Published online Dec 26, 2023. doi: 10.12998/wjcc.v11.i36.8557
Peer-review started: October 3, 2023
First decision: November 22, 2023
Revised: November 28, 2023
Accepted: December 11, 2023
Article in press: December 11, 2023
Published online: December 26, 2023
Processing time: 79 Days and 23.4 Hours
The procedure for microwave endometrial ablation (MEA) follows established MEA practice guidelines but requires hysteroscopic observation of the uterine lumen before and after MEA. When a luminal uterine lesion is recognized, its removal requires preoperative dilation of the cervix because the outer diameter of a conventional rigid hysteroscope is 8.7 mm. Recently, a fully disposable rigid hysteroscope (LiNA OperaScopeTM) with a narrow diameter (4.4 mm) and forceps capable of extracting endometrial lesions has become available.
Here, we report a case of heavy menstrual bleeding (HMB) complicated by endometrial polyps where MEA was performed after removing endometrial polyps using the LiNA OperaScopeTM device. A 48-year-old woman with three prior pregnancies and three deliveries was referred to our hospital for further examination and treatment after being diagnosed with HMB 2 years earlier. The patient underwent MEA following endometrial polypectomy using LiNA OperaScopeTM. After MEA, endometrial cauterization was again examined using the LiNA OperaScopeTM, and the procedure was completed. No preoperative cervical dilation was performed. The patient’s clinical course was favorable, and she was discharged 3 h after surgery. One month after surgery, menstruation resumed, and both HMB and dysmenorrhea improved markedly from 10 preoperatively to 1 postoperatively, as assessed subjectively using the visual analog scale. The patient’s postoperative course was uneventful with no complications.
LiNA OperaScopeTM can be a minimally invasive treatment for MEA of HMB with uterine lumen lesions.
Core Tip: LiNA OperaScopeTM is a fully disposable rigid hysteroscope with an outer diameter of 4.4 mm, narrower than conventional hysteroscopes, and equipped with forceps capable of excising endometrial lesions. We report a case of heavy menstrual bleeding (HMB) with endometrial polyps where microwave endometrial ablation (MEA) was performed after endometrial polyp removal using LiNA OperaScopeTM. This case suggests that MEA using the LiNA OperaScopeTM can remove luminal lesions without preoperative cervical dilation and can be a less invasive treatment option than conventional techniques for patients with HMB presenting with endometrial polyps.
- Citation: Kakinuma K, Kakinuma T, Ueyama K, Shinohara T, Okamoto R, Yanagida K, Takeshima N, Ohwada M. LiNA OperaScopeTM for microwave endometrial ablation for endometrial polyps with heavy menstrual bleeding: A case report. World J Clin Cases 2023; 11(36): 8557-8562
- URL: https://www.wjgnet.com/2307-8960/full/v11/i36/8557.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i36.8557
Heavy menstrual bleeding (HMB) is defined as heavy menstrual blood loss, severe anemia, and difficulty in daily living. It limits social activities due to the decrease in a woman’s quality of life. Although pharmacological treatment with hemostatic agents and hormones is often the first choice for HMB, hysterectomy is a curative treatment for patients who are unresponsive to conservative treatment and have no desire for a baby. However, many patients desire less invasive treatments due to preexisting conditions, complications, or social background.
Microwave endometrial ablation (MEA) is an ultrasound-guided method of endometrial ablation using microwave irradiation at 2.45 GHz. MEA is a treatment method that destroys the endometrium, including its basal layer, using a protein coagulator that uses dielectric heating produced by microwave irradiation of the tissue, thereby reducing its function. It aims to achieve a decrease in menstrual blood volume or transition to amenorrhea. MEA has gained popularity as a minimally invasive alternative to conventional hysterectomy, and its usefulness has been reported at our institution and others[1-3]. The procedure is performed following the MEA[4] guidelines and requires hysteroscopic observation of the uterine lumen before and after MEA. If there is an elevated lesion in the uterine lumen, it should be removed. When excising a bulging lesion under hysteroscopy, the cervix must be dilated preoperatively because the outer diameter of a conventional rigid hysteroscope is 8.7 mm. In recent years, a fully disposable rigid hysteroscope (LiNA OperaScopeTM) with an outer diameter of 4.4 mm, narrower than conventional hysteroscopes, and equipped with forceps capable of excising endometrial lesions, has been introduced.
