Published online Dec 16, 2023. doi: 10.12998/wjcc.v11.i35.8392
Peer-review started: September 5, 2023
First decision: November 1, 2023
Revised: November 6, 2023
Accepted: December 4, 2023
Article in press: December 4, 2023
Published online: December 16, 2023
Processing time: 100 Days and 1 Hours
Ligamentum flavum cysts, which are most common in mobile junctional levels of the spine, can be a rare cause of spinal stenosis. There have been several case reports of ligamentum flavum cysts. However, there is yet to be a documented case report of a calcified ligamentum flavum cyst. Herein, we report the first case of a calcified ligamentum flavum cyst causing ankle and toe weakness.
A 66-year-old male visited our hospital complaining of claudication as well as thigh and calf pain in his left leg, all beginning two weeks prior. Physical examination revealed motor weakness of the left ankle dorsiflexion and great toe dorsiflexion. Lumbar spinal computed tomography scans showed spinal stenosis combined with a calcified mass at the left side of the L4-5 level. Magnetic reso
The patient’s ankle and great toe weakness were improved successfully after surgical removal of the calcified cyst.
Core Tip: Ligamentum flavum cyst in lumbar spine can be a rare cause of spinal stenosis. There have been several case reports of ligamentum flavum cysts. However, to the best of our knowledge, no calcified ligamentum flavum cyst has been reported. We report the first case of a calcified ligamentum flavum cyst causing neurological claudication and motor weakness of lower extremities. We believe that our report would be useful for a diagnostic approach and treatment in patients who have spinal stenosis with neurological claudication and motor weakness.
- Citation: Jung HY, Kim GU, Joh YW, Lee JS. Ankle and toe weakness caused by calcified ligamentum flavum cyst: A case report. World J Clin Cases 2023; 11(35): 8392-8398
- URL: https://www.wjgnet.com/2307-8960/full/v11/i35/8392.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i35.8392
Ligamentum flavum cysts are a rare cause of spinal stenosis, which causes neurological claudication and pain in the lower extremities[1]. Ligamentum flavum cysts appear on the ventral surface of the ligament without any connections to articular facets. The precise pathogenic mechanism underlying the formation of ligamentum flavum cysts remains unclear. However, the development of these cysts has been suggested to be associated with persistent micro-instability at the motion segment and concomitant micro-trauma, which can increase the risk of cyst formation[2]. There have been several reports of ligamentum flavum cyst[3-8]. However, to our knowledge, there has yet to be a report of a calcified cyst of ligamentum flavum. Herein, we report the first case of a calcified ligamentum flavum cyst presenting ankle and toe weakness.
A 66-year-old male presented with claudication, thigh and calf pain and motor weakness in his left leg.
He complained of weakness in his left great toe and ankle beginning two weeks prior to his visit, and the complained that his symptoms had become gradually aggravated with time.
Hypertension as underlying disease.
There was no specific family health history.
Motor weakness of the left ankle dorsiflexion (grade 2) and great toe dorsiflexion (grade 0 to 1).
When the patient admitted to our hospital, laboratory investigations revealed low levels of hemoglobin (10.5 g/dL, normal range: 14.0-18.0) with low levels of hematocrit (30.7 %, normal range: 42.0-52.0). White blood cell count was 6.70 × 109/L [normal range: (4.0-10.0) × 109] and platelet count was 240 × 109/L [normal range: (150-450) × 109]. Coagulation function test: Prothrombin time (PT): 10.0 s (normal range: 9.7-13.3); PT%: 119% (normal range: 77-120); international normalized ratio: 0.90 (normal range: 0.88-1.20); activated partial thromboplastin time: 28.8 s (normal range: 23.1-37.3). These results were all within normal ranges.
