Published online Dec 16, 2023. doi: 10.12998/wjcc.v11.i35.8291
Peer-review started: September 27, 2023
First decision: October 9, 2023
Revised: October 22, 2023
Accepted: November 30, 2023
Article in press: November 30, 2023
Published online: December 16, 2023
Processing time: 78 Days and 2.7 Hours
Varicosis is a common venous condition, which is typically treated surgically. However, selection of the optimal surgical approach can be challenging. Previous studies comparing endovenous laser treatment (EVLT) and conventional surgery were retrospective and observational in nature and the results may therefore have been influenced by selection bias and the presence of other confounding factors. In this study, we used propensity score matching to reduce selection bias when comparing EVLT and conventional surgery for the treatment of varicose great saphenous veins.
To compare the perioperative and postoperative outcomes of EVLT and conventional surgery in patients with great saphenous vein varicosis.
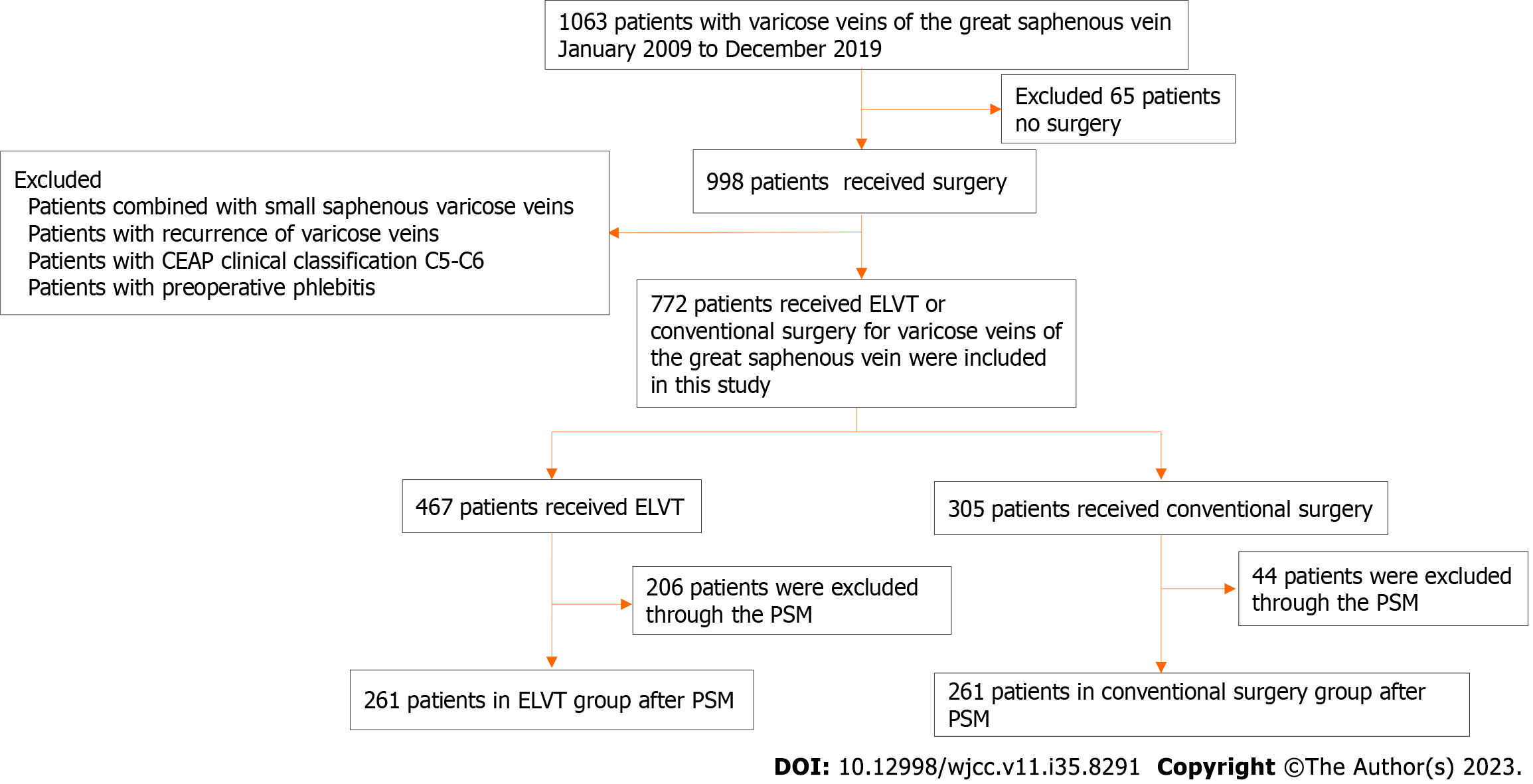
We retrospectively reviewed the records of 1063 patients treated for primary varicosis of the great saphenous vein at the Second Affiliated Hospital of Xuzhou Medical University between January 2009 and December 2019. Among them, 56 patients were excluded owing to additional small saphenous varicose vein involvement, 81 owing to recurring varicose veins, 83 owing to complicated varicose veins (CEAP clinical classification C5-C6), and 6 owing to perioperative phlebitis. Finally, 772 patients were enrolled in this study. Standard demographic and clinicopathological data were collected from the medical records of the patients. For propensity score matching, 522 patients (261 who underwent EVLT and 261 who underwent conventional surgery) were randomly matched 1:1 by age, sex, onset time, smoking status, presence of diabetes, family history, stress therapy, C class, and the affected leg.
