Published online Dec 26, 2023. doi: 10.12998/wjcc.v11.i36.8519
Peer-review started: August 29, 2023
First decision: September 28, 2023
Revised: October 12, 2023
Accepted: December 7, 2023
Article in press: December 7, 2023
Published online: December 26, 2023
Processing time: 114 Days and 18.5 Hours
Cholecystoenteric fistula (CEF) involves the formation of a spontaneous ano
We present the case of a 57-year-old male with advanced gallbladder cancer (GBC) who arrived at the emergency room with persistent vomiting, abdominal pain, and diarrhea. An abdominopelvic computed tomography scan revealed a contracted gallbladder with bubbles in the fundus connected to the second por
The combination of imaging and surgery can enhance preoperative diagnosis and alleviate symptoms in patients with GBC complicated by CEF.
Core Tip: Cholecystoenteric fistulas are rarely associated with malignancy, and synchronous cholecystoduodenal and cholecystocolonic fistulas are even rarer. We present the case of a 57-year-old male with advanced gallbladder cancer complicated by synchronous cholecystoduodenal and cholecystocolonic fistulas. He presented with persistent vomiting, abdominal pain, and diarrhea. We also review 30 cases of gallbladder cancer-related cholecystoenteric fistulas published between 1973 and 2023. We performed a statistical analysis of clinical symptoms, imaging findings, and management. Our aim is to share our experience with diagnosis and surgical treatment of this condition and offer our insights to guide future clinical decision-making.
- Citation: Wang CY, Chiu SH, Chang WC, Ho MH, Chang PY. Cholecystoenteric fistula in a patient with advanced gallbladder cancer: A case report and review of literature. World J Clin Cases 2023; 11(36): 8519-8526
- URL: https://www.wjgnet.com/2307-8960/full/v11/i36/8519.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i36.8519
Gallbladder cancer (GBC) is a lethal disease typically diagnosed at an advanced stage, leading to a grim prognosis[1]. Cholecystoenteric fistula (CEF) is an uncommon complication of biliary disease that results from an abnormal connection between the gallbladder and the adjacent gastrointestinal tract. CEF occurs in only 3%-5% of patients with cholelithiasis and 0.15%-4.8% of those undergoing biliary surgery[2]. The most prevalent type of CEF is the cholecystoduodenal fistula (CDF), accounting for 70% of cases, followed by the cholecystocolonic fistula (CCF) at 20%[2,3]. CEF can be attributed to various factors, including cholelithiasis, peptic ulcer disease, and malignant neoplasms[2,4]. However, malignancy is associated with CEF in only 3%-14% of cases[5-8]. The coexistence of CDF and CCF is exceedingly rare, with reported incidences ranging from 1.5% to 5%[5,9-11].
We present the case of a 57-year-old male with advanced GBC complicated by synchronous CDF and CCF, who presented with persistent vomiting, abdominal pain, and watery diarrhea.
A 57-year-old Taiwanese male presented to our emergency department in November 2022 with a 3-d history of vomiting, abdominal pain, and watery diarrhea.
The patient reported experiencing postprandial vomiting, epigastric abdominal pain, and watery diarrhea more than 10 times daily for 3 d.
His past medical history was significant for gallstones, for which he received conservative treatment. In April 2022, he was diagnosed with poorly differentiated gallbladder adenocarcinoma, cT3N1M1, stage IVB, with liver metastases. He underwent 3 mo of palliative chemotherapy with cisplatin and gemcitabine. While the primary tumor exhibited a partial response, the hepatic tumor progressed. He subsequently underwent 3 mo of treatment with gemcitabine, high-dose 5-fluorouracil, and leucovorin.
The patient denied any family history of malignant tumors.
A physical examination revealed generalized abdominal tenderness but no Murphy’s sign or rebound abdominal tenderness. His body temperature was 36.0 ℃, blood pressure 130/90 mmHg, heart rate 103 beats per minute, and respiratory rate 18 breaths per minute.
