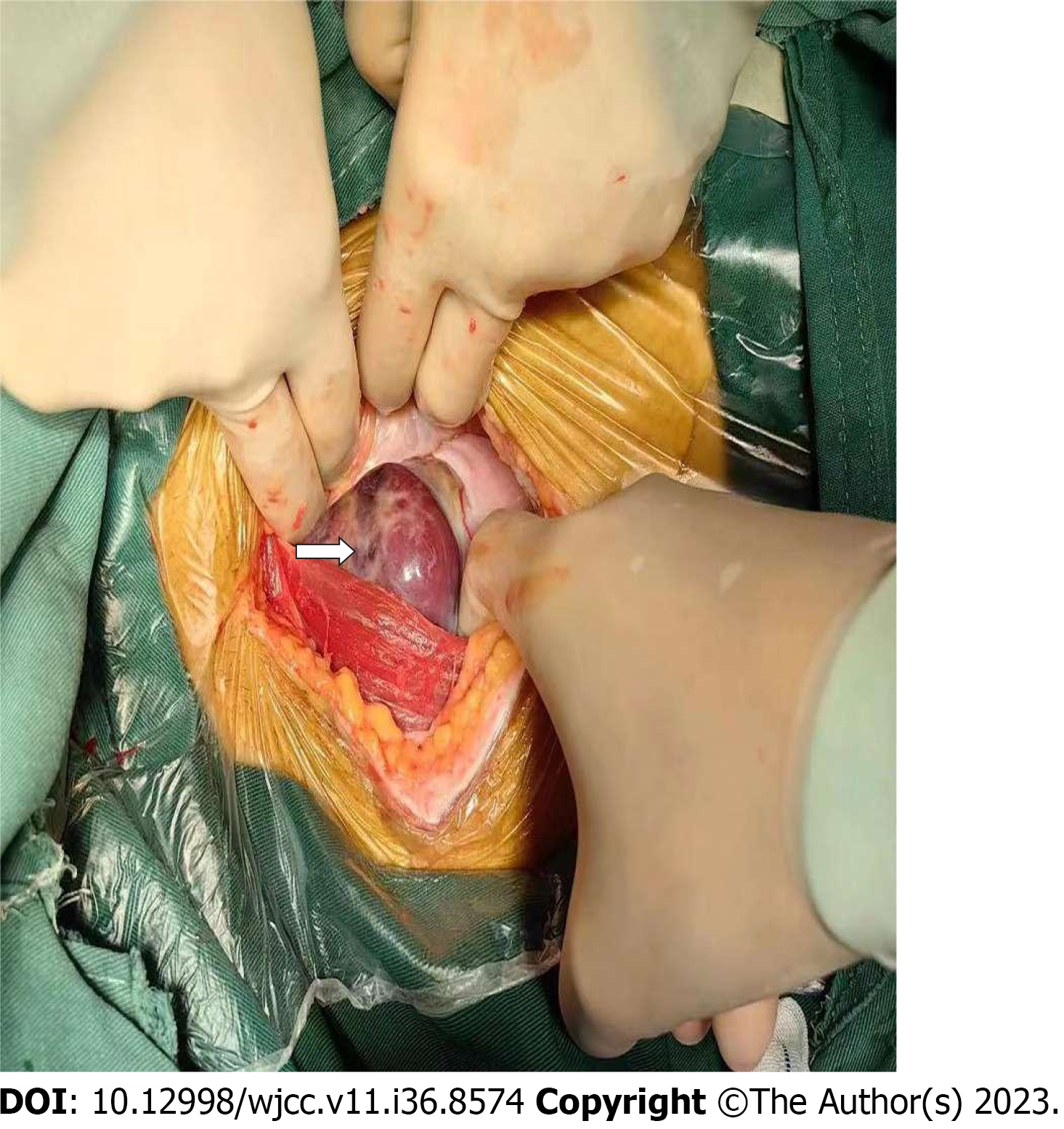
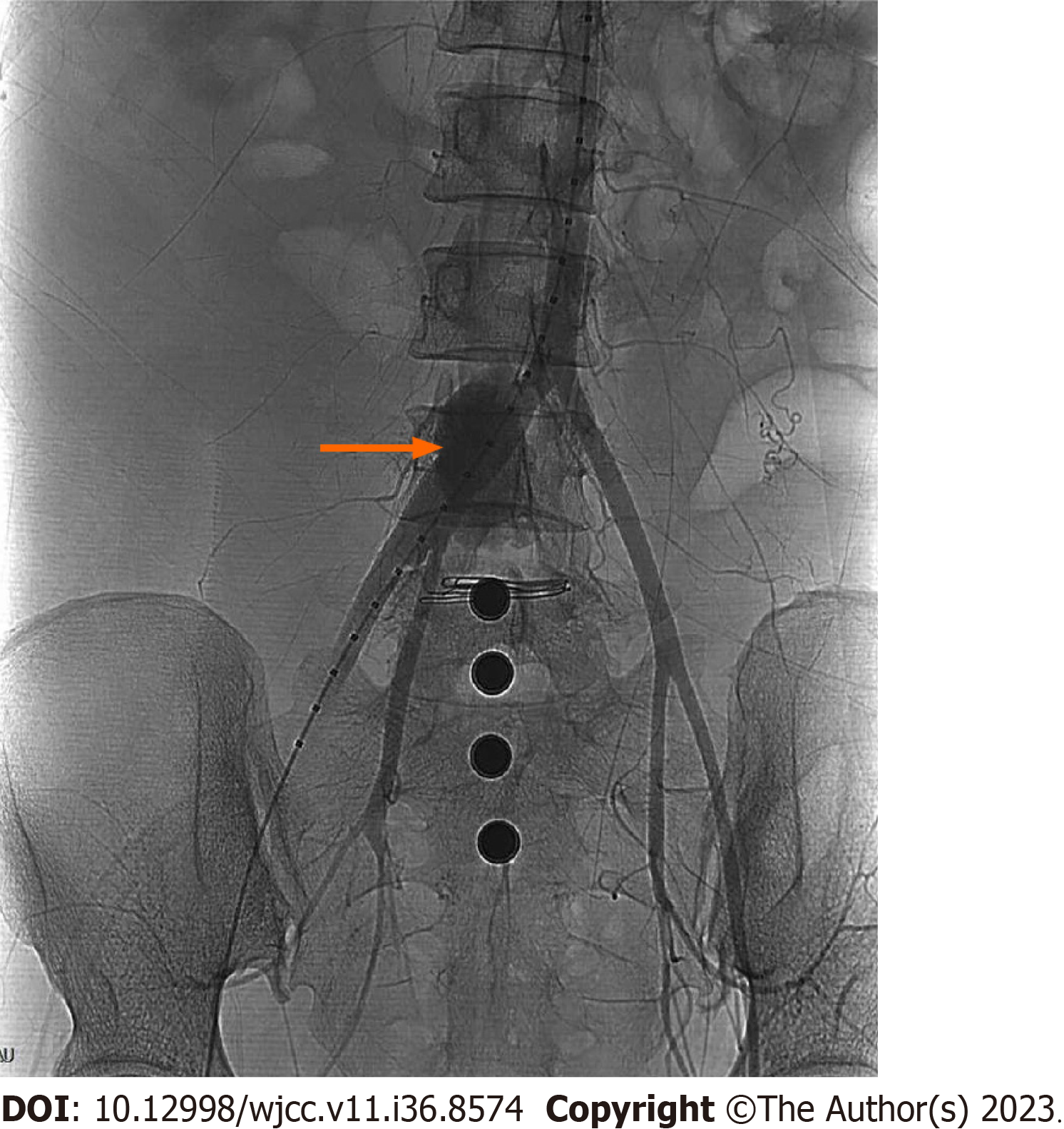
After entering the abdomen, it was found that the bladder peritoneum was tightly adhered to the the previous uterine scar. The placenta was implanted in the scar of the previous caesarean section of the uterus, and the surface blood vessels were dilated (Figure 2), making it impossible to push down the bladder peritoneum. The uterus was transversely cut 1cm above the scar, and a large amount of brownish-red purulent thread-like blood gushed out of the uterine cavity. After puncturing the amniotic membrane, a 470 g baby boy was delivered, but the foetus died, most likely due to intrauterine infection, then the pungent, pale yellow-green was immediately aspirated. After the delivery of the dead foetus, extensive implantation and adhesions of placental tissue were observed in the posterior wall, left and right walls, and lower segment of the uterus. Bleeding was active at the dissection site, and the obstetrician immediately filled the abdominal aortic balloon at this time. The blocking effect was observed to be poor, and the amount of bleeding did not decrease. Then, after the tourniquet was tied in the vascular free zone of the broad ligament in the lower segment of the uterus, the ascending branches of the bilateral uterine arteries were ligated, the posterior wall and the lower segment of the uterus were sutured with “8” shaped sutures for haemostasis and symptomatic treatment to promote uterine contraction, and the bleeding of the wound caused by the separation of uterus and placenta was reduced. Due to the time of filling