Of the 772 patients included in the study, 467 underwent EVLT and 305 underwent conventional surgery. There were significant differences in age, onset time, smoking and diabetes status, and family history between the two groups. Following propensity score matching, no significant differences in patients’ characteristics remained between the two groups. ELVT was associated with a shorter operation time and hospital stay than conventional surgery, both before and after propensity score matching. There were no differences in complications between the two groups after propensity score matching. Patients who underwent EVLT had a higher recurrence rate during the two-year follow-up period than those who underwent conventional surgery (33.33% vs 21.46%, χ2 = 11.506, P = 0.001), and a greater percentage of patients who underwent EVLT experienced pain one week after the procedure (39.85% vs 19.54%, P = 0.000).
EVLT may not always be the best option for the treatment of great saphenous vein varicosis.
Core Tip: In the study, we first time use a propensity score matching analysis to compare endovenous laser treatment (EVLT) and conventional surgery for great saphenous vein varicosis, we found that EVLT offers advantages in terms of surgical time and invasiveness. However, it exhibits a higher postoperative recurrence rate and greater postoperative pain compared to conventional surgery. Propensity score matching was employed to reduce bias. These findings emphasize the importance of considering individual patient characteristics and preferences when selecting the optimal treatment method for varicose veins, shedding light on the nuanced trade-offs between EVLT and conventional surgery in clinical practice.
- Citation: Li Q, Zhang C, Yuan Z, Shao ZQ, Wang J. Endovenous laser treatment vs conventional surgery for great saphenous vein varicosities: A propensity score matching analysis. World J Clin Cases 2023; 11(35): 8291-8299
- URL: https://www.wjgnet.com/2307-8960/full/v11/i35/8291.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i35.8291
Great saphenous vein (GSV) varicosis is more common in women than in men[1]. In most cases varicose veins are harmless; however, in severe cases they can result in chronic disabling ulcers, which can have a major impact on patients’ quality of life and ability to work. It has been estimated that half of adults experience mild venous insufficiency, and varicose veins are visible in approximately 15% of men and 35% of women[2-4]. Therefore, there is a need to identify suitable clinical treatments for varicose veins.
Currently, surgery is the preferred treatment for GSV varicose veins, with high ligation and stripping being the most common surgical technique; however, this procedure has been associated with a high rate of postoperative clinical recurrence, a slow recovery, and visible scarring[5-7]. Minimally invasive endovenous laser treatment (EVLT) is beco
The aim of this study was to compare the perioperative and postoperative results of EVLT and CS in patients with GSV varicose veins, using PSM to avoid bias and known confounding factors.
We retrospectively reviewed the records of all patients with GSV varicose veins undergoing treatment at the Department of General Surgery of the Second Affiliated Hospital of Xuzhou Medical University between January 2009 and December 2019. Exclusion criteria were as follows: (1) Treatment involving neither CS nor EVLT; (2) complicated varicose veins (CEAP clinical classification, C5-C6); (3) recurrence of varicose veins; (4) combined GSV and small saphenous vein involvement; (5) preoperative phlebitis; (6) presence of acute systemic infectious diseases; (7) consent not provided; and (8) patients who did not have any other causes. The patients were divided into two groups: EVLT and CS. Clinicopathological data, including sex, age, onset time, clinical classification, surgery time, surgical technique, and complications, were collected. All patients underwent deep venography before surgery to rule out deep vein thrombosis.