Laboratory blood tests revealed a white blood cell count of 10990/L (normal range: 4500-11000), hemoglobin level of 8.0 g/dL (normal range: 13.5-18.0), platelet count of 466 x 103/µL (normal range: 150-400 × 103), creatinine level of 1.1 mg/dL (normal range: 0.7-1.2), aspartate aminotransferase 10 U/L (normal range: < 40), alanine aminotransferase 5 U/L (normal range: < 40), C-reactive protein 18.09 mg/dL (normal range: < 0.8), and lipase < 3 U/L (normal range: 11-82).
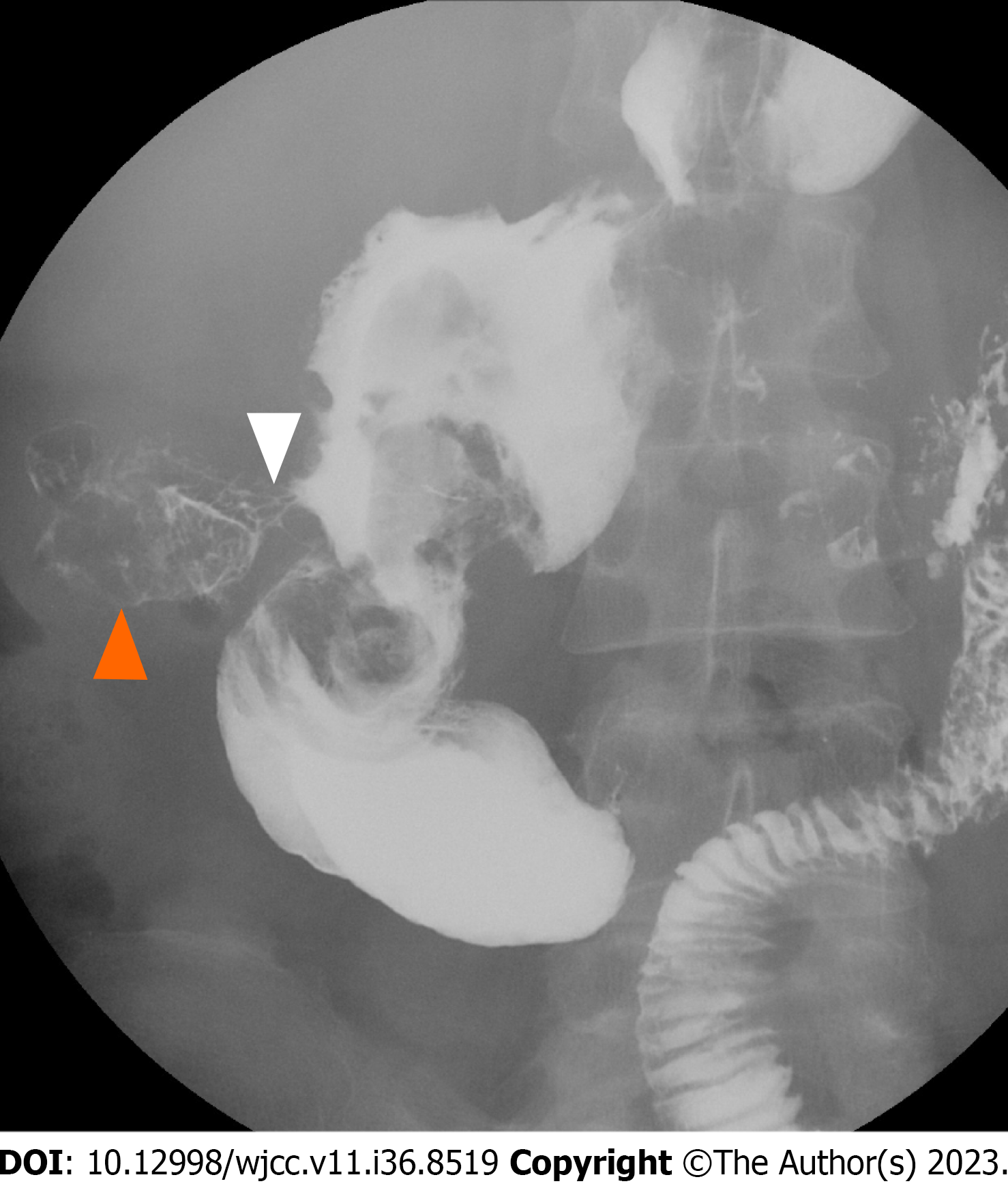
Abdominopelvic computed tomography (CT) displayed a gallstone in the gallbladder and a contracted gallbladder with bubbles in the fundus connected to the second portion of the duodenum and transverse colon (Figure 1). We suspected GBC invasion of the adjacent gastrointestinal tract through a CDF or a CCF. A subsequent esophagogastroduodenoscopy (EGD) and upper gastrointestinal (UGI) series identified a CDF in the second portion of the duodenum (Figure 2). A colo
Considering the patient’s medical history, we arrived at a final diagnosis of advanced GBC complicating synchronous CDF with CCF.