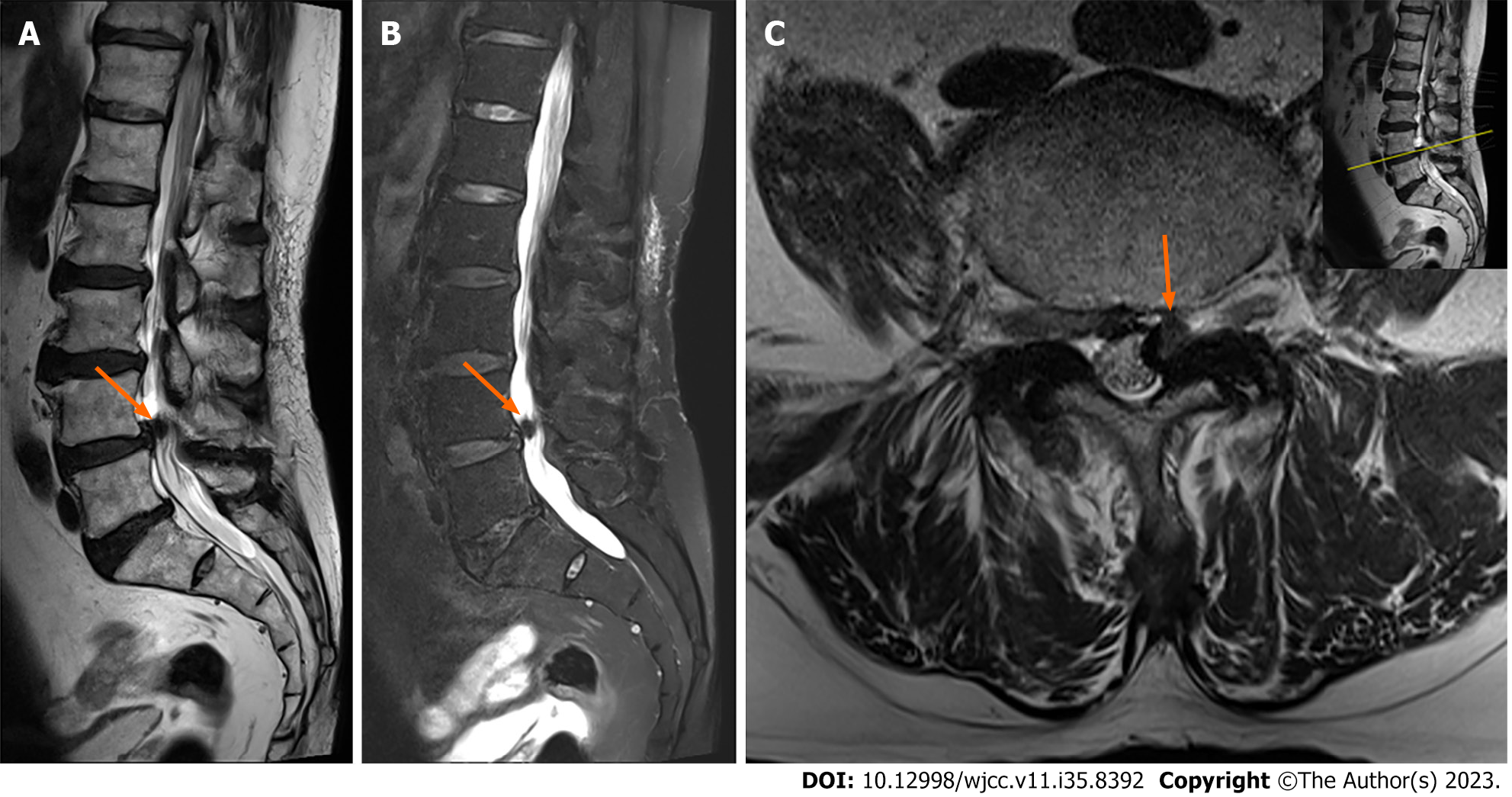
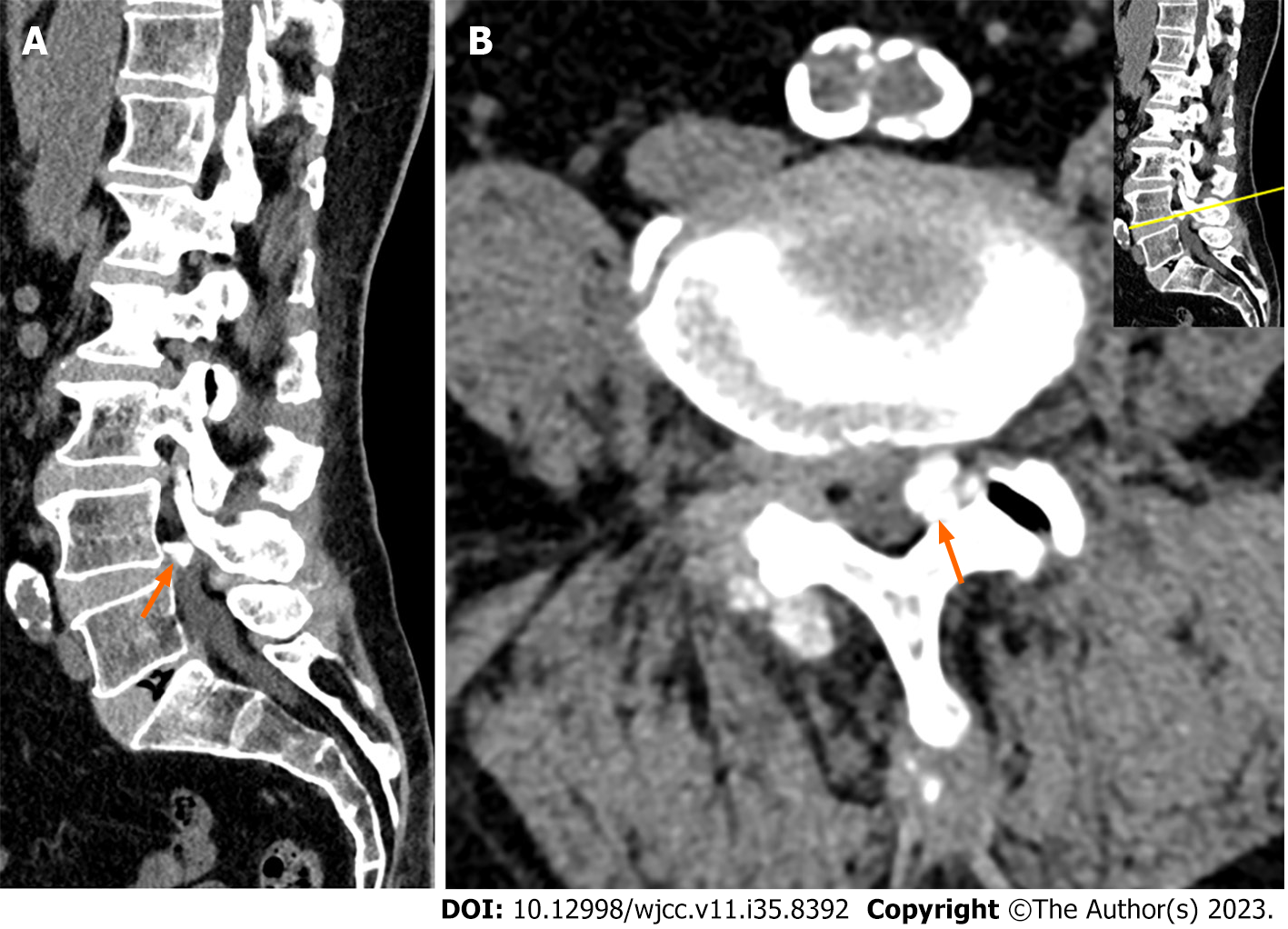
Plain radiograph of the lumbar spine showed degenerative changes and spondylolisthesis L4 on L5 (Figure 1). Magnetic resonance imaging (MRI) showed protrusion disc and dural sac compression attributable to a mass at the L4-5 level (Figure 2). Lumbar spinal computed tomography (CT) scans showed spinal stenosis combined with dural sac compression caused by a calcified mass at the left side of the L4-5 level (Figure 3).
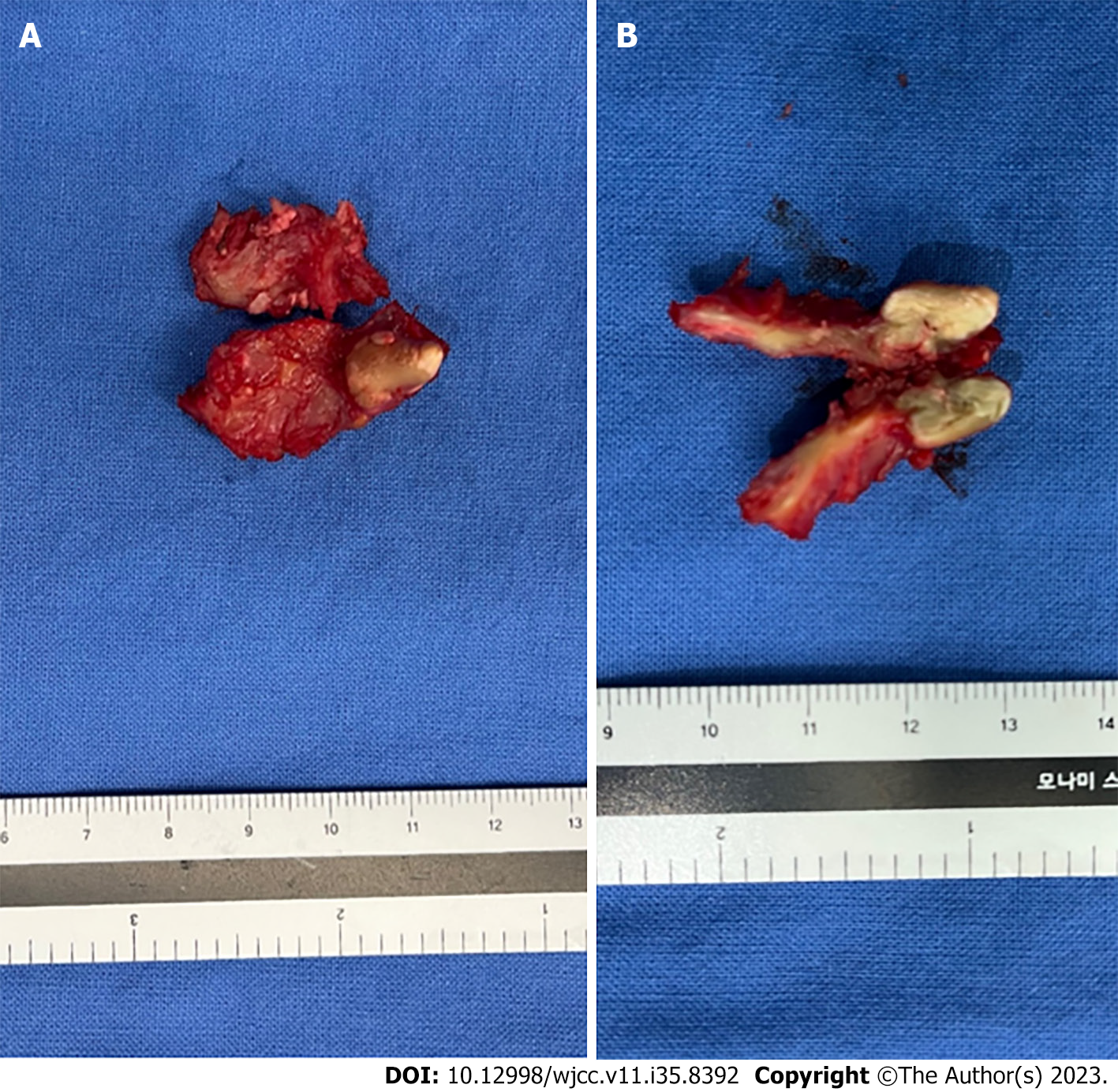
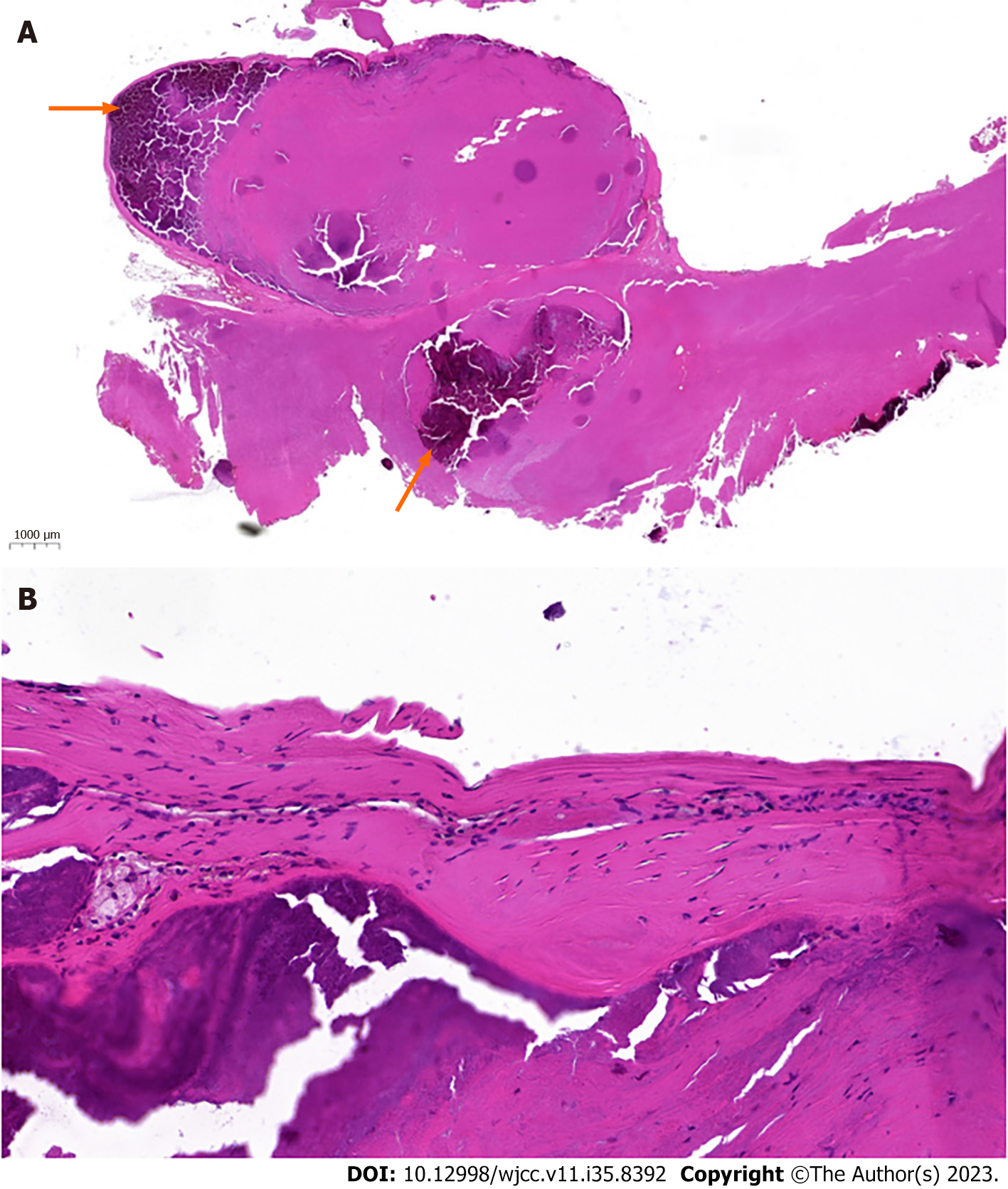
Calcified pseudocyst of ligamentum flavum was confirmed by histological examination after surgery (Figures 4 and 5).
Decompressive laminectomy and excision of the calcified mass for lumbar spinal stenosis, along with posterior lumbar interbody fusion at the L4-5 level for spondylolisthesis were performed.