A flowchart of this study is shown in Figure 1. The study was approved by the Ethics Committee of the Second Affiliated Hospital of Xuzhou Medical University.
Conventional surgical procedure: An oblique incision, approximately 5 cm long, was made parallel to the inguinal ligament with the oval fossa as the midpoint, on the right pubic bone and two transverse fingers downwards. The skin, subcutaneous tissue, and superficial fascia was incised to expose the oval fossa, and the confluence of the GSV and the femoral vein was dissected. The superficial iliac circumflex vein, superficial abdominal wall vein, and external pudendal vein were dissected, and the internal and external femoral veins were ligated and cut, respectively. The GSV was freed to the junction with the femoral vein, and ligated and clamped with the fourth line from the femoral vein. Suturing was performed after ligation at the proximal end, and the distal end was temporarily clamped with hemostatic forceps to await detachment. Hemostatic forceps were used to open the distal end of the GSV and insert a vein dissector, and temporary ligation was carried out using silk thread to control bleeding; the dissector was advanced slowly towards the lower leg. After the dissector entered the upper part of the inner ankle, a small incision was made at this position to separate and cut the GSV. The distal end was ligated, and the proximal end was ligated on the dissector. Then the dissector was pulled upwards to slowly extract the GSV. The skin at the branch of the severe varicose GSV was cut, subcutaneous separation was performed, the communicating branch was ligated and cut, the varicose vein was fully peeled off and cut, and the incisions were sutured sequentially.
EVLT: The saphenous vein sheath surrounding the GSV was injected with tumescent anesthesia (500 mL physiological saline, 10 mL 1% lidocaine, and 0.5 mL 0.1% adrenaline) under the guidance of ultrasound. The saphenous vein was then punctured anterior to the medial malleolus under ultrasound guidance, with the puncture needle core removed and exchanged for a 5F puncture cannula sheath. A 0.035 ultra-slip long guidewire was inserted from the cannula to the junction of the GSV and femoral vein, and a 5F catheter was sent along the guidewire to 1 cm below the junction of the saphenofemoral vein. With the guidance of the catheter, a 2 cm transverse incision was made under the groin, the GSV was freed, and after the catheter was retreated 2-5 cm, the saphenous vein was double-ligated 1 cm below the junction of the saphenofemoral vein. The guidewire was then extracted and the fiber was advanced through the catheter, until the fiber head was 1 cm below the ligation of the GSV, and the end of the fiber head was more than 2 cm beyond the end of the catheter. The optical fiber was connected to the semiconductor laser treatment instrument, whose power (14 W for the GSV trunk), with a target linear endovenous energy density of 80-100 J/cm, was applied using an 810 nm laser source (Leifukang, Shanghai, China; 1.5 s pulse, 1 s interval).
Subsequently, multi-point puncture laser closure was performed for each branch of the varices, and each branch of the varices was cauterized sequentially. After strict hemostasis, the incisions were sutured using absorbable sutures.
After CS or EVLT, the affected limb was wrapped in an elastic bandage to apply pressure. Patients were helped to get out of bed and perform a small amount of activity 6 h after the operation, and the bandages were removed after 72 h. All patients wore medical elastic stockings for at least 3 mo after discharge from hospital.
Follow up: Evaluations of varicose veins were typically performed 1-4 wk, 3-6 mo, and 2 years after the procedure. Recurrence was confirmed through ultrasound doppler examination at follow-up, indicating local recurrence or trunk recanalization. In cases of severe recurrence, patients exhibited visible varicose veins and experienced clinical symptoms during the follow-up period. Pain levels, as measured on a visual analog scale (VAS) ranging from 0 (no pain) to 10 (worst possible pain) were assessed 1 wk after the procedure.
PSM: We used the nearest-neighbor matching method with no replacement for our propensity score analysis in a one-to-one match. We tested the matching algorithm using a histogram of the propensity score and a dot plot to standardize mean differences based on logistic regression. Matching was performed using a caliper of 0.02.
Quantitative data are expressed as mean ± SD, and individual t-tests were used to compare differences between the groups. The chi-square test was used to compare categorical data between the groups. Clinical recurrence was analyzed by the Kaplan-Meier method with intergroup log rank significance testing. Statistical analysis and PSM were performed using SPSS Statistics for Windows software version 26.0 (IBM Corporation, Armonk, NY, United States), and P < 0.05 was considered to indicate statistical significance. All tests were two-sided.