The patient was administered empiric antibiotic treatment for his intra-abdominal infection and parenteral nutrition. Nevertheless, the postprandial vomiting and watery diarrhea persisted, leading us to consider that his symptoms were the result of the synchronous CDF and CCF. We referred the patient to a general surgeon for palliative surgery to improve his quality of life. During the exploratory laparotomy, we identified GBC with invasion of the duodenum and transverse colon, resulting in CDF and CCF. Furthermore, severe adhesions over the second portion of the duodenum and hepatic flexure of the colon posed challenges for fistulectomy, fistula closure, and stent placement. As a result, we performed a Roux-en-Y gastrojejunostomy and loop ileostomy.
Following surgery, his symptoms improved, and he resumed oral intake. On day 50, he was discharged and commenced oral targeted therapy with lenvatinib for ongoing anticancer treatment.
While most CEFs arise as late complications of gallstone disease, they can also develop when GBC invades the adjacent gastrointestinal tract, as reported in several studies (Table 1). Adenocarcinoma is the predominant cancer type (68.7%). The incidence of CCF is similar to CDF, with rates of 45.2% and 38.7%, respectively. Synchronous CCF and CDF occur in 12.9% of all patients, typically within the hepatic flexure (72.2%) and transverse colon (28.8%). Gallstones and recurrent gallbladder inflammation preceding GBC invasion may contribute to CEF development[12]. Direct GBC invasion into the duodenal and colonic walls likely contributed to our case’s fistula formation.
| Ref. | Sex/age(yr) | Clinical symptoms | Image modalities and findings | Type of GBC | Type of CEF | Management |
| [4] | M/68 | Abdomen pain, anorexia, weight loss | CT, colonoscopy: GBC, HF colon fistula | Adenocarcinoma | CCF | Diverting loop ileostomy |
| [15] | F/64 | Right abdomen pain, weight loss, fever, jaundice | CT: GBC, HF colon fistula | Carcinoma | CCF | Palliative treatment |
| [16] | F/78 | Nausea, vomiting | EGD, CT: GBC, duodenal fistula | Adenocarcinoma | CDF | Cholecystectomy, left hepatic lobectomy, antrectomy, resection of first portion of duodenum, reconstruction with a Roux-en-Y gastrojejunostomy |
| [17] | F/81 | Right upper abdomen pain, anorexia, fever | EGD, CT, MRI, gastrografin: GBC, duodenal fistula, HF colon fistula | SqCC | CDF, CCF | EGD and colonoscopy with endoscopic fistula closure |
| [18] | F/59 | Nausea, vomiting | CT, ERCP: GBC, duodenal fistula | Adenocarcinoma | CDF | Endobiliary RFA with stents placement |
| [19] | F/80 | Right upper abdomen pain | CT: Transverse colon fistula | SqCC | CCF | Cholecystectomy, partial colectomy |
| [20] | M/68 | Right upper abdomen pain, weight loss | CT: Duodenal fistula | SqCC | CDF | Palliative chemotherapy, targeted therapy, and radiotherapy |
| [21] | M/68 | None | PET CT, MRI, EGD: porcelain gallbladder, suspected GBC, duodenal fistula | Adenocarcinoma | CDF | Subtotal stomach-preserving pancreatoduodenectomy, radical cholecystectomy |
| [22] | M/59 | Abdomen pain, vomiting | CT: HF colon fistula, a gallstone in the left colon | Carcinoma | CCF | Colostomy |
| [23] | M/74 | Right upper abdomen pain, weight loss | CT: Duodenal fistula | Adenocarcinoma | CDF | Unknown |
| [24] | F/67 | Upper abdomen pain, nausea, diarrhea, weight loss | CT: GBC | SGCC | CCF | Cholecystectomy, bisegmentectomy IVb-V, right hemicolectomy |
| [25] | M/87 | Abdomen pain | CT: Transverse colon fistula | Carcinosarcoma | CCF | Cholecystectomy with partial transverse colectomy |
| [6] | F/62 | None | CT: Gallstone, suspected HF colon cancer | Adenocarcinoma | CCF | Cholecystectomy, right hemicolectomy |
| [26] | F/81 | Upper abdomen pain, fever | PTC: GBC, transverse colon fistula | Papillomatosis | CCF | Cholecystectomy, fistula closure, choledocholithotomy with T-tube drainage |