Here, we report a case of HMB with endometrial polyps in which MEA was performed after endometrial polyp removal using LiNA OperaScopeTM.
The patient, a 48-year-old woman with three prior pregnancies and three vaginal deliveries, presented with HMB.
The patient had been experiencing HMB for 2 years. She visited her local doctor and was found to be anemic (hemoglobin level: 7.9 mg/dL). Subsequently, she was referred to our hospital for further examination and treatment.
First menstruation at age 11 years; 28-d cycle; duration, 6 d; regular, characterized by heavy menstrual blood with clots and severe dysmenorrhea.
There was no pertinent history.
On admission, she was 160.0 cm tall, weighed 55.0 kg, and had a body surface area of 21.5 kg/m2. She was fully conscious. Her blood pressure was 123/78 mmHg, pulse rate was 99/min, and SpO2 was 99% (supine position, room air).
Cytological examination of cervical specimens was negative for intraepithelial lesions or malignancy. Cytological examination of the endometrial samples was also negative.
Ultrasonography in the follicular phase revealed irregular thickening of the endometrium, and endometrial polyps were suspected.
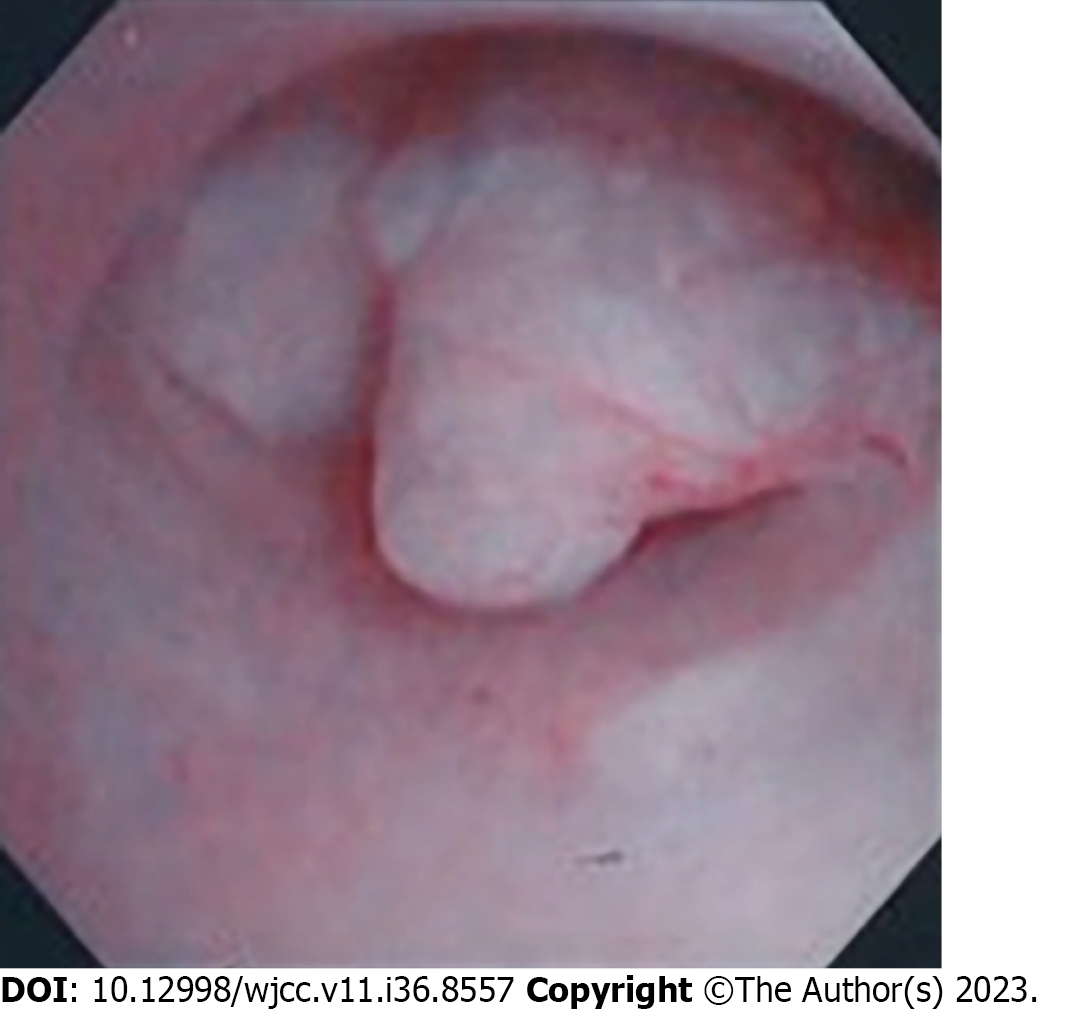
Hysteroscopic examination revealed a pale-red, elevated lesion in the lower part of the uterine body (Figure 1).
