Published online Dec 26, 2023. doi: 10.12998/wjcc.v11.i36.8507
Peer-review started: August 20, 2023
First decision: November 1, 2023
Revised: November 14, 2023
Accepted: December 12, 2023
Article in press: December 12, 2023
Published online: December 26, 2023
Processing time: 123 Days and 22.9 Hours
Spinal infection with sparganosis is rarely seen, and multiple spinal infections with sparganosis in the thoracic spine have not been reported.
In this case report, a 56-year old male patient suffered from back pain for 3 mo. Computed tomography examination of the thoracic spine showed bone destruction of the T4-5 vertebral body, as well as the right pedicle and lamina of T5. Magnetic resonance imaging showed high signals on T2W1 images and fat-suppressed images in the right vertebral body of T4-5 and the right pedicle and lamina of T5, a high signal in the vertebral canal, and similar high signals in the paravertebral and subcutaneous regions of the whole spine. Puncture biopsy showed sparganosis. Following definite diagnosis, the patient was treated with debridement of T4-5 infected lesions under a microscope, bone grafting and internal fixation. Postoperatively, the patient's back pain symptoms were significantly relieved; the incision healed after one-stage treatment, and alben
Puncture biopsy is the most reliable method to diagnose infection by sparganum. Removal of infected lesions under the microscope and albendazole for anti
Core Tip: Spinal infection with sparganosis is rarely seen, and multiple spinal infections with sparganosis in the thoracic spine have not been reported.
- Citation: Wen GJ, Chen J, Zhang SF, Zhou ZS, Jiao GL. Multiple sparganosis spinal infections mainly in the thoracic region: A case report. World J Clin Cases 2023; 11(36): 8507-8511
- URL: https://www.wjgnet.com/2307-8960/full/v11/i36/8507.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i36.8507