Immediately after surgery, the pain in his left thigh and calf improved, but the motor weakness in his left ankle and great toe remained. On the fourth postoperative day, histological examination confirmed a calcified pseudocyst of ligamentum flavum (Figure 5). Two weeks after the operation, the motor weakness in the patient’s ankle and great toe had improved gradually, and he was discharged from the hospital.
Ligamentum flavum cyst was first described by Moiel et al[8] in 1967, in a case where it compressed dural sac and presented as testicular pain and leg radiating pain. Ligamentum flavum cyst can be distinguished from facet joint cyst by its location on the ventral surface of the ligamentum flavum without any connections to articular facet[9,10]. The pathogenic mechanism of ligamentum flavum cyst has yet to be clearly identified. Segmental instability and micro-trauma have been described as major causes of the formation of ligamentum flavum cysts[9-11]. Segmental instability and micro-trauma at motion segment are believed to predispose one to cyst formation. Ligamentum flavum consists of elastic fiber with a reduced amount of collagen fibers. When lesions occur due to micro-trauma or segmental instability, the regeneration of elastic fibers is extremely limited. This limited regeneration leads to a decrease in the elasticity of ligamentum flavum along with the deposition of collagen[12]. The accumulation of collagen in ligamentum flavum leads to progressive degeneration, and the myxoid changes can form cysts[13]. In our case, we found a segmental instability with grade I spondylolisthesis at the L4-5 level in our patient. It could also be considered a possible cause of cyst formation. However, the mechanism of calcification of ligamentum flavum cyst is unknown. It is presumed that calcification additionally occurred in the degenerative change of ligamentum flavum.
In general, ligamentum flavum cyst can be diagnosed using MRI. Ligamentum flavum cyst typically appears as hyperintense on T2-weighted images and as hypointense on T1-weighted images, where it appears as a cyst arising from the ventral surface of ligamentum flavum[6]. In our case, axial images of the L4-5 level showed left side dural sac compression by a mass that appears as hypointense on T2-weighted and T1-weighted images. Based on these MRI findings, we considered the mass to be a sequestrated disc material. However, lumbar CT scans revealed dural sac compression by the calcified mass at the left side of the L4-5 level. It was then surgically confirmed that the mass was a calcified cyst of ligamentum flavum cysts. In this way, performing CT scans along with MRI can aid one in making an accurate diagnosis.
Conservative treatment, such as that consisting of medication and percutaneous steroid injections, can be performed in ligamentum flavum cysts. However, these conservative therapies have not shown successful long-term results[4,14]. Surgical decompression with cyst excision is the treatment of choice when conservative treatment fails[4,14]. In this case, we decided to perform surgical removal of the calcified ligamentum flavum cyst due to the progression of motor weakness.
To our knowledge, the treatment reported herein is the first surgical treatment for calcified ligamentum flavum cyst causing ankle and toe weakness. We performed surgical decompression and excision of the calcified cyst. After the surgery, the patient’s motor weakness gradually improved.
We thank Dr. Eun-Sun Jung for her suggestions regarding the preparation of pathologic slides. We also thank the patient for providing consent for this case report.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: South Korea
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Lu M, China S-Editor: Wang JJ L-Editor: A P-Editor: Yu HG
| 1. | Kwon JW, Moon SH, Park SY, Park SJ, Park SR, Suk KS, Kim HS, Lee BH. Lumbar Spinal Stenosis: Review Update 2022. Asian Spine J. 2022;16:789-798. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 47] [Reference Citation Analysis (0)] |
| 2. | Onofrio BM, Mih AD. Synovial cysts of the spine. Neurosurgery. 1988;22:642-647. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 197] [Cited by in RCA: 191] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 3. | Taha H, Bareksei Y, Albanna W, Schirmer M. Ligamentum flavum cyst in the lumbar spine: a case report and review of the literature. J Orthop Traumatol. 2010;11:117-122. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 20] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 4. | Seo DH, Park HR, Oh JS, Doh JW. Ligamentum flavum cyst of lumbar spine: a case report and literature review. Korean J Spine. 2014;11:18-21. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 9] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 5. | Kalidindi KKV, Bhat MR, Gupta M, Mannem A, Chhabra HS. Ligamentum Flavum Cyst With Acute Onset Motor Deficit: A Literature Review and Case Series. Int J Spine Surg. 2020;14:544-551. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 6. | Singh V, Rustagi T, Mahajan R, Priyadarshini M, Das K. Ligamentum Flavum Cyst: Rare Presentation Report and Literature Review. Neurol India. 2020;68:1207-1210. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 7. | Ayberk G, Ozveren F, Gök B, Yazgan A, Tosun H, Seçkin Z, Altundal N. Lumbar synovial cysts: experience with nine cases. Neurol Med Chir (Tokyo). 2008;48:298-303; discussion 303. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 34] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 8. | Moiel RH, Ehni G, Anderson MS. Nodule of the ligamentum flavum as a cause of nerve root compression. Case report. J Neurosurg. 1967;27:456-458. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 27] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 9. | Baker JK, Hanson GW. Cyst of the ligamentum flavum. Spine (Phila Pa 1976). 1994;19:1092-1094. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 61] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 10. | Wildi LM, Kurrer MO, Benini A, Weishaupt D, Michel BA, Brühlmann P. Pseudocystic degeneration of the lumbar ligamentum flavum: a little known entity. J Spinal Disord Tech. 2004;17:395-400. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 24] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 11. | Howington JU, Connolly ES, Voorhies RM. Intraspinal synovial cysts: 10-year experience at the Ochsner Clinic. J Neurosurg. 1999;91:193-199. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 66] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 12. | Viejo-Fuertes D, Liguoro D, Rivel J, Midy D, Guerin J. Morphologic and histologic study of the ligamentum flavum in the thoraco-lumbar region. Surg Radiol Anat. 1998;20:171-176. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 52] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 13. | Yoshida M, Shima K, Taniguchi Y, Tamaki T, Tanaka T. Hypertrophied ligamentum flavum in lumbar spinal canal stenosis. Pathogenesis and morphologic and immunohistochemical observation. Spine (Phila Pa 1976). 1992;17:1353-1360. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 143] [Cited by in RCA: 136] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 14. | Bureau NJ, Kaplan PA, Dussault RG. Lumbar facet joint synovial cyst: percutaneous treatment with steroid injections and distention--clinical and imaging follow-up in 12 patients. Radiology. 2001;221:179-185. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 63] [Article Influence: 2.6] [Reference Citation Analysis (0)] |