Based on these findings, abnormal uterine bleeding with polyps was diagnosed according to the International Federation of Gynecology and Obstetrics Abnormal Uterine Bleeding System.
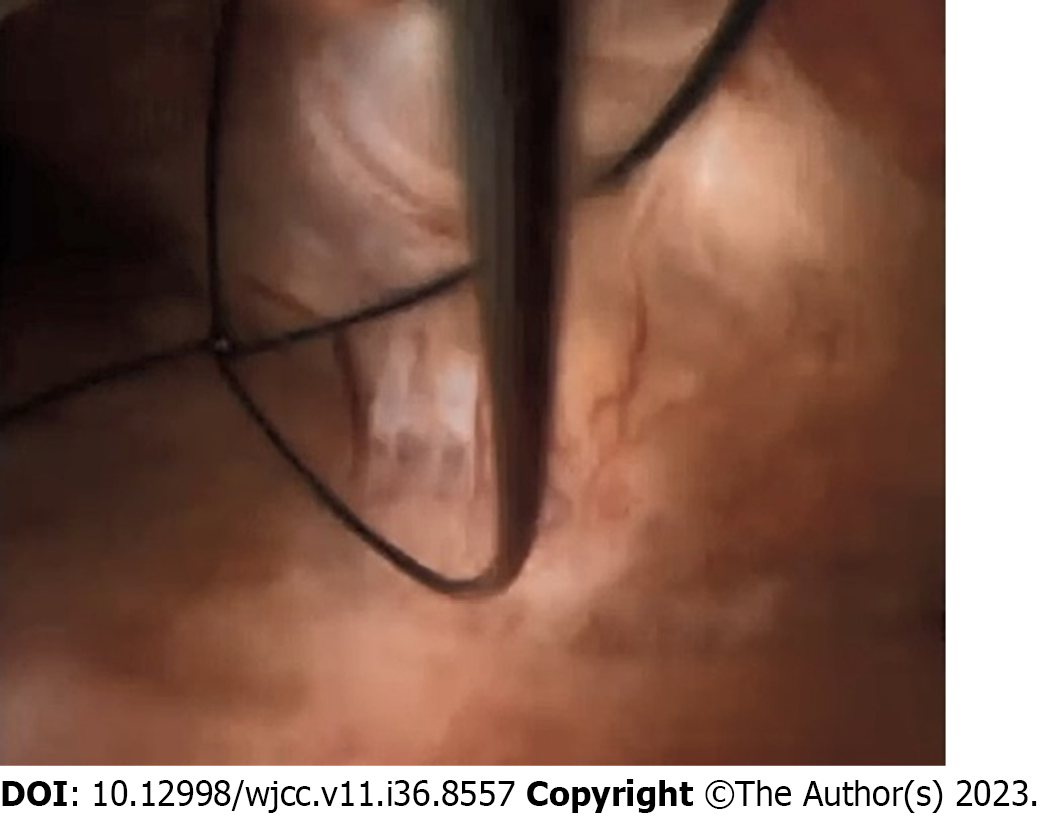
Surgery was initiated with the patient in the lithotripsy position under general anesthesia. After observing the uterine lumen using the LiNA OperaScopeTM device (Terumo Corporation, Tokyo, Japan) (Figure 2), endometrial polyps were excised using basket forceps (Figure 3). MEA was performed under transabdominal ultrasound guidance after endometrial polypectomy using a Microtase AFM-712 device (Alfresa Pharma Corporation, Osaka, Japan) and a sounding applicator, CSA-40CBL-1006200C (Alfresa Pharma Corporation), to cauterize the endometrium with a microtase output of 70 W and a coagulation energization time of 50 S per cycle. After MEA, the uterine cavity was again observed with the LiNA OperaScopeTM to confirm that the endometrium was coagulated and necrotic, cauterization did not extend into the endometrial or cervical mucosa, and no necrotic tissue was retained by the endometrial cautery (Figure 4). Preoperative cervical dilation was unnecessary. The operative time was 33 min, and blood loss was minimal.