Infection due to sparganum was first reported by Cobbola[1] in 1883. Sparganum is a rare parasite, which can be found anywhere in the body, including the central nervous system. In spinal sparganosis, cervical vertebra, thoracic vertebra and lumbosacral vertebra have been reported[2-7], and sparganosis in the spinal canal, epidural, subdural and intramedullary regions have also been reported[8]. However, multiple spinal infections with sparganosis in the thoracic spine, spinal canal, vertebral body and paravertebral region have not been reported.
A 56-year-old male patient suffered from back pain for 3 mo.
No special notes.
No special notes.
The patient had a habit of eating raw beef, raw mutton and raw snake meat in the past.
Physical examination showed no obvious neurological damage.
Laboratory examination results were as follows: Leukocytes and neutrophils were not significantly increased, and no obvious abnormalities in tumor markers were found.
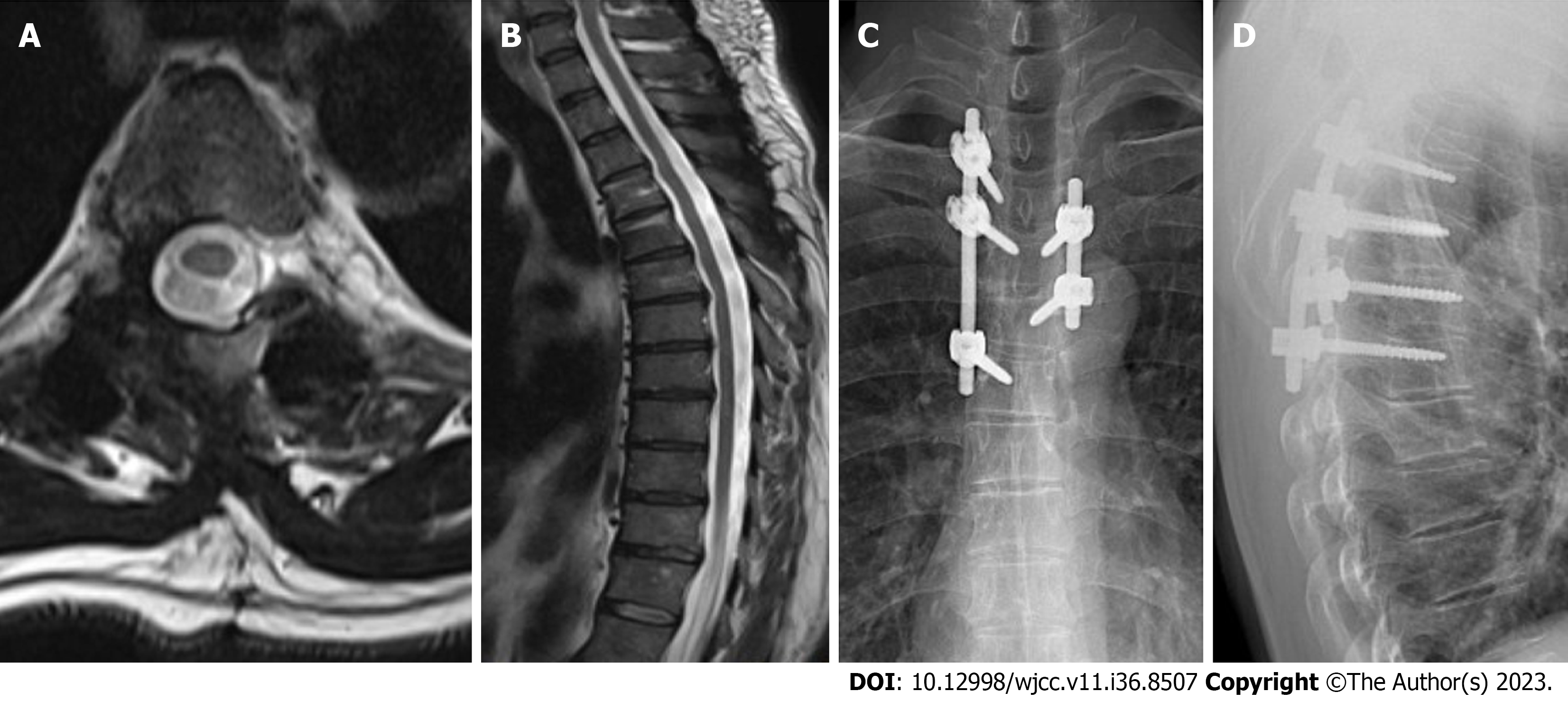
Computed tomography examination showed that bone of the T4-5 vertebral body was damaged; the right pedicle and lamina of T5 were also damaged (Figure 1A and B). Cervical, thoracic and lumbar magnetic resonance imaging (MRI) showed high signals on T2W1 images and fat-suppressed images in the right vertebral body of T4-5 and the right pedicle and lamina of T5, high signals in the vertebral canal, with similar high signals in the paravertebral and subcutaneous regions of the whole spine (Figure 1C-G).
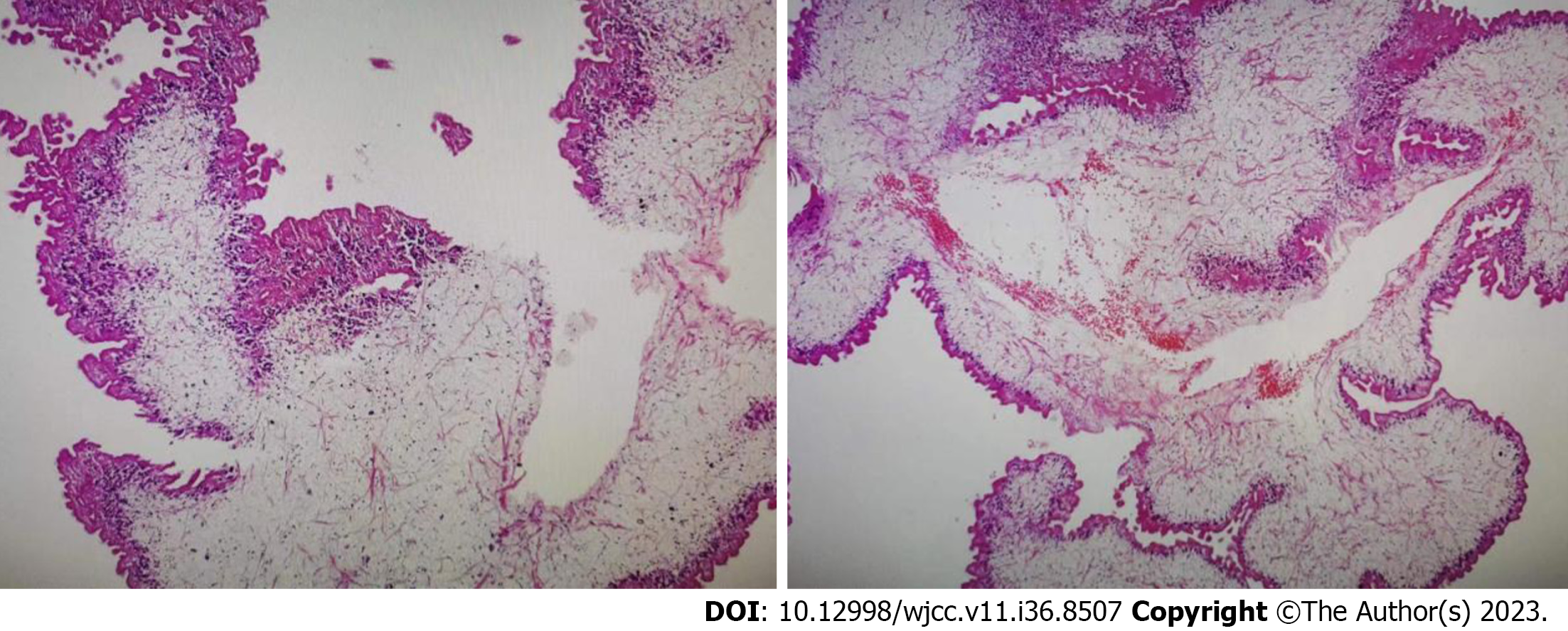
The biopsy results showed that parasites were found in the punctured lesions, which was consistent with sparganosis (Figure 2).
The patient was treated with debridement of T4-5 infected lesions, bone grafting and internal fixation. Postoperatively, the patient was treated with albendazole for 3 mo (Video).
Following surgery, the patient's back pain symptoms were significantly relieved, and there was no neurological damage. The incision healed after one-stage treatment. One week after surgery, the patient could walk normally with a brace. Nine months after surgery, the patient had no obvious back pain, MRI showed significant absorption of the lesions, and the anteroposterior and lateral radiographs suggested that local curvature and the screw positions were satisfactory (Figure 3).
Spinal sparganosis is a very rare disease. In particular, thoracic spine sparganosis with multiple infections in the spinal region has not been reported. For the diagnosis of sparganosis, anti-sparganum antibodies in serum or cerebrospinal fluid can be detected by enzyme-linked immunosorbent assay (ELISA). The sensitivity of this diagnostic technique can reach 85.7%-100%, and the specificity can reach 95.7%[9]. In 2014, Yamasaki et al[10] proposed a new detection technology for sparganosis, the iSpaICT kit, which is faster and easier than ELISA, with better sensitivity and specificity. Sparganosis is extremely rare, and laboratory testing is not routinely carried out in most Chinese hospitals. In the present patient, MRI of the spine showed a cystic lesion located in T4-5 compressing the spinal cord, many minor mass-like lesions were located in the paravertebral and subcutaneous regions of the spine, and the MRI features were very similar to literature reports[3,11]. Puncture biopsy is the most effective and reliable method for diagnosing sparganosis. However, for sparganosis in the vertebral canal, subdural region, spinal cord or brain, puncture biopsy is very risky, and sometimes cannot be performed. Accordingly, these cases require to be confirmed by laboratory examinations or after focal resection. Our patient underwent a puncture biopsy on the third day after admission, and the lesion was easily visualized under fluoroscopy. The biopsy sample was submitted for examination and culture, but no bacteria were cultured. Parasites were seen under the microscope, and a small quantity of calcareous corpuscles was seen below them, which conformed to the shape of sparganosis. Broken striated muscle tissue and dead bone tissue were also seen, in addition to an inflammatory reaction. When the pathological diagnosis was confirmed, the patient was asked about his past history. The patient had a habit of eating raw beef, raw mutton and raw snake meat.