of the abdominal aortic balloon up to 15 min, the balloon was immediately emptied. At this time, the patient’s BP suddenly dropped to 60/30 mmHg. Blood transfusion and fluid replacement were immediately performed to treat shock. At the same time, bilateral appendages and abdominal cavities were examined, and a dark red haematoma with a diameter of approximately 10 cm was found on the right side of the sacral promontory of the posterior peritoneum, with irregular range and significant fluctuations and no significant increase in BP after deep pressure treatment. We palpated the patient’s bilateral dorsalis pedis arteries, and the pulsation of the right artery was significantly weaker than that of the left. We had reason to suspect that the patient’s abdominal aortic balloon shifted and injured the artery after filling it. Immediate angiography was performed to confirm the diagnosis, and it was observed that the patient’s right common iliac artery was torn and bleeding, with blood extravasation forming a haematoma (Figure 3). Immediately, we requested that an interventional physician perform the right common iliac artery covered stent implantation surgery. Postoperative angiography showed that the lumen of the right common iliac artery was unobstructed, the stent was well unfolded, and no definite contrast agent leakage was observed. The ruptured vessel was successfully repaired (Figure 4), and the patient’s vital signs gradually stabilized. The total duration of this surgery was 5 h, with a blood loss of approximately 3000 mL. During the surgery, 10 U of red blood cell suspension and 1000 mL of plasma were transfused.
After the surgery, the patient was transferred to an intensive care unit for continued close monitoring, and received active treatment, such as anti-infection therapy, promotion of uterine contractions, and correction of anaemia. After recovery, the patient was discharged from the hospital.
With the reform of China’s family planning policy, the number of caesarean sections and the difficulty of surgery are constantly increasing, especially for high-risk pregnant women with placenta previa and placenta accreta spectrum (PAS) diseases. It has been reported that the incidence rate of PPP patients in China is 0.31%-0.89%, and approximately 53.3% of PPP patients have PAS[10], which means that obstetricians and anaesthesiologists face greater challenges. For pregnant women with placenta previa or placental implantation diseases, preoperative preventive intervention treatments such as abdominal aortic balloon implantation and uterine artery embolization allow doctors rescue patients with postpartum haemorrhage and have achieved significant results both domestically and internationally[11]. However, inevitably, there are still many worrisome aspects to interventional therapy, such as whether X-ray exposure is harmful to the foetus, whether preventive intervention surgery can completely avoid postpartum haemorrhage, and whether arterial blockade can cause ischaemi damage to other organs, which are all worthy of attention.
The main feature of our case is the occurrence of a rare complication, injury to the common iliac artery caused by filling the abdominal aortic balloon after unforeseen displacement.
The possible reasons for the occurrence of this rare complication are as follows: (1) The preoperative abdominal aortic balloon implantation surgery for patients undergoing caesarean section is performed using digital subtraction an
Summary of experience and lessons learned from this case: (1) For the delivery foetuses of pregnant women with PPP accompanied by placental implantation, it is necessary to pay attention to the prevention and treatment of severe post
Pregnant women with PPP often need preventive interventional therapy before undergoing caesarean section, which can significantly reduce the incidence of postpartum haemorrhage and a series of serious adverse consequences. However, the patient experienced a rare complication of balloon displacement, which led to more severe postpartum haemorrhage. Yet, after timely identification and multidisciplinary collaboration in diagnosis and treatment, the life of this pregnant woman was ultimately saved. Thus, any treatment method has complications, so regardless of the probability of occurrence, clinical doctors should remain vigilant, be prepared to face all possible critical situations, gain clinical experience, and protect the patient’s life.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Yarmahmoodi F, Iran S-Editor: Qu XL L-Editor: A P-Editor: Qu XL
| 1. | Kollmann M, Gaulhofer J, Lang U, Klaritsch P. Placenta praevia: incidence, risk factors and outcome. J Matern Fetal Neonatal Med. 2016;29:1395-1398. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 50] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 2. | Soyama H, Miyamoto M, Ishibashi H, Takano M, Sasa H, Furuya K. Relation between Birth Weight and Intraoperative Hemorrhage during Cesarean Section in Pregnancy with Placenta Previa. PLoS One. 2016;11:e0167332. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 3. | Matsuzaki S, Mandelbaum RS, Sangara RN, McCarthy LE, Vestal NL, Klar M, Matsushima K, Amaya R, Ouzounian JG, Matsuo K. Trends, characteristics, and outcomes of placenta accreta spectrum: a national study in the United States. Am J Obstet Gynecol. 2021;225:534.e1-534.e38. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 117] [Article Influence: 29.3] [Reference Citation Analysis (0)] |
| 4. | Horng HC, Lai MJ, Chang WH, Wang PH. Placenta accreta spectrum (PAS) and peripartum hysterectomy. Taiwan J Obstet Gynecol. 2021;60:395-396. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 14] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 5. | Wei Y, Luo J, Luo D. Comparison of Efficacy between Internal Iliac Artery and Abdominal Aorta Balloon Occlusions in Pernicious Placenta Previa Patients with Placenta Accrete. Gynecol Obstet Invest. 2019;84:343-349. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 14] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 6. | Huo F, Liang H, Feng Y. Prophylactic temporary abdominal aortic balloon occlusion for patients with pernicious placenta previa: a retrospective study. BMC Anesthesiol. 2021;21:134. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 15] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 7. | Wang Y, Huang G, Jiang T, Han X. Application of abdominal aortic balloon occlusion followed by uterine artery embolization for the treatment of pernicious placenta previa complicated with placenta accreta during cesarean section. J Interv Med. 2019;2:113-117. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 8. | Ben-David B, Kaligozhin Z, Viderman D. Quadratus lumborum block in management of severe pain after uterine artery embolization. Eur J Pain. 2018;22:1032-1034. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 9] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 9. | Wang ZX, Zhao YF, Li L. Is prophylactic intraoperative abdominal aortic balloon occlusion beneficial in pregnancies with placenta previa and placenta accreta spectrum during cesarean section? A 5-year retrospective study. Int J Gynaecol Obstet. 2023;163:572-578. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 10. | Zhou Y, Song Z, Wang X, Zhang M, Chen X, Zhang D. Ultrasound-based nomogram for postpartum hemorrhage prediction in pernicious placenta previa. Front Physiol. 2022;13:982080. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 11. | Zhang LL, Wang WH, Hou YL. Analysis of the Risk Factors for Massive Hemorrhage in Pernicious Placenta Previa and Evaluation of the Efficacy of Internal Iliac Artery Balloon Occlusion. Int J Womens Health. 2022;14:1769-1776. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 7] [Reference Citation Analysis (0)] |
| 12. | Li N, Yang T, Liu C, Qiao C. Feasibility of Infrarenal Abdominal Aorta Balloon Occlusion in Pernicious Placenta Previa Coexisting with Placenta Accrete. Biomed Res Int. 2018;2018:4596189. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 16] [Article Influence: 2.3] [Reference Citation Analysis (0)] |