| [27] | M/66 | Right upper abdomen pain, nausea, vomiting | CT, EGD: Duodenal fistula | SqCC | CDF | Palliative treatment |
| [28] | F/48 | Right upper abdomen pain, jaundice, melena | US, CT: GBC, HF colon fistula | Adenocarcinoma | CCF | Chemotherapy, radiotherapy |
| [29] | F/81 | Upper abdomen pain, vomiting | CT: Duodenal fistula | Adenocarcinoma | CDF | Cholecystectomy, fistula closure, gastrojejunostomy, choledochojejunostomy |
| [30] | F/75 | Abdomen pain, vomiting, diarrhea | CT: Air-filled thickened-walled gallbladder | Adenocarcinoma | Unknow | Laparotomy with stone extraction, palliative treatment |
| [31] | F/80 | Anorexia | EGD: Duodenal fistula | Adenocarcinoma | CDF | Cholecystectomy, fistula closure, choledocholithotomy with T-tube drainage |
| [32] | F/46 | Right upper abdomen pain, weight loss | US, CT: GBC, gallstone | Adenocarcinoma | CCF | Cholecystectomy with partial hepatic segments resection (IV and V), fistulectomy, right hemicolectomy |
| [33] | F/76 | Right upper abdomen pain, vomiting | CT: Air-filled thickened-walled gallbladder, duodenal fistula | Carcinoma | CDF | Enterotomy with stone extraction |
| [34] | M/84 | Coffee ground emesis | EGD, CT: Gallstone, duodenal fistula | Adenocarcinoma | CDF | Cholecystectomy, duodenum repair |
| [35] | F/60 | Right upper abdomen pain, fever, nausea, vomiting | US, PTC, MRI: GBC, gallstone, HF colon fistula | Adenocarcinoma | CCF | Laparotomy, right hemicolectomy, primary anastomosis |
| [36] | F/67 | Right upper abdomen pain, anorexia | CT, gastrografin: Gastric fistula | Adenocarcinoma | CGF | Cholecystectomy, liver wedge resection, and gastric antrectomy including the fistula, gastroduodenal anastomosis |
| [37] | F/70 | Abdomen pain, nausea, vomiting, weight loss | US, gastrografin: HF colon fistula | SqCC | CCF | Extended right hemicolectomy, subtotal excision of the gallbladder |
| [38] | F/72 | Upper abdomen pain, nausea, vomiting | Gastrografin, EGD: Gallstone in duodenum | Metastatic breast carcinoma | CDF | Laparotomy with stone extraction |
| [39] | F/75 | Abdomen pain, nausea, diarrhea, weight loss | US, gastrografin, EGD: Gallstone, gastric outlet obstruction | Adenocarcinoma | CDF | Enterostomy with stone extraction, cholecystectomy with fistula excision |
| [40] | M/55 | Right upper abdomen pain, diarrhea, weight loss | Gastrografin, colonoscopy, EGD: duodenal fistula, transverse colon fistula | Adenocarcinoma | CDF, CCF | Radical cholecystectomy, partial gastrectomy, vagotomy, duodenectomy, proximal pancreatectomy, right hemicolectomy, resection of the proximal jejunum, anticolic antiperistaltic gastrojejunostomy (Polya), end-to-side choledochojejunostomy, ileotransverse colostomy |
| [41] | F/51 | Right upper abdomen pain, fever, vomiting | Gastrografin: Leakage from the duodenum | Adenocarcinoma | CDF, CCF | Diagnostic laparotomy, palliative treatment |
| [41] | M/63 | Right upper abdomen pain, melena | None | Adenocarcinoma | CCF | Palliative treatment |
| Our case | M/57 | Abdomen pain, vomiting, diarrhea | CT, EGD, colonoscopy, gastrografin, MRCP: GBC, gallstone, duodenal fistula, transverse colon fistula | Adenocarcinoma | CDF, CCF | Roux-en-Y gastrojejunostomy, loop ileostomy |
The primary clinical manifestations of CEF include abdominal pain (typically in the right upper quadrant), nausea, vomiting, weight loss, and diarrhea[2,5]. Our review of the literature found that the most common symptoms of GBC-related CDF are abdominal pain (68.8%), nausea or vomiting (62.5%), and weight loss (25%). These symptoms resemble GBC-related CCF (abdominal pain: 88.9%, nausea or vomiting: 33.3%, and weight loss: 33.3%). Only 16.7% of patients with GBC-related CCF experience diarrhea. Due to its nonspecific symptoms, signs, and laboratory investigations, pre