Following the diagnosis of sparganosis, posterior thoracic 4-5 lesion removal, bone grafting and internal fixation were performed. Compared with tumor resection, the removal of sparganosis lesions is less difficult. There is no need to embolize the blood vessels before surgery, and bleeding during surgery is easily controlled. During surgery, neuroelectrophysiological monitoring was used and the infected lesion was removed under the microscope, which enhanced the safety of surgery and ensured the thoroughness of lesion removal. After thorough removal of the dead bone and the lesion in the vertebral body, bone grafting was performed using the posterior resected vertebral lamina and small articular processes as the bone graft materials. Due to instability in this region, we implanted the pedicle rod system for internal fixation. The pedicle in the right side of the T5 was damaged. The left sides of T4 and T5 were fixed, and the right sides of T3-6 were fixed.
Postoperatively, antiparasitic treatment was considered very important, and the drug of choice in the literature[3,12] for sparganosis is praziquantel. However, the patient experienced dizziness, chest tightness, nausea and vomiting after taking praziquantel, and switched to albendazole for 3 mo. Nine months after surgery, the patient had no obvious back pain, and MRI showed significant absorption of the lesions. Thus, treatment was considered safe and effective.
Spinal infection with sparganosis is a rare event. We report an uncommon case of thoracic spine sparganosis with multiple sites of infection. Puncture biopsy is the most effective and reliable method for diagnosing sparganosis. Removal of infected lesions under a microscope and albendazole antiparasitic treatment was safe and effective (Video).
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Infectious diseases
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): E
P-Reviewer: Chhabra HS, India; Viswanathan VK, United States S-Editor: Liu JH L-Editor: Webster JR P-Editor: Zhang YL
| 1. | Cobbola TS. Description of ligulamansoni, a new human cestode. J Lin Soc Lond. 1883;17:78-83. [RCA] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 2. | Jang SY, Kim CH. Migration of sparganosis from the brain to the cervical spinal cord. J Korean Neurosurg Soc. 2012;51:170-172. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 3. | Bao XY, Ding XH, Lu YC. Sparganosis presenting as radiculalgia at the conus medullaris. Clin Neurol Neurosurg. 2008;110:843-846. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 4. | Park JH, Park YS, Kim JS, Roh SW. Sparganosis in the lumbar spine: report of two cases and review of the literature. J Korean Neurosurg Soc. 2011;49:241-244. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 5. | Chotmongkol V, Phuttharak W, Jingjit K, Chaisuriya N, Sanpool O, Chaichan S, Khamsai S. Case Report: Sparganosis of the Cauda Equina. Am J Trop Med Hyg. 2021;104:298-302. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 6. | Fan JF, Huang S, Li J, Peng RJ, Huang H, Ding XP, Jiang LP, Xi J. A Human Case of Lumbosacral Canal Sparganosis in China. Korean J Parasitol. 2021;59:635-638. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 7. | Boonyasiri A, Cheunsuchon P, Srirabheebhat P, Yamasaki H, Maleewong W, Intapan PM. Sparganosis presenting as cauda equina syndrome with molecular identification of the parasite in tissue sections. Korean J Parasitol. 2013;51:739-742. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 12] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 8. | Cho YD, Huh JD, Hwang YS, Kim HK. Sparganosis in the spinal canal with partial block: an uncommon infection. Neuroradiology. 1992;34:241-244. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 11] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 9. | Kim H, Kim SI, Cho SY. Serological Diagnosis Of Human Sparganosis By Means Of Micro-ELISA. Kisaengchunghak Chapchi. 1984;22:222-228. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 67] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 10. | Yamasaki H, Nakamura T, Intapan PM, Maleewong W, Morishima Y, Sugiyama H, Matsuoka H, Kobayashi K, Takayama K, Kobayashi Y. Development of a rapid diagnostic kit that uses an immunochromatographic device to detect antibodies in human sparganosis. Clin Vaccine Immunol. 2014;21:1360-1363. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 14] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 11. | Huang X, Jia C, Zhan Y, Fu S, Zhang H. Subcutaneous sparganosis: a case report and literature review. Int J Dermatol. 2023;62:1067-1069. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 12. | Meng Y, Wan W, Xiong ZC, Wu P, Zhang N, Yu YQ, Huang SH, Liu ZL, Liu JM. Sparganosis of a thoracic vertebra misdiagnosed as bone metastasis from lung cancer. Int J Infect Dis. 2023;135:67-69. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |