Published online Dec 26, 2023. doi: 10.12998/wjcc.v11.i36.8486
Peer-review started: October 18, 2023
First decision: November 2, 2023
Revised: November 23, 2023
Accepted: December 12, 2023
Article in press: December 12, 2023
Published online: December 26, 2023
Processing time: 65 Days and 4.1 Hours
Critical time intervention (CTI) is an evidence-based model of practice that is time-limited and aims to provide support for most susceptible individuals during a transition period.
To examine the significance of fostering the mental health of diabetes patients through CTI using the scoping review methodology.
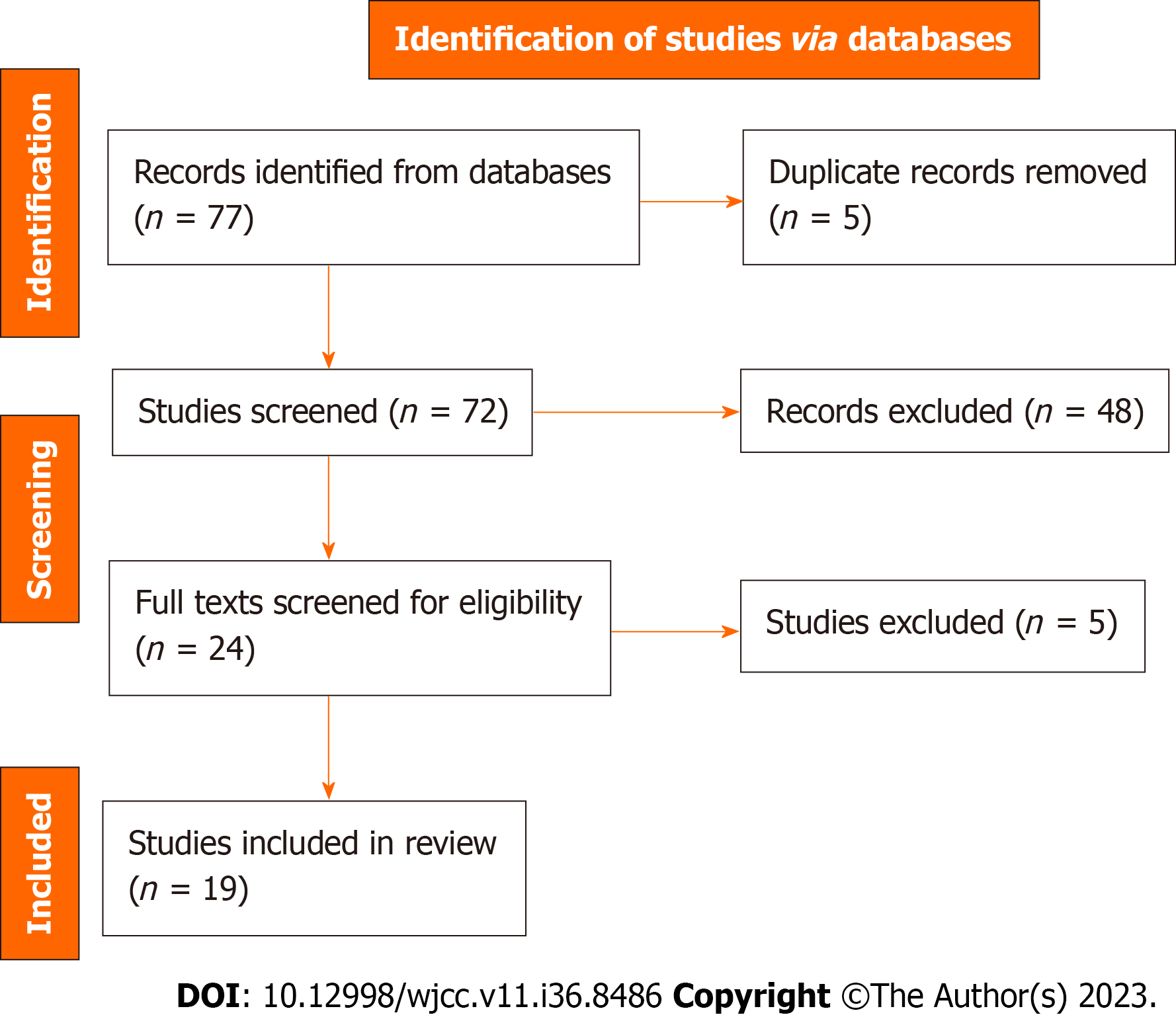
As part of the scoping review process, we followed the guidelines established by the Joanna Briggs Institute. The search databases were Google Scholar, PubMed, Scopus, PsycINFO, Reference Citation Analysis (https://www.referencecitationanalysis.com/), and Cochrane Library. From these databases, 77 articles were retrieved with the aid of carefully selected search terms. However, 19 studies were selected after two reviewers appraised the full texts to ensure that they are all eligible for inclusion, while 54 papers were excluded.
This study revealed that diabetic patients who had experienced homelessness were at higher risk of being diagnosed with mental illness and that social support services are impactful in the management of the comorbidity of diabetes and mental health problems. In addition, this review reveals that CTI is impactful in enhancing the mental health of homeless patients during the transitional period from the hospital through social support services.
CTI is a promising intervention for alleviating mental health symptoms in homeless patients. Empirical studies are needed across the globe, involving both hospitalized and community-based patients, to determine how clinically effectively CTI is in managing the mental health of diabetics.
Core Tip: Evidence suggests that diabetic patients who have experienced homelessness are at higher risk of being diagnosed with mental illness, and that social support services are impactful in the management of the comorbidity of diabetes and mental health problems. Studies on the effectiveness of critical time intervention (CTI) among patients with diabetes are limited. Available studies have shown that CTI is a promising intervention for alleviating mental health symptoms in homeless patients.
- Citation: Eseadi C, Amedu AN, Aloh HE. Significance of fostering the mental health of patients with diabetes through critical time intervention. World J Clin Cases 2023; 11(36): 8486-8497
- URL: https://www.wjgnet.com/2307-8960/full/v11/i36/8486.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i36.8486
Diabetes can cause other health problems and complications, both physically and psychologically. Diabetes is a chronic disorder of metabolism that has become a major health concern worldwide. It is characterized by absolute deficits in insulin secretion; chronic hyperglycemia; and abnormal carbohydrate, lipid, and protein metabolism[1]. Glucose levels in the blood are elevated in people with diabetes[2]. In the literature, diabetes has been classified into four types: Type 1 diabetes (T1D), type 2 diabetes (T2D), gestational diabetes (GD), and other diabetes associated with certain specific conditions such as pathologies or disorder[3,4]. TID is insulin-dependent diabetes, which constitutes 5%-10% of all diabetic cases. T1D is an autoimmune disorder distinguished by T cell-mediated degeneration of pancreatic β cells, ultimately resulting in insulin depletion and hyperglycemia[5]. The pathogenesis of T1D is influenced by both genetic and environmental factors, and the pancreatic β cell-specific autoimmunity development rate is rapid in infants and children. T2D is non-insulin-dependent diabetes that constitutes about 90%–95% of diabetes cases. The characteristics of T2D are abnormalities in insulin secretion, β cell dysfunction, and insulin resistance[6]. T2D is often undiagnosed because it progresses very slowly asymptomatically over the years until the appearance of classic symptoms connected with severe hyperglycemia such as weight loss, growth impairment, polyuria, and polydipsia at the advanced stage. The pathogenesis of T2D is complex and involves multiple unknown and known features such as a combination of genetic predisposition and strong environmental influences. T2D is prevalent in older adults and is linked to obesity, inactivity, adoption of modern lifestyles, and a family history of diabetes[3]. GD is a type of diabetes linked to pregnancy, which is diagnosed between the second and third trimesters excluding undetected T2D. GD is characterized by an increase in blood glucose levels in the third trimester of pregnancy. Ninety percent of diabetes and its complications in such a period are attributed to GD, with a prevalence varying from 1% to 14%[7]. The risk of GD is linked to older age, previous pregnancy with a large baby, obesity, and a history of impaired glucose tolerance and is associated with a high lifetime risk of developing T2D[3]. Other types of diabetes associated with peculiar conditions such as pathologies or many disorders are those stemming from monogenic defects in β cell function, genetic abnormalities in insulin action, and exocrine pancreatic pathologies, among other conditions[8].
Diabetic patients may feel insecure in terms of their mental health. As a result, they monitor their blood glucose excessively, worry about complications, and constantly monitor their personal and work lives. When diabetes and mental illness coexist, the prognosis is often poor[9]. Complex interventions are often required for chronic and comorbid illnesses. Medications are in most cases less effective at treating all facets of diabetes and mental illness together[10]. As a chronic disease, it can impair daily function and mobility, which are more prevalent in homeless people than in homeowners[11]. Having diabetes can be physically and emotionally difficult, both for those with the disease and their families. As a result, people living with it must manage the disease continuously.
There are a number of mental health issues, such as anxiety and depression, which can affect diabetic patients. Diabetes has been linked to mental health complications such as psychotic disorders and complications distinctive to diabetic patients[12]. A number of terms were also utilized to describe the mental health problems connected with diabetes. For example, “diabetes distress” describes the negative emotions experienced by people with diabetes, as well as the burden of managing it, which explains the feelings of despair and emotional turmoil that are specifically related to diabetes, particularly the need for continued monitoring and care, ongoing concerns regarding complications, and the potential for professional and personal relationships to be eroded[13]. A condition known as psychological insulin resistance is characterized by an unwillingness to accept insulin therapy, leading to a delay in starting treatment[14]. Knowledge of the relationship between diabetes and mental health is crucial in that psychiatric and diabetes-specific psychosocial problems are associated with diminished participation in self-management activities that can decrease the quality of life and care for victims and their families. Complications related to diabetes and mortality in the early stages are associated with psychiatric disorders in diabetic patients[15]. In addition to depression, anxiety, and eating disorders, individuals with T1D or T2D are at increased risk of these conditions[16]. For example, depression rates across the lifespan are twice as high for diabetics as for the general population. It was predicted that diabetic patients have poorer mental health generally, and in a variety of mental health dimensions in particular[17]. In addition, studies in the past have shown that diabetes is linked to severe depressive disorder, anxiety, bipolar disorder[18], schizophrenia[19], personality disorders[20,21], stress, trauma, abuse and neglect[22,23], and sleep issues[23]. To reduce the morbidity and mortality associated with diabetes and mental health conditions, non-pharmacological interventions such as critical time intervention (CTI) can be used.
CTI is an intervention program that is time-limited and designed to decrease the adverse effects associated with homelessness and other risky outcomes by providing assistance to individuals in their critical transitional time[24-26]. CTI is characterized by concentrated case management that lasts for 6 to 9 mo and is geared towards assisting mental health patients navigate the severe service system and create contact with long-term community-based links, resources, and interventions[26]. CTI may benefit adults with diabetes and mental health challenges. As a result, comorbid diabetes and mental health conditions make maintaining lifestyle changes more difficult. As a result, this group has more difficulty recognizing and discussing their health concerns, and engaging with services to manage their health[27]. Homelessness and inadequate care may also be challenges they face. Although CTI has received a lot of attention as a way of managing mental health conditions, little is known about its effectiveness in managing and treating coexistent diabetes and mental health conditions. CTI is an evidence-based practice designed to mobilize support for society's most disadvantaged individuals in times of transition[28]. This promotes greater integration into the community and ensures a continuous flow of care by allowing people to remain connected to their communities and social support networks during these difficult times. CTI is also a type of time-limited, intensive case management model of treatment, which helps maintain continuity of care for service users while they are in transition such as from a shelter to a private residence after discharge[25]. As a result of this intervention, a person’s network of support within the community is strengthened[29].
In addition to reducing the risk of homelessness after institutional discharge, CTI strives to enhance the quality of life for individuals and families. It also provides time-limited direct support in terms of emotional and practical assistance during the period of transition by reinforcing the consumer’s long-term ties to formal services, family, and friends[28]. Among the key features of CTI is the provision of post-discharge assistance by workers who have maintained close contact with clients before discharge[30]. Aside from providing emotional and practical assistance during critical transition periods, CTI also offers case management services to enhance the relationship between an individual and their family, friends, and services[31]. There are three stages of CTI[25]: (1) Providing direct assistance to the client and assessing the resources available to support the client; (2) evaluating and adjusting the support systems as necessary; and (3) ensuring that existing community resources are transferred to the client. A variety of groups have benefited from CTI, including veterans, individual with psychiatric disorders, those who have been incarcerated, and people with diabetes. After being discharged from hospitals, shelters, prisons, and other institutions, individuals with mental illness may become homeless. The foundation of CTI rests on elements found in other evidence-based models such as small caseloads, active community outreach, individual case management plans, psychosocial skill building, and motivational coaching are key elements[32-34].
Notwithstanding the substantial role of CTI in the management of mental health problems in patients with other health problems, there is a lacuna with respect to documented empirical evidence of the effectiveness of CTI in enhancing the mental health of diabetic patients. Therefore, conducting a scoping literature review to establish the scope and depth of empirical research on the effectiveness of CTI in improving the mental health of patients with diabetes is necessary due to the prevalence of diabetes worldwide. Taking this study into account, public health practitioners will be able to determine the extent of CTI’s effectiveness in improving the mental wellbeing of diabetics. Furthermore, psychologists or therapists will find this study useful since it will expose the existing gaps regarding CTI in treating the mental health of diabetic patients.
Therefore, the major aim of this study was to establish the current significance of fostering the mental health of patients with diabetes through CTI by conducting a scoping review of the available empirical studies.
The following questions were addressed by this review:
What are the mental health challenges associated with homeless diabetic patients?
What is the impact of CTI in enhancing the mental health of homeless individuals during the time of transition?
Based on a scoping review of existing research studies, the current study examined the significance of fostering the mental health of diabetic patients through CTI. Due to the fact that the study relied on empirical literature analysis, no ethics approval was necessary. Scoping reviews are a valuable tool for mapping the research process on a specific topic.
A protocol defining the methods and defining the inclusion and exclusion criteria was developed in advance. In this review, we followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses[34].
The literature was searched extensively using medical and scientific databases including Google Scholar, PubMed, Scopus, PsycINFO, Reference Citation Analysis (https://www.referencecitationanalysis.com/), and Cochrane Library. Boolean operators were applied to a specific set of keywords (i.e. “OR,” “AND”) during the literature search. Search queries were used across titles, abstracts, subject-specific keywords, and topic fields in databases. The key words used in the primary search stage were: “Diabetes mellitus” OR ‘‘type I diabetes’’ OR ‘‘type II diabetes’’ AND “Mental health” “psychosocial support,” “psychological,” “psychiatric,” “anxiety,” “depression,” AND “critical time interventions” and other terms relevant to the current study (see Table 1).
| Search query | Search keywords applied on titles, abstracts, topics, and subject headings |
| 1 | “Diabetes mellitus” OR ‘‘type I diabetes’’ OR ‘‘type II diabetes’’ OR “diabetic patients” OR “people with diabetes” OR “diabetic conditions” |
| 2 | “Mental health” OR “psychosocial support” OR “psychological” OR “psychiatric” “anxiety,” OR “depression,” OR ‘‘fear” OR ‘‘phobia” OR “dental wellbeing” OR “dental well-being” OR “dental disorder” OR “oral health” OR “wellbeing” OR “mental disorder” OR “schizophrenia” OR “trauma” |
| 3 | “Critical time interventions” OR “case management interventions” |
| Final search query | 1 AND 2 AND 3 |
Following the preliminary search, which ended on September 20, 2023, the researchers added additional search terms to the list based on the results of the first search. The reference lists of the articles included in the search were further reviewed.
This scoping review included articles that met all of the following criteria: Studies that attempted to treat participants of any age with comorbid diabetes and mental health condition; primary studies using either a retrospective or prospective design or a quantitative and/or qualitative design including clinical trials; studies in any country across the globe; full-length studies that were published in journals as peer-reviewed articles; and studies conducted in any year. There were no restrictions on variables such as culture, stage of illness, occupational class, or education. The searches were limited to the English language as the time and cost of translation were not feasible within this review’s timeline.
The exclusion criteria were: Studies that dealt only with the prevalence of mental health among diabetic patients; opinion papers, pre-conference abstracts, and review studies; non-English language articles; commentaries, editorials, or case studies on transition; and studies that treated diabetes without either a mental health construct or homelessness.
Screening: After the database search was completed, the results were exported into Zotero and duplicates were removed. To evaluate all retrieved citations, the authors used a cloud-based systematic review management portal (rayyan.ai). Next, titles were screened to exclude irrelevant publications, opinion papers, and reviews. Then all titles and abstracts of papers were screened by two reviewers using stipulated inclusion and exclusion criteria. To extract and synthesize data, all citations eligible for full-text review were examined using the same methodology. We kept articles with uncertain eligibility status for further review during the assessment process. Finally, the abstracts were read to determine whether the study's aim met the scoping review question.
Selection: The full-text articles were read to confirm each study's eligibility according to the inclusion and exclusion criteria. A third reviewer assisted the first two reviewers in resolving potential conflicts about eligibility through dis
Data extraction process: In the extraction phase, the data were independently extracted from articles according to the theme, purposes, and questions of the present scoping review. Relevant information from all included papers were extracted using a pre-designed data extraction form that included items on study characteristics [e.g., author and year of study, location, population and year of the study, study objective, type of mental health disorder, participants’ characteristics (age of participants and sex among others), method and sample, intervention description and findings]. Two reviewers participated independently in the data extraction process, and a third author reviewed all of the extracted data to ensure consistency and accuracy. All reviewers participating in data extraction discussed discrepancies and reached a consensus.
Using the collective body of evidence, this scoping review produced an evidence map and identified potential gaps. A summary of the major study variables, interventions, and all comorbidity health outcomes were provided by the authors. The findings were arranged and presented in tabular form to provide an overview of the existing studies.
A total of 77 articles related to the mental health of people with diabetes were found during the electronic search of the six databases. Following the removal of duplicates, 72 papers remained. Two independent researchers assessed papers based on stipulated criteria to exclude 48 papers in the first screening, which involved reading titles and abstracts. As a result, 24 papers were screened a second time by reading the full texts while still looking for the inclusion criteria, and three articles were finally selected for data extraction. After full-text assessment, more than five papers were excluded, as shown in Figure 1.
An overview of the included studies is provided in Table 2. Findings from this scoping review revealed that the 19 articles[25,35-52] selected for data extraction were published between 2007 and 2022. The distribution of these studies reviewed across the globe showed that five studies were conducted in Canada, the United States, Japan, Britain, and the Netherlands. The study design included six survey studies, three qualitative, one retrospective evaluation, seven ran
| Authors | Location/population | Objectives | Mental health disorder/CTI/management of diabetes | Method/sample | Results |
| Lennox et al[25] | Britain, 14 | CTI model was adapted to reflect the stages of transition for prisoners in England | CTI | Mixed method of qualitative and quasi-experimental | CTI intervention groups showed a lower level of anxiety regarding release and more support in terms of housing, access to services, and reintegration into the community as compared to previous imprisonment |
| Wiens et al[35] | Ontario, & Toronto, 6944 | To create a population cohort of people with diabetes with a history of homelessness to understand their unique demographic and clinical characteristics and improve long-term health outcomes | Psychotic disorder, Bipolar disorder | Descriptive | Patients with a history of homelessness were more likely to be diagnosed with mental illness (49% vs 2%) and be admitted to a designated inpatient mental health bed (37% vs 1%). A suitable match was found for 5219 (75%) diabetic people with documented homelessness after the intervention. The derived matched cohort was balanced on important demographic and clinical characteristics |
| Davachi and Ferrari[36] | CDIRC in Canada, 524 | To develop an accessible and effective diabetes management support for the homeless population especially those at risk or already diagnosed with diabetes | chronic disease self-management disorder | Survey study | There was a reduction in participants FBG and their HbA1c levels. Although the low numbers of follow-up data collected, the mean reductions in FBG of 4 mmol/L and HbA1c of 1.1% is significant for this population. Baseline results and results captured at the 3 to 12 mo follow-ups were only available for 10 patients with pre-existing diabetes |
| Thompson et al[37] | Canada, 52 | Group medical visits, GMV in primary care for patients with diabetes and low socioeconomic status and low perception of life: users' perspectives and lessons for practitioners | Low perception of life | Qualitative research design | The GMV as a CTI promotes group identification and cohesion against the Diabetes mellitus disease process. The relationships made within the group were found to be supportive and therapeutic. It may also improve individuals' perception of diabetes management from problem solving, modelling, information and education, emotional support, accountability, and social competition |
| Campbell et al[38] | Canada, 28 | To report the experiences of co-researchers with lived experience of homelessness and diabetes, giving voice to patients | Community-based participatory research approach | Qualitative | Many participants felt that the study provided them with intangible benefits, including feeling respected, valued, and heard; feeling accomplished and purposeful, resulting in improved self-efficacy in other areas; and building a sense of community with others who shared many of their life experiences |
| Campbell et al[39] | Canada, 96 | The study documented the innovations in providing diabetes care for individuals experiencing homelessness | Management of diabetes | Survey | Among homeless individuals, this study identified five innovative and unique approaches to diabetes care. Among these approaches are the provision of in-shelter care, the provision of peer outreach, the provision of diabetes specialty outreach clinics, and the provision of diabetes group care specific to this population |
| Mayberry et al[40] | TN United States, 9 | Explore acceptability of engaging family/friends in patients’ T2D self-management using text messaging | Depressive symptoms | Qualitative | A majority of participants (48%) cited needing assistance and seeing the benefits of engaging others as reasons for inviting a support person, while reasons for not inviting one included being an unnecessary "burden" or being unable to text. As a result of the texts, support persons reported an increase in awareness, a creation of dialogue, and an improvement in their own health and behavior |
| Elder and Tubb[41] | United States, 15 | Seeks to understand barriers and enablers to health for homeless people with diabetes as perceived by homeless persons and providers | Management of diabetes | Survey | Despite being regarded as peripheral to diabetes care, all social service providers considered their primary roles to be important |
| Kasprow and Rosenheck[42] | United States, 484 | evaluate an effort to disseminate a program of CTI case management for homeless veterans with mental illness being discharged from veteran psychiatric inpatient units | CTI | Randomized controlled trial | A higher proportion of CTI clients spent more time at home and fewer days in institutional settings than those receiving typical VA services. Clients of CTI case management also reported a reduction in alcohol consumption, drug use, and psychiatric disorders |
| Clark et al[43] | United States, 230 | examine two the CTI management for people with co-occurring disorders and histories of chronic homelessness and to better understand their roles in permanent supported housing | CTI | Descriptive | A significant decrease in alcohol consumption, drug use, and psychological symptoms was also observed in participants of the CTI program |
| Shinn et al[44] | United States, 200 | compared effects of a FCTI to usual care for children in 200 newly homeless families in which mothers had diagnosable mental illness or substance problem | CTI | Randomized trial | In children 6-10 and in adolescents 11-16, referrals to FCTI resulted in fewer internalizing and externalizing problems, as well as self-reported school troubles |
| Tomita and Herman[45] | New York City, 150 | Evaluated the impact of CTI in reducing rehospitalization among formerly homeless individuals with severe and persistent mental illness after discharge from inpatient psychiatric treatment | CTI | Randomized control trial | The study revealed that CTI is effective in lowering psychiatric rehospitalization and efficient in reducing the likelihood of recurrent of homelessness |
| Asgary et al[46] | New York City, 418 | This study assesses diabetes control and rates and predictors of diabetes that is not well-managed among patients experiencing homelessness compared with those of domiciled patients who receive medical care at New York City's shelter-clinics | Mental illness, substance abuse | Retrospective evaluative of T2D measurement | Homeless patients were more likely to have inadequately managed diabetes than other patients. The average HBA1c of homeless individuals was greater than that of domiciled individuals. There was a significant association between diabetic patients with mental illness and a lower HBA1c, as a result of better living conditions in their shelters |
| Keene et al[47] | United States, 5 | Examine transitions into rent-assisted housing as they relate to diabetes self-management behaviors | Management of diabetes | Survey | Participants were able to reduce financial stress and offset diabetes-related expenses as a result of affordable housing and rental assistance |
| Yamamoto et al[48] | Japan, 106 | survey of the prevalence of diabetes and prediabetes among homeless men in Nagoya, Japan | Cognitive disability | Descriptive survey | Prevalence of prediabetes differed significantly between groups with and without a history of social support. The prevalence of prediabetes was lower in the group with social support than in others. Early intervention for preventing diabetes and social support focused on diabetes management is imperative for homeless people |
| Shaw et al[49] | Britain, 150 | Establish effectiveness of CTI in improving engagement of prisoners with mental illness | CTI | Parallel group randomized controlled trial | Participants engaged more fully with CTI than their counterparts. However, the difference was not substantial. Furthermore, the intervention group demonstrated better continuity of care and improved access to services |
| Jarrett et al[50] | United Kingdom, 60 | This study aimed to see whether a CTI in the 1st week’s post-release effectively connects mentally ill prisoners with social, clinical, housing, and welfare services on leaving prison | CTI | Randomized Controlled | The CTI program significantly increased the number of prisoners receiving medication and being registered with their general practitioner |
| de Vet et al[51] | Dutch, 183 | Examined the evidence base in Europe for effective interventions that improve the wellbeing of homeless people | CTI | Parallel-group randomized controlled trial | The CTI significantly enhanced the social support of individuals experiencing low levels of social support and psychological distress |
| Lako et al[52] | Europe, 136 | To examine the effectiveness of CTI—an evidence-based intervention—for abused women transitioning from women’s shelters to community living | CTI | A randomized controlled trial | There is evidence that CTI is effective in reducing post-traumatic stress symptoms and unmet care needs in a population of abused women |
To foster the mental health of homeless diabetic patients, this study used the scoping review approach to reveal the mental health challenges of homeless diabetic patients and the impact of CTI in enhancing the mental health of homeless individuals during the time of transition. Regarding the mental health challenges associated with homeless diabetic patients, this study revealed that diabetic patients with a history of homelessness are more likely to be diagnosed with mental illness such as self-management disorder, low perception, depression, substance abuse, cognitive disability, psychotic disorder, and bipolar disorder. The comorbidity of diabetics and mental health problems of homeless patients are associated with higher hemoglobin A1c (HBA1c). However, taking medication with increased support and su
This review also found that social support services are impactful in the management of comorbidity of diabetes and mental health problems. Such social supports that enhances the mental health of diabetic patients are affordable house rent and rental assistance, which reduce diabetic patients’ expenditure with respect to rent and increases their financial muscle to offset their diabetes-related expenses[47]. In addition, a study identified that provision of in-shelter care, peer outreach and support, diabetes specialty outreach clinics, diabetes group care specific for this population, and com
This review reveals that CTI is impactful in enhancing the mental health of homeless patients during the transitional period from the hospital through social support and interventions to ensure that their needs are met and delivered in a timely manner as well as engagement of these homeless patients. However, the effectiveness of CTI has not been tested in homeless diabetic patients. This means that there is a lacuna in the use of CTI to enhance the mental health of patients with diabetes, especially homeless individuals transitioning from the hospital. However, the literature has shown that the effectiveness of CTI has been established in homeless individuals with mental health problems. A study revealed that CTI enhanced participants’ engagement in continuity with care and improved access to service[49]. Access to service is one focus of CTI, especially for homeless patients during the transition process. CTI is a robust intervention for promoting social support in individuals experiencing psychological distress who have less social support[51]; it promotes the fulfillment of unmet needs and lessens the symptoms of post-traumatic stress symptoms among abused women[52]. Furthermore, CTI is also helpful in transitioning prisoners with mental illness because clients who receive CTI in
The reviewed studies revealed that CTI is impactful in managing individuals with a history of chronic homelessness and co-occurring disorders through a decrease in alcohol use, drugs, and psychiatric symptoms[35,46,47], possibly due to the fact that they are known to suffer from a higher frequency of diabetes-related adverse consequences. A number of factors contribute to this disparity including inadequate access to medical care, inability to pay for medications and supplies, dissatisfaction with healthcare providers, and conflicting priorities.
Moreover, one of the major contributors to the disparities in outcomes is likely related to the fact that diabetes treatments are often not tailored to the specific needs and circumstances of people who are homeless. According to the reviews, no studies have specifically examined the impact of CTI on the mental health of diabetic patients. This indicates that there is a gap in the literature concerning CTI for fostering diabetic patients' mental health. Therefore, more studies are needed to truly understand CTI’s impact on the mental health of diabetic patients.
This review identified two key findings regarding CTI's effectiveness in managing the mental health of homeless patients. First, CTI improves housing outcomes and service engagement use outcomes for homeless people with diabetes-related ailments and their mental health conditions. Results like these coincide with CTI’s focus of connecting individuals with community services and support to address critical transition needs. It is clear from these findings that the CTI model is practical and adaptable in that it can be successfully implemented in a variety of settings and populations[53]. This assertion was demonstrated in the study by Davachi and Ferrari[36], which used a survey research design to conduct a 12-mo intervention study to develop a diabetes management support program for homeless people, especially those at risk or already diagnosed with the disease. According to the study by Davachi and Ferrari[36], social service support, which is part of CTI, is effective for managing the mental health of people with pre-existing diabetes. A cohort study conducted by Wiens et al[35] between 2006 and 2019 in Ontario, Toronto in Canada further supports the above assertion. According to the study, 5219 diabetic people with documented homelessness (75%) found suitable matches. An important demographic and clinical characteristic of diabetic people was also balanced within a derived matched cohort. Second, CTI has been shown to be supportive and therapeutic in managing diabetic patients' mental health. This is substantiated by the studies of Shaw et al[49], de Vet et al[51], Kasprow and Rosenheck[42], and Shinn et al[44] whose findings proved that CTI is effective in enhancing the mental health of homeless individuals. CTI may improve individuals' perception of diabetes management through problem solving, modeling, information and education, emotional support, accountability, and social competition.
This study revealed that diabetic patients with a history of homelessness are more likely to be diagnosed with mental illness, and social support services are impactful for the management of comorbidity of diabetes and mental health problems. This indicates that the mental health disorder of homeless diabetic patients could be attributed to the adverse effects of their environment, which predispose them to substance abuse that increases their mental disorder. Therefore, an intervention such as CTI, which focuses on enhancing the mental health of homeless diabetic patients, is required to facilitate and manage their smooth transition and ensure that they have access to support services that facilitate their integration into society. This study supports existing research demonstrating that CTI is highly effective, supportive, and therapeutic for managing the mental health of patients, especially those who are homeless or have a history of homelessness. As a result, most homeless patients' mental health disorders are managed using either or both of these interventions and ultimately are successful in overcoming their challenges. Therefore, healthcare professionals are well positioned to identify homeless patients and work with them to reduce their individual barriers to diabetes care; however, organizations must ensure that patients are connected to the larger health care system and facilitate low barriers to accessing diabetes care. This review found limited evidence addressing how CTI achieves its positive effects. Exactly how CTI reduces the mental health conditions of diabetic patients with homelessness and other outcomes is unknown. Consequently, this lays the groundwork for future studies investigating CTI's impact on diabetic mental health. Further research is clearly needed to determine whether and how CTI's program components affect specific outcomes and to map these components onto specific mediators.
Due to the unavailability of studies that specifically dealt with the impact of CTI on homeless diabetic patients, this review revolved around the mental health challenges associated with homeless diabetic patients and the impact of CTI in enhancing the mental health of homeless individuals during the time of transition. Second, the included studies used a variety of populations and settings, resulting in a difficult comparison across them. Accordingly, we did not assess methodological quality or bias risk in accordance with the adhering guidelines. Furthermore, the study did not examine the cost of CTI or examine other kinds of case management interventions that could be used in treating diabetic patients’ mental health, instead focusing solely on CTI. Therefore, future reviews should consider all kinds of case management interventions that may be used. Furthermore, we retrieved literature from leading databases to include peer-reviewed articles, while unpublished studies from unselected databases were not included. Last but not least, including only English-language articles may have resulted in a loss of evidence regarding the effectiveness of CTI for diabetic mental health.
This review has shown that homeless diabetic patients are frequently diagnosed with several mental health problems, which require an intervention program such as CTI for enhancing their mental health. The available literature reviewed for this research shows that there is no specific CTI study that focused on managing the mental health of diabetic patients. This indicates that it has not been given adequate attention by researchers. In light of this, more empirical studies should be conducted across the globe, using both participants in hospitals as well as community-based settings to determine the effectiveness of CTI in managing mental health of diabetic patients more effectively and clearly.
Critical time intervention (CTI) is an evidence-based model of practice that is time-limited and aims to provide support for most susceptible individuals during a transition period.
Diabetes can cause other health problems and complications, both physically and psychologically. To reduce the morbidity and mortality associated with diabetes and mental health conditions, non-pharmacological interventions such as CTI can be used.
This research examined the significance of fostering the mental health of diabetes patients through CTI.
This research employed the scoping review methodology and followed the guidelines established by the Joanna Briggs Institute. The search databases were Google Scholar, PubMed, Scopus, PsycINFO, Reference Citation Analysis (https://www.referencecitationanalysis.com/), and Cochrane Library.
Diabetic patients who had experienced homelessness are at higher risk of being diagnosed with mental illness, and social support services are impactful in the management of the comorbidity of diabetes and mental health problems. CTI is impactful in enhancing the mental health of homeless patients during the transitional period from the hospital through social support services.
CTI is a promising intervention for alleviating mental health symptoms in homeless patients. Empirical studies are needed to determine how clinically effectively CTI is in managing the mental health of diabetics.
It is crucial to facilitate and manage the smooth transition of homeless diabetic patients into society, as well as to ensure that they have access to supports services that facilitate their integration into society, by providing CTI that focus on enhancing their mental health.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: South Africa
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Qureshi W, India; Setiawati Y, Indonesia S-Editor: Li L L-Editor: Filipodia P-Editor: Li L
| 1. | Golbidi S, Ebadi SA, Laher I. Antioxidants in the treatment of diabetes. Curr Diabetes Rev. 2011;7:106-125. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 129] [Cited by in RCA: 119] [Article Influence: 8.5] [Reference Citation Analysis (2)] |
| 2. | Devarajan M, Subramaniyaswamy V, Vijayakumar V, Ravi L. Fog-assisted personalized healthcare-support system for remote patients with diabetes. J Ambient Intell Humaniz Comput. 2019;10:3747-3760. [DOI] [Full Text] |
| 3. | Banday MZ, Sameer AS, Nissar S. Pathophysiology of diabetes: An overview. Avicenna J Med. 2020;10:174-188. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 24] [Cited by in RCA: 266] [Article Influence: 53.2] [Reference Citation Analysis (1)] |
| 4. | Rodríguez-Ramírez BA, Rodríguez-Ramírez PM. Relationship between type 2 diabetes and periodontitis. Mex J Med Res ICSA. 2023;11:48-53. [DOI] [Full Text] |
| 5. | Lichti CF, Wan X. Using mass spectrometry to identify neoantigens in autoimmune diseases: The type 1 diabetes example. Semin Immunol. 2023;66:101730. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 8] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 6. | Almheiri A, Alhammadi A, AlShehhi F, Mohammad A, Alshamsi R, Alzaman K, Jabeen S, Haq B. Biomarkers for Prediabetes, Type 2 Diabetes, and Associated Complications. Am J Health Med Nurs Pract. 2023;9:1-21. [DOI] [Full Text] |
| 7. | Heath H, Rosario R, McMichael LE, Fanter R, Alarcon N, Quintana-Diaz A, Pilolla K, Schaffner A, Jelalian E, Wing RR, Brito A, Phelan S, La Frano MR. Gestational Diabetes Is Characterized by Decreased Medium-Chain Acylcarnitines and Elevated Purine Degradation Metabolites across Pregnancy: A Case-Control Time-Course Analysis. J Proteome Res. 2023;22:1603-1613. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 8. | Sousa M, Bruges-Armas J. Monogenic Diabetes: Genetics and Relevance on Diabetes Mellitus Personalized Medicine. Curr Diabetes Rev. 2020;16:807-819. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 16] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 9. | Sartorious N. Comorbidity of mental and physical diseases: a main challenge for medicine of the 21st century. Shanghai Arch Psychiatry. 2013;25:68-69. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 45] [Reference Citation Analysis (0)] |
| 10. | Ee C, Lake J, Firth J, Hargraves F, de Manincor M, Meade T, Marx W, Sarris J. An integrative collaborative care model for people with mental illness and physical comorbidities. Int J Ment Health Syst. 2020;14:83. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 43] [Cited by in RCA: 58] [Article Influence: 11.6] [Reference Citation Analysis (0)] |
| 11. | Nyssa L, Snow-Hill. The survey of attitudes toward homeless people: the validation of a new instrument assessing negative attitudes toward homeless people. Doctoral Thesis, University of South Carolina. 2019. Available from: https://scholarcommons.sc.edu/etd/5394. |
| 12. | Robinson DJ, Coons M, Haensel H, Vallis M, Yale JF; Diabetes Canada Clinical Practice Guidelines Expert Committee. Diabetes and Mental Health. Can J Diabetes. 2018;42:S130-S141. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 118] [Article Influence: 16.9] [Reference Citation Analysis (0)] |
| 13. | Robinson EB, St Pourcain B, Anttila V, Kosmicki JA, Bulik-Sullivan B, Grove J, Maller J, Samocha KE, Sanders SJ, Ripke S, Martin J, Hollegaard MV, Werge T, Hougaard DM; iPSYCH-SSI-Broad Autism Group, Neale BM, Evans DM, Skuse D, Mortensen PB, Børglum AD, Ronald A, Smith GD, Daly MJ. Genetic risk for autism spectrum disorders and neuropsychiatric variation in the general population. Nat Genet. 2016;48:552-555. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 318] [Cited by in RCA: 270] [Article Influence: 30.0] [Reference Citation Analysis (0)] |
| 14. | Polonsky WH, Hajos TR, Dain MP, Snoek FJ. Are patients with type 2 diabetes reluctant to start insulin therapy? An examination of the scope and underpinnings of psychological insulin resistance in a large, international population. Curr Med Res Opin. 2011;27:1169-1174. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 82] [Cited by in RCA: 82] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 15. | Toender A, Vestergaard M, Munk-Olsen T, Larsen JT, Kristensen JK, Laursen TM. Risk of diabetic complications and subsequent mortality among individuals with schizophrenia and diabetes - a population-based register study. Schizophr Res. 2020;218:99-106. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 24] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 16. | Ducat L, Philipson LH, Anderson BJ. The mental health comorbidities of diabetes. JAMA. 2014;312:691-692. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 200] [Cited by in RCA: 245] [Article Influence: 22.3] [Reference Citation Analysis (0)] |
| 17. | Kang W. Investigating the association between diabetes and mental health: A train-and-test approach. Front Psychiatry. 2022;13:1044714. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 18. | Calkin CV, Chengappa KNR, Cairns K, Cookey J, Gannon J, Alda M, O'Donovan C, Reardon C, Sanches M, Růzicková M. Treating Insulin Resistance With Metformin as a Strategy to Improve Clinical Outcomes in Treatment-Resistant Bipolar Depression (the TRIO-BD Study): A Randomized, Quadruple-Masked, Placebo-Controlled Clinical Trial. J Clin Psychiatry. 2022;83. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 46] [Article Influence: 15.3] [Reference Citation Analysis (0)] |
| 19. | Lieberman JA, Stroup TS, McEvoy JP, Swartz MS, Rosenheck RA, Perkins DO, Keefe RS, Davis SM, Davis CE, Lebowitz BD, Severe J, Hsiao JK; Clinical Antipsychotic Trials of Intervention Effectiveness (CATIE) Investigators. Effectiveness of antipsychotic drugs in patients with chronic schizophrenia. N Engl J Med. 2005;353:1209-1223. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3914] [Cited by in RCA: 3739] [Article Influence: 187.0] [Reference Citation Analysis (0)] |
| 20. | Hackett RA, Lazzarino AI, Carvalho LA, Hamer M, Steptoe A. Hostility and physiological responses to acute stress in people with type 2 diabetes. Psychosom Med. 2015;77:458-466. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 20] [Article Influence: 2.0] [Reference Citation Analysis (1)] |
| 21. | Nefs G, Speight J, Pouwer F, Pop V, Bot M, Denollet J. Type D personality, suboptimal health behaviors and emotional distress in adults with diabetes: results from Diabetes MILES-The Netherlands. Diabetes Res Clin Pract. 2015;108:94-105. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 38] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 22. | Farr OM, Ko BJ, Joung KE, Zaichenko L, Usher N, Tsoukas M, Thakkar B, Davis CR, Crowell JA, Mantzoros CS. Posttraumatic stress disorder, alone or additively with early life adversity, is associated with obesity and cardiometabolic risk. Nutr Metab Cardiovasc Dis. 2015;25:479-488. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 60] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 23. | Ramos AR, Wallace DM, Pandi-Perumal SR, Williams NJ, Castor C, Sevick MA, Mcfarlane SI, Jean-Louis G. Associations between sleep disturbances and diabetes mellitus among blacks with metabolic syndrome: Results from the Metabolic Syndrome Outcome Study (MetSO). Ann Med. 2015;47:233-237. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 14] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 24. | Manuel JI, Nizza M, Herman DB, Conover S, Esquivel L, Yuan Y, Susser E. Supporting Vulnerable People During Challenging Transitions: A Systematic Review of Critical Time Intervention. Adm Policy Ment Health. 2023;50:100-113. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 25. | Lennox C, Stevenson C, Edge D, Hopkins G, Thornicroft G, Susser E, Conover S, Herman D, Senior J, Shaw J. critical time intervention: a qualitative study of the perspectives of prisoners and staff. J Forensic Psychiatry Psychol. 2020;31:76-89. [DOI] [Full Text] |
| 26. | Reid N, Mason J, Kurdyak P, Nisenbaum R, de Oliveira C, Hwang S, Stergiopoulos V. Evaluating the Impact of a Critical Time Intervention Adaptation on Health Care Utilization among Homeless Adults with Mental Health Needs in a Large Urban Center. Can J Psychiatry. 2022;67:57-66. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 6] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 27. | Hassan S, Heinkel S, Burton A, Blackburn R, McCloud T, Ross J, Osborn D, Walters K. A qualitative study exploring the barriers and facilitators of implementing a cardiovascular disease risk reducing intervention for people with severe mental illness into primary care contexts across England: the 'PRIMROSE' trial. BMC Health Serv Res. 2020;20:753. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 22] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 28. | Whiffin CJ, Gracey F, Ellis-Hill C. The experience of families following traumatic brain injury in adult populations: A meta-synthesis of narrative structures. Int J Nurs Stud. 2021;123:104043. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 7] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 29. | Silberman School of Social Work. Understanding the critical time intervention model. CTI implementation. 2022. [cited 23 November 2023]. Available from: https://sssw.hunter.cuny.edu/research/centers-networks/. |
| 30. | Cornes M, Aldridge RW, Biswell E, Byng R, Clark M, Foster G, Fuller J, Hayward A, Hewett N, Kilmister A, Manthorpe J, Neale J, Tinelli M, Whiteford M. Improving care transfers for homeless patients after hospital discharge: a realist evaluation. Southampton (UK): NIHR Journals Library, 2021. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 9] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 31. | Howerton AC. Serving poverty & homeless populations through structured encampments with personal interaction (s) and healthcare providers volunteering. Scholar Work, Walden University. Apr 4, 2023. [cited 23 November 2023]. Available from: https://scholarworks.waldenu.edu/cgi/viewcontent.cgi?article=1058&context=picportfolios. |
| 32. | Draine J, Herman DB. Critical time intervention for reentry from prison for persons with mental illness. Psychiatr Serv. 2007;58:1577-1581. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 52] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 33. | Meadows CJ. Ameliorating the revolving door of the mental health crisis and the criminal justice system: A Grant Proposal. MSc Thesis, California State University, Long Beach. 2019. |
| 34. | Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;339:b2535. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18665] [Cited by in RCA: 17508] [Article Influence: 1094.3] [Reference Citation Analysis (1)] |
| 35. | Wiens K, Bai L, Austin PC, Ronksley PE, Hwang SW, Spackman E, Booth GL, Campbell DJ. Characteristics of people with type I or type II diabetes with and without a history of homelessness: A Population-based Cohort Study. 2022 Preprint. Available from: medRxiv: 2022.08.11.22278127. [DOI] [Full Text] |
| 36. | Davachi S, Ferrari I. Homelessness and diabetes: reducing disparities in diabetes care through innovations and partnerships. Can J Diabetes. 2012;36:75-82. [RCA] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 25] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 37. | Thompson C, Meeuwisse I, Dahlke R, Drummond N. Group medical visits in primary care for patients with diabetes and low socioeconomic status: users' perspectives and lessons for practitioners. Can J Diabetes. 2014;38:198-204. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 17] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 38. | Campbell DJT, Campbell RB, DiGiandomenico A, Larsen M, Davidson MA, McBrien K, Booth GL, Hwang SW. Using a community-based participatory research approach to meaningfully engage those with lived experience of diabetes and homelessness. BMJ Open Diabetes Res Care. 2021;9. [DOI] [Full Text] |
| 39. | Campbell DJT, Campbell RB, Booth GL, Hwang SW, McBrien KA. Innovations in Providing Diabetes Care for Individuals Experiencing Homelessness: An Environmental Scan. Can J Diabetes. 2020;44:643-650. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 16] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 40. | Mayberry LS, Bergner EM, Harper KJ, Laing S, Berg CA. Text messaging to engage friends/family in diabetes self-management support: acceptability and potential to address disparities. J Am Med Inform Assoc. 2019;26:1099-1108. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 11] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 41. | Elder NC, Tubb MR. Diabetes in homeless persons: barriers and enablers to health as perceived by patients, medical, and social service providers. Soc Work Public Health. 2014;29:220-231. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 19] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 42. | Kasprow WJ, Rosenheck RA. Outcomes of critical time intervention case management of homeless veterans after psychiatric hospitalization. Psychiatr Serv. 2007;58:929-935. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 33] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 43. | Clark C, Guenther CC, Mitchell JN. Case Management Models in Permanent Supported Housing Programs for People With Complex Behavioral Issues Who Are Homeless. J Dual Diagn. 2016;12:185-192. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 6] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 44. | Shinn M, Samuels J, Fischer SN, Thompkins A, Fowler PJ. Longitudinal Impact of a Family Critical Time Intervention on Children in High-Risk Families Experiencing Homelessness: A Randomized Trial. Am J Community Psychol. 2015;56:205-216. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 38] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 45. | Tomita A, Herman DB. The impact of critical time intervention in reducing psychiatric rehospitalization after hospital discharge. Psychiatr Serv. 2012;63:935-937. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 58] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 46. | Asgary R, Beideck E, Naderi R. Diabetes care and its predictors among persons experiencing homelessness compared with domiciled adults with diabetes in New York City; An observational study. EClinicalMedicine. 2022;48:101418. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 47. | Keene DE, Henry M, Gormley C, Ndumele C. 'Then I Found Housing and Everything Changed': Transitions to Rent-Assisted Housing and Diabetes Self-Management. Cityscape. 2018;20:107-118. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 18] [Reference Citation Analysis (0)] |
| 48. | Yamamoto M, Watanabe T, Uehara R, Horita R, Sado T, Nishio A. Prevalence of diabetes among homeless men in Nagoya, Japan: A survey study. J Diabetes Investig. 2019;10:667-672. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 49. | Shaw J, Conover S, Herman D, Jarrett M, Leese M, McCrone P, Murphy C, Senior J, Susser E, Thornicroft G, Wright N, Edge D, Emsley R, Lennox C, Williams A, Cust H, Hopkin G, Stevenson C. Critical time Intervention for Severely mentally ill Prisoners (CrISP): a randomised controlled trial. Southampton (UK): NIHR Journals Library, 2017. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 18] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 50. | Jarrett M, Thornicroft G, Forrester A, Harty M, Senior J, King C, Huckle S, Parrott J, Dunn G, Shaw J. Continuity of care for recently released prisoners with mental illness: a pilot randomised controlled trial testing the feasibility of a Critical Time Intervention. Epidemiol Psychiatr Sci. 2012;21:187-193. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 41] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 51. | de Vet R, Beijersbergen MD, Jonker IE, Lako DAM, van Hemert AM, Herman DB, Wolf JRLM. Critical Time Intervention for Homeless People Making the Transition to Community Living: A Randomized Controlled Trial. Am J Community Psychol. 2017;60:175-186. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 19] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 52. | Lako DAM, Beijersbergen MD, Jonker IE, de Vet R, Herman DB, van Hemert AM, Wolf JRLM. The effectiveness of critical time intervention for abused women leaving women's shelters: a randomized controlled trial. Int J Public Health. 2018;63:513-523. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 20] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 53. | Herman DB. Transitional Support for Adults with Severe Mental Illness: Critical time intervention and its roots in assertive community treatment. Res Soc Work Pract. 2014;24:556-563. [DOI] [Full Text] |