Conventional surgery for CEF involves cholecystectomy and fistula closure, performed as an open or laparoscopic procedure based on the surgeon’s experience and the patient’s condition[2,5,9,11,13]. However, few cases are suitable for resection, and palliative chemotherapy with gemcitabine and cisplatin is the current standard of care for patients with advanced-stage GBC[1,14]. Therefore, surgical closure of fistulas, stent placement therapy, and bypass surgery may be considered. Our patient underwent an exploratory laparotomy for palliative purposes. Further palliative treatment, such as chemotherapy, radiation therapy, or targeted therapy, is indicated. Due to the failure of previous standard chemo
Clinicians should consider CEF in patients with GBC who present with persistent vomiting or diarrhea. Use of multiple imaging modalities can increase the likelihood of detecting CEF before surgery. Despite its grim prognosis and 5-year survival rate of < 5%, surgery remains a viable option for alleviating GBC symptoms and enhancing quality of life.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Oncology
Country/Territory of origin: Taiwan
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Kai K, Japan; Shariati MBH, Iran; Wani I, India S-Editor: Yan JP L-Editor: A P-Editor: Yan JP
| 1. | Roa JC, García P, Kapoor VK, Maithel SK, Javle M, Koshiol J. Gallbladder cancer. Nat Rev Dis Primers. 2022;8:69. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 220] [Cited by in RCA: 178] [Article Influence: 59.3] [Reference Citation Analysis (0)] |
| 2. | Gonzalez-Urquijo M, Rodarte-Shade M, Lozano-Balderas G, Gil-Galindo G. Cholecystoenteric fistula with and without gallstone ileus: A case series. Hepatobiliary Pancreat Dis Int. 2020;19:36-40. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 16] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 3. | Choi C, Osman K, Hartley CP, Maselli DB. Cholecystocolonic fistula as an uncommon cause of diarrhea: a case-report and review of the literature. Clin J Gastroenterol. 2021;14:1147-1151. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 4. | Ojemolon PE, Kwei-Nsoro R, Haque M, Shah MP, Pinnam B, Almoghrabi A. Different Approaches to the Management of Cholecystoenteric Fistula. ACG Case Rep J. 2023;10:e00960. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 5. | Huang SF, Han YH, Chen J, Zhang J, Huang H. Surgical Management of Cholecystoenteric Fistula in Patients With and Without Gallstone Ileus: An Experience of 29 Cases. Front Surg. 2022;9:950292. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 6. | Ha GW, Lee MR, Kim JH. Cholecystocolic fistula caused by gallbladder carcinoma: preoperatively misdiagnosed as hepatic colon carcinoma. World J Gastroenterol. 2015;21:4765-4769. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 11] [Cited by in RCA: 11] [Article Influence: 1.1] [Reference Citation Analysis (2)] |
| 7. | Inal M, Oguz M, Aksungur E, Soyupak S, Börüban S, Akgül E. Biliary-enteric fistulas: report of five cases and review of the literature. Eur Radiol. 1999;9:1145-1151. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 34] [Article Influence: 1.3] [Reference Citation Analysis (1)] |
| 8. | Yamashita H, Chijiiwa K, Ogawa Y, Kuroki S, Tanaka M. The internal biliary fistula--reappraisal of incidence, type, diagnosis and management of 33 consecutive cases. HPB Surg. 1997;10:143-147. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 60] [Cited by in RCA: 62] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 9. | Li XY, Zhao X, Zheng P, Kao XM, Xiang XS, Ji W. Laparoscopic management of cholecystoenteric fistula: A single-center experience. J Int Med Res. 2017;45:1090-1097. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 28] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 10. | Clavien PA, Richon J, Burgan S, Rohner A. Gallstone ileus. Br J Surg. 1990;77:737-742. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 245] [Cited by in RCA: 247] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 11. | Chowbey PK, Bandyopadhyay SK, Sharma A, Khullar R, Soni V, Baijal M. Laparoscopic management of cholecystoenteric fistulas. J Laparoendosc Adv Surg Tech A. 2006;16:467-472. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 84] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 12. | Bochus HL. Gastroenterology. 2nd ed. vol. 3. Philadelphia: Saunders, 1966: 852. |
| 13. | Crespi M, Montecamozzo G, Foschi D. Diagnosis and Treatment of Biliary Fistulas in the Laparoscopic Era. Gastroenterol Res Pract. 2016;2016:6293538. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 22] [Cited by in RCA: 33] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 14. | Sturm N, Schuhbaur JS, Hüttner F, Perkhofer L, Ettrich TJ. Gallbladder Cancer: Current Multimodality Treatment Concepts and Future Directions. Cancers (Basel). 2022;14. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 20] [Cited by in RCA: 28] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 15. | Gasque RA, Mollard L, Cervantes JG, Lenz Virreira ME, Quiñonez EG, Mattera FJ. [Cholecystocolonic fistula as a complication of advanced gallbladder cancer]. Rev Fac Cien Med Univ Nac Cordoba. 2022;79:301-303. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 16. | Shelton J, McCall M, Strickland M. A216 When cancer casts the first stone: a case report of gallbladder cancer presenting as gallstone ileus. J Can Assoc Gastroenterol. 2022;5:104-106. [RCA] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 17. | Sato S, Chinda D, Tanaka Y, Kaizuka N, Higuchi N, Ota S, Miyazawa K, Kikuchi H, Aizawa S, Iwamura H, Fukuda S. Effective Endoscopic Closure of Cholecysto-duodenal and Transverse Colon Fistulas Due to Squamous Cell Carcinoma of the Gallbladder Using Polyglycolic Acid Sheets and a Covered Metal Stent. Intern Med. 2021;60:1723-1729. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 18. | Vanek P, Freeman ML, Trikudanathan G. Complex endoscopic management of gallbladder cancer patient with Bouveret syndrome. VideoGIE. 2021;6:16-18. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 19. | Sunakawa T, Ko K, Moriyasu R, Nishida Y, Otagiri N, Tauchi K. Emergency surgery for acute cholecystitis associated with cholecystocolonic fistula caused by gallbladder cancer: a case report. J Surg Case Rep. 2020;2020:rjaa305. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 20. | Reith TP, Nair V, McKenna EJ, Singavi A. Metastatic Squamous Cell Carcinoma in the Gallbladder Fossa Complicated by a Duodenal Fistula. Cureus. 2019;11:e6522. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 21. | Matsumoto Y, Fujimoto K, Mitsuoka E, Senda E, Shio S, Ichikawa K, Yamada H. Cholecystoduodenal fistula caused by aggressive mucinous gallbladder carcinoma with a porcelain gallbladder. Clin J Gastroenterol. 2019;12:460-465. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 22. | Brieau B, Barret M, Leblanc S, Oudjit A, Coriat R. A rolling stone plugging the colon: Consequence of a cholecystocolonic fistula from gallbladder cancer. Presse Med. 2017;46:784-785. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 23. | Khosla MS, Nadir A, Ravi J, Chuang KY. Invasive Gallbladder Cancer With a Cholecystoduodenal Fistula Allowing Direct Gallbladder Biopsy Through EGD. Am J Gastroenterol. 2016;111:1228. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 24. | Garcia Amador C, Ramia JM, Alonso J, de la Plaza R, Lopez-Marcano A, Gonzales JD, Valenzuela JC, Medina A. Gallbladder spindle and giant cell type undifferentiated carcinoma and cholecysto-colonic fistula. HPB. 2016;18:e478. [DOI] [Full Text] |
| 25. | Tonouchi A, Yokoyama N, Hashidate H, Matsuzawa N, Katayanagi N, Otani T. Education and Imaging. Gastroenterology: Carcinosarcoma of the gallbladder presenting as a cholecysto-colic fistula. J Gastroenterol Hepatol. 2015;30:1112. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 26. | Kuo JY, Jao YT. Gallbladder papillomatosis and cholecystocolonic fistula: a rare combination. Am J Case Rep. 2014;15:466-470. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 27. | Malhotra N, Sultan M, Mattar M. Gallbladder Cancer Eroding Into the Duodenum Causing Gastric Outlet Obstruction: 2168. Am J Gastroenterol. 2014;109:S628. [DOI] [Full Text] |
| 28. | Dwivedi AN, Kumar S, Rana S, Maurya B. Transmural invasion of hepatic flexure of colon causing cholecystocolic fistula by aggressive gallbladder carcinoma. World J Surg Oncol. 2013;11:86. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 29. | Shinoda M, Aiura K, Yamagishi Y, Masugi Y, Takano K, Maruyama S, Irino T, Takabayashi K, Hoshino Y, Nishiya S, Hibi T, Kawachi S, Tanabe M, Ueda M, Sakamoto M, Kitagawa Y. Bouveret's syndrome with a concomitant incidental T1 gallbladder cancer. Clin J Gastroenterol. 2010;3:248-253. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 30. | Heemskerk J, Nienhuijs SW. Gallstone ileus as first presentation of a gallbladder carcinoma. J Gastrointestin Liver Dis. 2009;18:253-254. [PubMed] |
| 31. | Yachida S, Tsutsui K, Suzuki Y. Minute gallbladder carcinoma associated with an anastomotic cholecystoduodenal fistula. Clin Gastroenterol Hepatol. 2009;7:e6-e7. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 32. | Rastogi R. Cholecystocolic fistula secondary to gallbladder carcinoma: a rare case. Saudi J Gastroenterol. 2008;14:144-146. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 33. | Zissin R, Osadchy A, Klein E, Konikoff F. Consecutive instances of gallstone ileus due to obstruction first at the ileum and then at the duodenum complicating a gallbladder carcinoma: a case report. Emerg Radiol. 2006;12:108-110. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 34. | Chorost MI, Huang IP, Webb H, Abir F, Ghosh BC. Incidental gallbladder carcinoma associated with a cholecystoduodenal fistula. Mil Med. 2002;167:862-863. [PubMed] |
| 35. | Ramos-De la Medina A, Medina-Franco H. [Biliary-colonic fistulas. Analysis of 2 cases and literature review]. Rev Gastroenterol Mex. 2002;67:207-209. [PubMed] |
| 36. | Lein HH, Tai FC, Huang CS, Chen KM, Lee CL. Xanthogranulomatous Cholecystitis Combined with Gall Bladder Cancer and Cholecystogastric Fistula-A Case Report. Formosan J of Surg. 1999;32:191-195. |
| 37. | Khaira HS, Awad RW, Thompson AK. Squamous cell carcinoma of the gallbladder presenting with a biliary-colic fistula. Eur J Surg Oncol. 1995;21:581-582. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 17] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 38. | Panov TA, Kiossev KT, Losanoff JE. Bouveret's syndrome: a rare consequence of malignant cholecystoduodenal fistula. Mil Med. 1994;159:755-757. [PubMed] |
| 39. | Singer M, Chandar VP, Hookman P. Gallbladder carcinoma with gastric outlet obstruction and gallstone ileus. South Med J. 1986;79:902-903. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.0] [Reference Citation Analysis (0)] |
| 40. | Morris SJ, Greenwald RA, Barkin JS, Tedesco FJ, Snyder R. Cholecystoduodenocolic fistula secondary to carcinoma of the gallbladder. Am J Dig Dis. 1978;23:849-852. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 41. | Shah M, Mori W. A clinico-pathological study of spontaneous internal biliary fistula. Acta Pathol Jpn. 1973;23:349-358. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |