Published online Dec 26, 2023. doi: 10.12998/wjcc.v11.i36.8551
Peer-review started: September 23, 2023
First decision: November 17, 2023
Revised: December 2, 2023
Accepted: December 8, 2023
Article in press: December 8, 2023
Published online: December 26, 2023
Processing time: 89 Days and 16.9 Hours
Spontaneous gastric hematoma is an exceedingly rare condition characterized by the accumulation of blood within the gastric wall without any apparent iatrogenic or traumatic cause. Coagulopathies are the most frequent cause of gastric he
We present the case of a spontaneous gastric hematoma in a 22-year-old male. He presented to our emergency department complaining of pain in the left flank area lasting for 2 wk. There was no history of trauma, anticoagulant medications or endoscopy procedures. His hemoglobin and hematocrit levels were slightly lower than normal. Multi-slice computed tomography, ultrasound and endoscopy confirmed a gastric intramural hematoma. We recommended conservative treatment because there was no hemodynamic instability nor significant bleeding. The patient responded well, and there were no unexpected events. At the 3-mo follow-up, the ultrasound exa
After reviewing the literature and our experience, we recommend that more of these cases should be treated conservatively. The tendency to treat these cases with potentially burdensome procedures such as total or subtotal gastrectomy should be significantly reduced.
Core Tip: It is our intention to emphasize spontaneous gastric intramural hematoma as one of possible causes of acute abdomen. Also we would like to underline the option for conservative treatment of this condition. With our experience and by reviewing the literature we are under impression that majority of these cases could have been treated conservatively and number of surgical procedures could be reduced to some extent.
- Citation: Budimir I, Žulec M, Eljuga K, Židak M, Lisek V. Spontaneous gastric hematoma as a rare cause of acute abdomen: A case report. World J Clin Cases 2023; 11(36): 8551-8556
- URL: https://www.wjgnet.com/2307-8960/full/v11/i36/8551.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i36.8551
Intramural hematomas of the gastrointestinal tract are uncommon lesions. They most commonly occur in the esophagus and duodenum[1]. Spontaneous gastric hematoma is a rare clinical entity characterized by the accumulation of blood within the gastric wall in the absence of trauma or an underlying gastrointestinal pathology. Coagulopathies are the most frequent cause of gastric hematomas. However, other causes include amyloidosis, pancreatitis, visceral vascular aneu
A 22-year-old male presented to our emergency department with a complaint of persistent blunt abdominal pain in the left flank that first occurred 2 wk prior.
The patient stated that he vomited and had diarrhea a few days prior to the onset of pain. These symptoms were interpreted as gastroenteritis and resolved spontaneously. The patient denied a history of trauma or recent endoscopic procedures and was not taking anticoagulant medications. It is known that some patients, especially younger ones, do not mention abdominal trauma because they do not recognize it as a trauma or because they want to hide illicit or inappropriate behavior[5,6]. However, we ruled out these possibilities for this patient.
Chronic illnesses and bleeding disorders were absent. There was no history of trauma nor endoscopy procedures.
There was no family history of blood disorders, vascular diseases nor gastrointestinal diseases.
Physical examination revealed tenderness in the left flank and epigastric region but with no signs of peritoneal irritation. There was a palpable mass below the left costal arch. It was 10 cm in diameter, spheric, soft and mildly painful on palpation. There were no signs of any type of trauma such as bruises or excoriations. The vital parameters (blood pressure, respiration and pulse) were all within normal ranges. Digital rectal examination did not show any abnor
Initial blood count showed slightly lower hemoglobin (123 g/L; normal range: 138-175 g/L) and hematocrit (0.367 L/L; normal range: 0.415-0.530 L/L). All other laboratory findings, including coagulation profile, were within normal ranges.