The patient’s progress was favorable; she was discharged 3 h after surgery and followed up as an outpatient. Histopathological examination of the excised specimen revealed the presence of an endometrial polyp. The patient resumed menstruating 1 mo postoperatively, and both HMB and dysmenorrhea improved markedly (from 10 to 1 on subjective evaluation using the visual analog scale). No complications occurred during the patient’s clinical course, and the postoperative course was favorable. As of postoperative month 6, there was no HMB recurrence.
MEA is a treatment for functional or organic hypermenorrhea in which the endometrium is destroyed using microwave ablation. MEA is considered less invasive than hysterectomy; therefore, its effectiveness as an alternative treatment to hysterectomy has been reported in cases where the perioperative risk is considered high due to medical complications, obesity, or previous abdominal surgery. This procedure is also gaining widespread use as a treatment characterized by high patient satisfaction[1-3].
For the implementation of MEA, we followed the Guidelines for the Implementation of Microwave Endometrial Ablation (2012 revision), published in Japan, that describes the details of the MEA procedure with safety assurances[4]. These guidelines state that MEA should be performed under ultrasound guidance and that the endometrium should be observed with a hysteroscope before and after MEA, especially to ensure no uncauterized endometrium at the end of the cautery. The presence of an uncauterized portion of the endometrium is also an important risk factor for HMB recurrence after MEA. Complications of MEA include thermal injury to the pelvic organs, cervical stenosis, retained uterine fluid due to endometrial cauterization, retained uterine hematochezia, pelvic inflammation such as endometritis from an ascending infection, and retained uterine pyometra[5]. Therefore, if the cauterization is extended to the endometrial or cervical mucosa, the cervix must be dilated postoperatively to prevent cervical stenosis and adhesions. In the present case, intrauterine infection was observed postoperatively[3]. Thus, we took precautionary steps to excise as much necrotic tissue as possible that remained due to endometrial ablation when checking the status of endometrial ablation using hysteroscopy immediately after MEA. Observation of the uterine lumen via hysteroscopy after MEA is also important to avoid complications.
A microwave surgical instrument and microwave applicator are required to perform MEA. A sounding applicator manufactured by Alfresa Pharma was used[6]. Because its diameter is as thin as 4 mm, cervical dilation is not necessary if only the observation of the uterine lumen is required.
As explained in the MEA guidelines, no endometrial lesions suggestive of malignancy should be confirmed before MEA. If a luminal uterine lesion is present, as in the present case, removal is required for histopathological evaluation. It is important to exclude malignant lesions from the uterus lumen before MEA. However, in a report from our institution, despite the preoperative exclusion of malignant endometrial lesions via endometrial cytology and histology, malignant endometrial lesions were found during endometrial histology during MEA[7]. In addition, atypical polypoid adenomyoma (APAM) is a mixed epithelial-stromal tumor that develops in a polypoid shape in the uterine lumen. Although APAM is classified as a benign tumor, it is associated with endometrial hyperplasia and endometrial adenocarcinoma and has a high risk of recurrence and progression to endometrial cancer[8]. Hysteroscopy is also useful for observing the degree of protrusion and coloration of the lesion and abnormal vascular images on the lesion surface. In recent years, the usefulness of transcervical resection has been highlighted in cases where it is difficult to evaluate benign or malignant lesions via preoperative histological examination; it can be used for luminal uterine lesions that are difficult to evaluate using magnetic resonance imaging or ultrasound tomography[9-11].
Using a conventional rigid hysteroscope (diameter, 8.7 mm) for this procedure would require cervical dilation prior to MEA. The smaller 4.4 mm outer diameter of the LiNA OperaScopeTM used in the present case allowed us to remove the lesion in the uterine lumen without preoperative cervix dilation. The lack of preoperative dilation of the cervix may enable a more minimally invasive procedure for MEA in HMB with luminal uterine lesions. In the present case, the patient was discharged within 3 h after surgery. If this procedure can be performed under local anesthesia, such as a paracervical block, it may be possible to perform it as an outpatient procedure without requiring hospitalization.
In addition, because this hysteroscopic instrument has a liquid crystal display, a light source with a built-in light-emitting diode, and a power supply with built-in dry batteries, and all parts are integrated into one unit, this one instrument alone is sufficient to observe the uterine cavity and remove lesions. Therefore, unlike conventional rigid hysteroscopic surgical systems, this does not incur high initial investment costs. Furthermore, as this device is a disposable, single-use product, it reduces the risk of infection and reduces the labor required by medical personnel to clean and sterilize surgical instruments.
The forceps that can be used with this device are limited to biopsies, scissors, and basket-type forceps. However, it is not equipped with a device with a hemostatic function using a high-frequency current generator or other heat source. It is not indicated for masses that protrude into the uterine lumen at a low rate or for lesions that bleed easily and are difficult to control.
The LiNA OperaScopeTM has been on the market for only a short time. Therefore, it is necessary to conduct clinical verification from various perspectives, such as histopathological examination of the extracted material, postoperative complications, HMB recurrence rate, time until recurrence, selection of cases prone to recurrence in MEA for HMB with uterine lumen lesions using this device, and detailed studies on the indications for this procedure prior to its widespread use.
MEA using the LiNA OperaScopeTM can remove luminal lesions without requiring preoperative cervical dilation and can be a less invasive treatment option than conventional techniques for patients with HMB presenting with endometrial polyps.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: Japan
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): 0
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Zhang S, China S-Editor: Lin C L-Editor: Filipodia P-Editor: Zhao S
| 1. | Sharp NC, Cronin N, Feldberg I, Evans M, Hodgson D, Ellis S. Microwaves for menorrhagia: a new fast technique for endometrial ablation. Lancet. 1995;346:1003-1004. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 99] [Cited by in RCA: 100] [Article Influence: 3.3] [Reference Citation Analysis (1)] |
| 2. | Hodgson DA, Feldberg IB, Sharp N, Cronin N, Evans M, Hirschowitz L. Microwave endometrial ablation: development, clinical trials and outcomes at three years. Br J Obstet Gynaecol. 1999;106:684-694. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 83] [Cited by in RCA: 84] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 3. | Kakinuma T, Kaneko A, Kakinuma K, Matsuda Y, Yanagida K, Takeshima N, Ohwada M. Effectiveness of treating menorrhagia using microwave endometrial ablation at a frequency of 2.45 GHz. World J Clin Cases. 2023;11:5653-5659. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 4. | Kanaoka Y, Ishikawa N, Asakawa Y, Nakayama K. Practice Guideline of MEA 2012. Apr 1, 2012. [cited 4 September 2023]. Available from: https://www.alfresa-pharma.co.jp/microtaze/MEAguideline2012.pdf. |
| 5. | Das S, Kirwan J, Drakeley AJ, Kingsland CR. Pelvic abscess following microwave endometrial ablation. BJOG. 2005;112:118-119. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 6. | Kanaoka Y, Hirai K, Ishiko O. Microwave endometrial ablation for an enlarged uterus. Arch Gynecol Obstet. 2003;269:30-32. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 17] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 7. | Kakinuma T, Kakinuma K, Tanaka H, Ohwada M. Considerations for performing microwave endometrial ablation (MEA) - Three cases with abnormal test results of endometrial tissue discovered by chance when performing MEA. Int J Hyperthermia. 2020;37:749-752. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 8. | Heatley MK. Atypical polypoid adenomyoma: a systematic review of the English literature. Histopathology. 2006;48:609-610. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 74] [Cited by in RCA: 72] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 9. | Engelberg D, Pankratieva E, Liauchonak I. Diagnostic value of hysteroscopy in abnormal uterine bleeding. Can Fam Physician. 2018;64:442-444. [PubMed] |
| 10. | Yang B, Xu Y, Zhu Q, Xie L, Shan W, Ning C, Xie B, Shi Y, Luo X, Zhang H, Chen X. Treatment efficiency of comprehensive hysteroscopic evaluation and lesion resection combined with progestin therapy in young women with endometrial atypical hyperplasia and endometrial cancer. Gynecol Oncol. 2019;153:55-62. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 72] [Article Influence: 12.0] [Reference Citation Analysis (0)] |
| 11. | Yamagami W, Susumu N, Ninomiya T, Nakadaira N, Iwasa N, Kuwahata M, Nomura H, Kataoka F, Banno K, Aoki D. Hysteroscopic transcervical resection is useful to diagnose myometrial invasion in atypical polypoid adenomyoma coexisting with atypical endometrial hyperplasia or endometrial cancer with suspicious myometrial invasion. J Obstet Gynaecol Res. 2015;41:768-775. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 1.0] [Reference Citation Analysis (0)] |