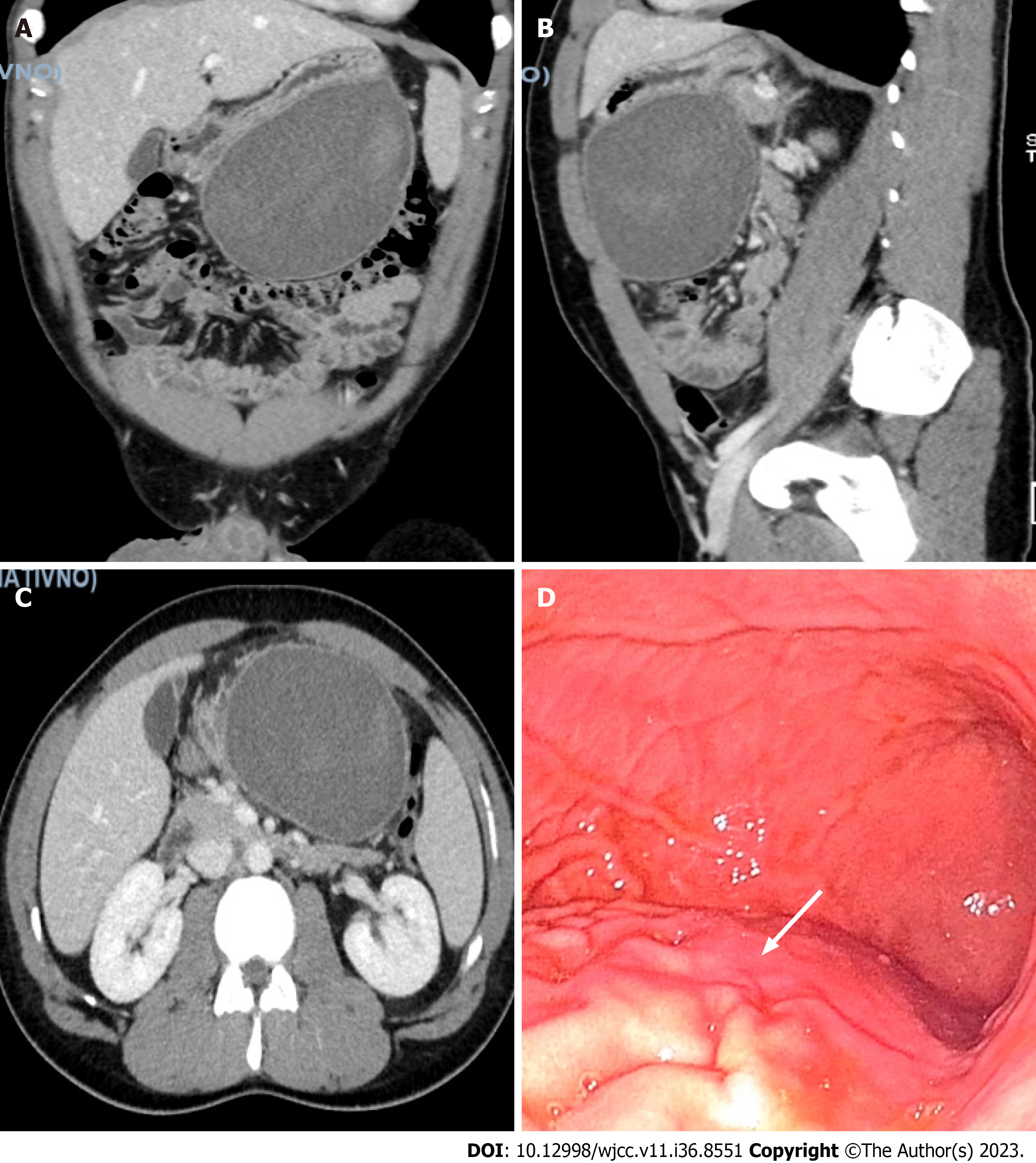
An abdominal ultrasound demonstrated a thickened and hypoechoic gastric wall. The radiologist determined the findings to be inconclusive but indicated a suspicion of an intramural hematoma. An abdominal contrast-enhanced multi-slice computed tomography examination confirmed a heterogenous intramural mass within the gastric wall, measuring approximately 15 cm × 11 cm × 9 cm (Figure 1A-C). There were no signs of calcifications specific to malignant lesions nor gastrointestinal stromal tumor (GIST)-specific cystic masses. The described mass had the density of a hematoma[7].
Endoscopic evaluation was performed to assess the source of bleeding and to rule out any underlying pathology. Esophagogastroduodenoscopy revealed a large, submucosal mass occupying the greater curvature of the stomach (Figure 1D). There were no signs of active bleeding, ulcers nor mucosal lesions. Neither endophytic growth nor lumen obstruction were present, providing additional support against the suspicion of GIST[8].
Spontaneous gastric intramural hematoma (GIH).
We opted to not perform ultrasound-guided biopsy. The patient was hospitalized and conservative treatment was chosen because of the absence of active bleeding and the presence of hemodynamic stability. The patient received pantoprazole, a proton pump inhibitor (PPI) (40 mg every morning, by mouth). Metamizole (500 mg) was administered for analgesia as needed, by mouth. The patient only received metamizole for the 1st 2 d, as his pain decreased significantly. Serial ab
Over the course of several days, the patient’s symptoms were significantly relieved. Repeated abdominal ultrasound showed a gradual decrease of the hematoma, and the hemoglobin level remained the same. The patient was discharged after 4 d with instructions for a soft diet and continued pantoprazole therapy as during the hospitalization.
The first follow-up examination was completed 2 wk after discharge. Laboratory findings were within normal limits. The patient stated that he did not experience any pain, did not use any analgesics and was following the diet and medication instructions. Ultrasound also showed a significant decrease in the mass. The patient was instructed to discontinue pantoprazole. A soft diet was unnecessary because he was not at risk for mechanical erosions of the mucosa and sub
Spontaneous GIH is a rare clinical entity that presents unique challenges for diagnosis and management. GIH was first described by MacLauchlan in 1838 and described as a pseudoaneurysmal tumor of the duodenum[9]. However, almost 200 years later, the pathophysiology is still not completely understood. When GIST is the working diagnosis, post
GIH is mostly caused by coagulopathy, peptic ulcers, fishbone ingestion and endoscopy procedures. In these types of cases, the patient has a higher chance of being appropriately diagnosed and managed, which is often not the case with idiopathic GIH.
Several studies have shown that the majority of GIH cases are treated conservatively. However, in idiopathic cases, surgery has been the treatment of choice in more than half of the patients[2,3]. Conservative treatment regimens include blood and coagulation factor replacement for cases of intrinsic coagulopathy[11]. When warfarin overdose is the cause, patients are treated with coagulopathy reversal[4,11]. The discontinuation of aspirin prior to an endoscopic or other invasive procedure, such as percutaneous gastrostomy, can prevent the development of GIH[12]. After reviewing the literature, it was apparent that no standard treatment protocol exists. Treatment was personalized according to the supposed cause of GIH and the individual patient’s symptoms[4,7,11-13].
Tabbikha et al[2] conducted a literature review of spontaneous GIH cases published in English. Their case report was the seventh published case. They found that 5 of 7 patients were treated surgically with total or subtotal gastrectomy or wedge gastric resection[2]. We found in our literature search that most GIH cases were misdiagnosed as visceral artery aneurysms, GIST, tuberculosis, or Dieulafoy’s lesion[2,7,11]. Spontaneous GIH was rarely the initial diagnosis[10,14-16] and was confirmed in most cases after surgical intervention. If the diagnosis of GIH is confirmed earlier, then gastrectomies and other surgical procedures could be decreased. We found that conservative treatment was successful in the cases initially diagnosed with spontaneous GIH[17].
Even though we did not complete a biopsy of the specimen, the absence of cystic masses and calcifications on multi-slice computed tomography assisted in excluding carcinomas and GIST[7,8]. Ultrasound findings were inconclusive but suggested GIH. The lack of the biopsy is one of the limitations in the management of this case because we did not confirm GIH pathohistologically. However, the patient was young and there were no indications of malignancy. Therefore, we determined that the risks of a biopsy outweighed the benefits.
Our patient was hemodynamically stable and responded well to analgesics. Therefore, conservative treatment was recommended. Interestingly, no publications on GIH cases mentioned that the patients were hemodynamically instable. Even though patients in the other published reports were initially diagnosed with superior mesenteric artery branch aneurysm, severely bleeding GIST or peptic ulcers, they were hemodynamically stable[3,7,13]. Some studies reported tachycardia and decreased hemoglobin levels, but the patients were normotensive[2,3,7,13,17].
Due to the scarcity of cases, we are aware that we do not have enough data nor experience to strongly recommend a conservative treatment protocol for all spontaneous GIH cases. However, we postulate that presentations similar to our patient are likely seen more frequently in emergency departments and are not widely reported. Therefore, it is important to recognize that a conservative treatment approach would be beneficial for such patients[2,7,13]. It is also our impression that the majority of spontaneous GIH cases could be treated conservatively, and potentially risky and burdensome procedures such as total or subtotal gastrectomy could be significantly reduced.
Spontaneous gastric hematoma is a rare condition that can mimic other gastrointestinal emergencies. Clinicians must maintain a high level of suspicion when evaluating patients with acute abdominal pain, especially in the absence of trauma or known bleeding disorders. Early diagnosis through imaging and endoscopy along with tailored management strategies can lead to successful outcomes for patients with this rare and unusual condition. Further research is warranted to expand our understanding of the pathophysiology of GIH with the purpose of finding the most appropriate treatment.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: Croatia
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Qi XS, China; Shiryajev YN, Russia S-Editor: Qu XL L-Editor: A P-Editor: Qu XL
| 1. | Jones WR, Hardin WJ, Davis JT, Hardy JD. Intramural hematoma of the duodenum: a review of the literature and case report. Ann Surg. 1971;173:534-544. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 64] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 2. | Tabbikha O, Maalouf H, Abou-Malhab C, Aby Hadeer R, Wakim R. Spontaneous Gastric Intramural Hematoma: Case Report and Literature Review. Cureus. 2022;14:e23268. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 3. | Ng SN, Tan HJ, Keh CH. A belly of blood: A case report describing surgical intervention in a gastric intramural haematoma precipitated by therapeutic endoscopy in an anticoagulated patient. Int J Surg Case Rep. 2016;26:65-68. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 7] [Article Influence: 0.8] [Reference Citation Analysis (1)] |
| 4. | Alabd A, Deitch C. A Rare Case of Gastric Intramural Hematoma in Recurrent Leukemia. Cureus. 2022;14:e21385. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 5. | Mânzat Saplacan RM, Catinean A, Manole S, Valean SD, Chira RI, Mircea PA. Posttraumatic gastric wall hematoma in a patient under anticoagulant therapy. Case report and literature review. Med Ultrason. 2011;13:165-170. [PubMed] |
| 6. | Kim SJ, Lee JH, Park SM, Kwon KH. Conservative management of traumatic acute intramural hematoma of duodenal 2nd and 3rd portion: A case report and review of literature. Ann Hepatobiliary Pancreat Surg. 2020;24:109-113. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 7. | Spychała A, Nowaczyk P, Budnicka A, Antoniewicz E, Murawa D. Intramural gastric hematoma imitating a gastrointestinal stromal tumor - case report and literature review. Pol Przegl Chir. 2017;89:62-65. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 8] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 8. | Park CH, Kim EH, Jung DH, Chung H, Park JC, Shin SK, Lee YC, Kim H, Lee SK. Impact of periodic endoscopy on incidentally diagnosed gastric gastrointestinal stromal tumors: findings in surgically resected and confirmed lesions. Ann Surg Oncol. 2015;22:2933-2939. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 23] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 9. | McLauchlan J. Fatal false aneurysmal tumour occupying nearly the whole of the duodenum. Lancet. 1838;2:203-205. [DOI] [Full Text] |
| 10. | Hui J, AhChong AK, Mak KL, Chiu KM, Yip AW. Spontaneous intramural hematoma of stomach. Dig Surg. 2000;17:524-527. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 11. | Dhawan V, Mohamed A, Fedorak RN. Gastric intramural hematoma: a case report and literature review. Can J Gastroenterol. 2009;23:19-22. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 30] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 12. | Lee CC, Ravindranathan S, Choksi V, Pudussery Kattalan J, Shankar U, Kaplan S. Intraoperative Gastric Intramural Hematoma: A Rare Complication of Percutaneous Endoscopic Gastrostomy. Am J Case Rep. 2016;17:963-966. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 13] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 13. | Yoshioka Y, Yoshioka K, Ikeyama S. Large gastric intramural hematoma mimicking a visceral artery aneurysm: a case report. J Med Case Rep. 2018;12:61. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 6] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 14. | Intragumtornchai T, Israsena S, Benjacholamard V, Lerdlum S, Benjavongkulchai S. Esophageal tuberculosis presenting as intramural esophagogastric hematoma in a hemophiliac patient. J Clin Gastroenterol. 1992;14:152-156. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 3] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 15. | Molnár P, Mikó T. Multiple arterial caliber persistence resulting in hematomas and fatal rupture of the gastric wall. Am J Surg Pathol. 1982;6:83-86. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 25] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 16. | Hayashi T, Nagasue N, Chang YC, Kohno H, Nakamura T. Duodenal stenosis caused by ruptured aneurysms of the pancreaticoduodenal artery--a case report. Jpn J Surg. 1989;19:63-66. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 15] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 17. | Oe S, Watanabe T, Kume K, Shibata M, Hiura M, Yoshikawa I, Harada M. A case of idiopathic gastroesophageal submucosal hematoma and its disappearance observed by endoscopy. J UOEH. 2014;36:123-128. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 0.7] [Reference Citation Analysis (0)] |