A total of 1063 patients diagnosed with GSV varicosis were assessed for eligibility: 65 patients who were not surgically treated, 56 patients with combined GSV and small saphenous vein involvement, 81 patients with recurrent varicosis, 83 patients with a CEAP clinical classification of C5-C6, and 6 patients with perioperative phlebitis were excluded. Finally, 772 patients were included in this study, of whom 467 received EVLT and 305 underwent CS (Figure 1).
Selection bias and confounding factors influenced the analysis, and significant differences were found in age, onset time, smoking and diabetes status, and inheritance between the groups (P < 0.05). After PSM, comparison of the remaining 261 patients in each group revealed no significant differences (P > 0.05) (Table 1).
| Variables | Overall population (n = 772) | Before matching | After matching | ||||||
| EVLT (n = 467) | CS (n = 305) | t/χ2 | P value | EVLT (n = 261) | CS (n = 261) | t/χ2 | P value | ||
| Sex, n (%) | 2.695 | 0.101 | 0.284 | 0.594 | |||||
| Female | 324 (41.97) | 207 (44.33) | 117 (38.36) | 111 (42.53) | 105 (40.23) | ||||
| Male | 448 (58.03) | 260 (55.67) | 188 (61.64) | 150 (57.47) | 156 (59.77) | ||||
| Age (yr) | 58.09 ± 9.62 | 56.04 ± 10.48 | -2.784 | 0.006 | 56.89 ± 9.517 | 56.64 ± 10.344 | 0.286 | 0.775 | |
| Duration (mo) | 84.80 ± 34.42 | 71.52 ± 40.14 | -4.902 | 0.000 | 78.97 ± 36.72 | 77.72 ± 37.88 | 0.384 | 0.701 | |
| Smoking, n (%) | 286 (37.05) | 158 (33.83) | 128 (41.97) | 5.234 | 0.022 | 104 (39.85) | 99 (37.93) | 0.202 | 0.653 |
| Diabetes, n (%) | 74 (9.59) | 41 (8.78) | 33 (10.82) | 8.655 | 0.003 | 28 (10.73) | 28 (10.73) | 0.000 | 1.000 |
| Family history, n (%) | 158 (20.47) | 78 (16.70) | 80 (26.23) | 10.288 | 0.001 | 66 (25.29) | 61 (23.37) | 0.260 | 0.610 |
| Compression therapy, n (%) | 204 (26.42) | 114 (24.41) | 90 (29.51) | 2.465 | 0.116 | 72 (27.59) | 67 (25.67) | 0.245 | 0.621 |
| C class, n (%) | 1.910 | 0.385 | 1.627 | 0.443 | |||||
| C2 | 121 (15.67) | 80 (17.13) | 41 (13.44) | 43 (16.48) | 34 (13.03) | ||||
| C3 | 406 (52.59) | 242 (51.82) | 164 (53.77) | 132 (50.57) | 144 (55.17) | ||||
| C4 | 245 (31.74) | 145 (31.05) | 100 (32.79) | 86 (32.95) | 83 (31.80) | ||||
| Legs, n (%) | 2.851 | 0.240 | 2.753 | 0.252 | |||||
| Left | 298 (38.60) | 181 (38.76) | 117 (38.36) | 98 (37.55) | 103 (39.46) | ||||
| Right | 262 (33.94) | 95 (20.34) | 167 (54.75) | 98 (37.55) | 81 (31.03) | ||||
| Both | 212 (27.46) | 93 (19.91) | 119 (39.02) | 65 (24.90) | 77 (29.50) | ||||
As shown in Table 2, no postoperative wound infection or deep venous thrombosis occurred, and there were no significant differences in phlebitis or paresthesia incidence between the two groups. Before PSM, the EVLT group had 18 hematomas, whereas the CS group had 7 hematomas (P = 0.034), however, after PSM, there was no significant difference (P = 0.593) in the incidence of local hematoma between the two groups. In terms of pain rate, there was no significant difference between EVLT and CS groups (P = 0.272), but there was a significant difference after PSM (P = 0.000). The results of the EVLT group were superior to those of the CS group in terms of surgical time and hospital stay before (P = 0.000, P = 0.000, respectively) and after PSM (P = 0.000, P = 0.000, respectively). However, in terms of recurrence after surgery, EVLT was inferior to CS both before (P = 0.004) and after (P = 0.001) PSM.
| Characteristics | Before matching | After matching | ||||||
| EVLT | CS | t/χ2 | P value | EVLT | CS | t/χ2 | P value | |
| Surgical time | 61.73 ± 17.38 | 70.68 ± 19.71 | 6.627 | 0.000 | 62.21 ± 17.66 | 70.86 ± 19.63 | 5.294 | 0.000 |
| Hospital day | 4.57 ± 2.14 | 6.56 ± 2.84 | 11.1 | 0.000 | 4.52 ± 2.12 | 6.64 ± 2.95 | 9.436 | 0.000 |
| Phlebitis | 31 | 19 | 0.051 | 0.822 | 19 | 16 | 0.276 | 0.600 |
| Local hematoma | 18 | 7 | 8.712 | 0.034 | 4 | 3 | 5.348 | 0.593 |
| Pain | 149 | 68 | 130.00 | 0.272 | 104 | 51 | 25.777 | 0.000 |
| Paresthesia | 103 | 82 | 2.362 | 0.124 | 63 | 75 | 1.418 | 0.234 |
| Wound infection | 0 | 0 | - | - | 0 | 0 | - | |
| Deep venous thrombosis | 0 | 0 | - | - | 0 | 0 | - | |
| Recurrence | 149 | 68 | 8.433 | 0.004 | 92 | 57 | 11.506 | 0.001 |
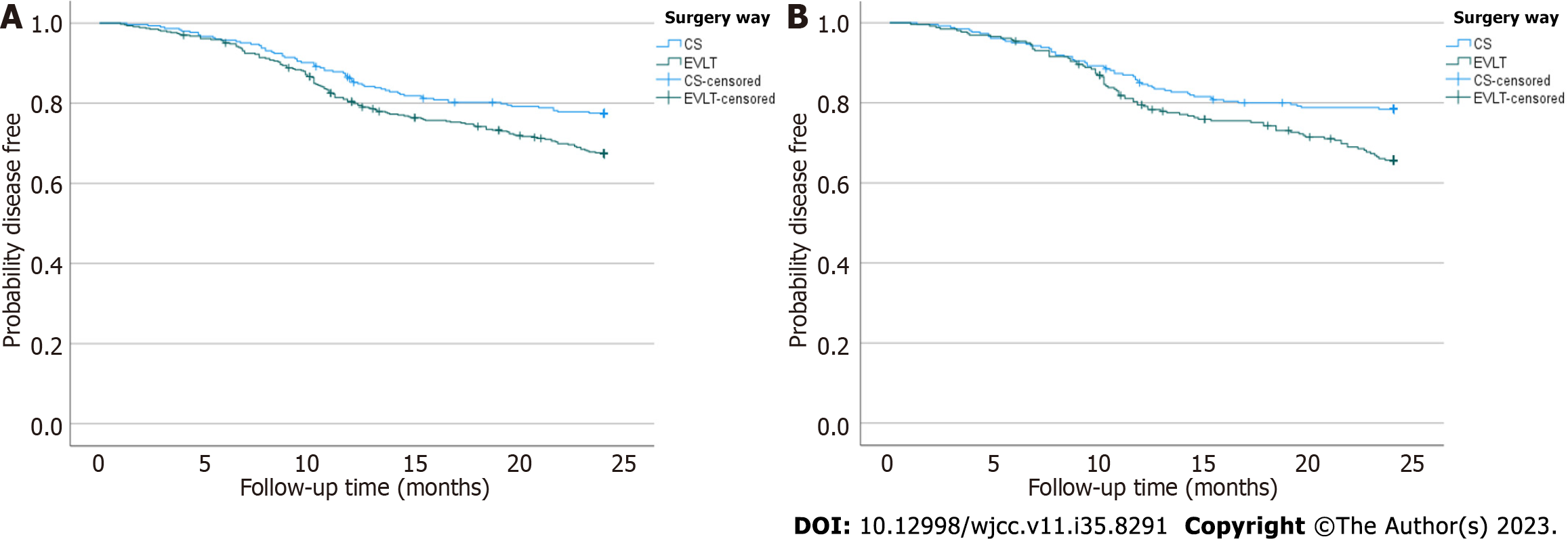
Two years after surgery, 149 (31.90%) of 467 patients that underwent EVLT, and 68 (22.30%) of 305 patients that underwent CS, experienced recurrence (P = 0.004). After PSM, the recurrence rate of the EVLT group was 33.33%, higher than that of the CS group (21.46%, P = 0.001). The median recurrence time of the EVLT group was 10.7 mo, later than that of the CS group (9.8 mo, P < 0.05; Figure 2). The results showed that patients who received EVLT were more likely to experience recurrence than those who underwent CS, but at a later date.
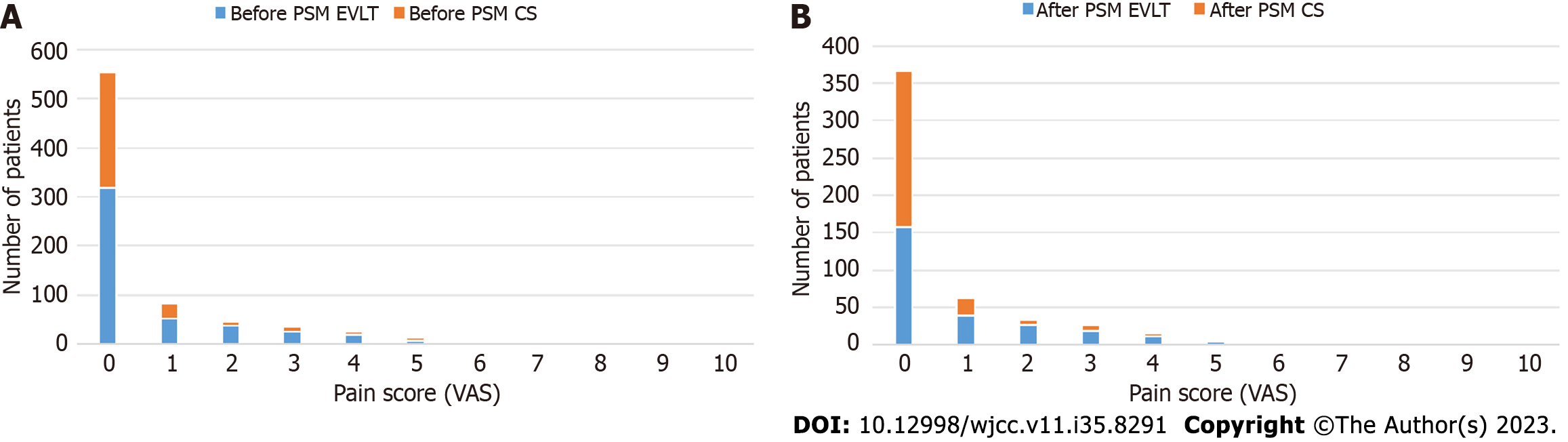
Pain levels were measured 1 wk postoperatively using a VAS, the results are presented in Figure 3. Of the entire patient cohort, 318 of 467 (68.09%) patients who received EVLT and 237 of 305 (77.70%) patients who received CS experienced no pain, and no pain scores of 10 were recorded. After PSM, the number of patients who experienced no pain was 157 (60.15%) and 210 (80.46%) in the EVLT and CS groups, respectively.
Before PSM, there was no significant difference in the percentage of patients who experienced pain between the EVLT and CS groups (30.19% vs 22.29%, P = 0.272), however, after PSM there was a significant difference between the EVLT and the CS groups (39.85% vs 19.54%, P = 0.000). This indicated that patients who underwent EVLT experienced more pain than those who underwent CS.
GSV varicosis is a common peripheral vascular condition, which is typically caused by incomplete closure of venous valves and often leads to venous blood reflux, distal venous stasis, and GSV expansion, bulging, and twisting[17]. The most effective treatment is surgery, and EVLT and CS are two of the main surgical methods[18].
EVLT delivers heat energy to the blood vessel lumen, which deforms or inactivates the proteins and enzymes in the blood vessel wall. As the vein wall becomes damaged, fibrosis develops, which causes the blood vessels to permanently constrict and close[19]. EVLT has become a commonly used treatment option for incompetent saphenous veins and has been proven highly effective by a number of studies[20]. However, different studies have found that the outcomes of EVLT are different from conventional surgery. A study conducted by Roopram AD shows that endovenous laser ablation has a lower recurrence rate and higher pain rating than saphenopopliteal laser ablation[21]. Another study conduced by Shrestha et al[22] show that There were no differences in the rate of recurrence at 1, 2, and 5 years, and EVLA was associated with fewer postoperative complications than conventional surgery. A 5-years randomized controlled trial show that EVLT have a significantly higher varicose vein recurrence rate than saphenofemoral ligation and stripping[23]. Variability in these studies might be attributed to the retrospective, observational nature of these studies, which may have produced selection bias and confounding variables . Therefore, we used PSM to avoid bias and known confounding factors. The rate of recurrence of varicosis and the pain were higher after EVLT than after CS, but the surgical time, hospital stay, and invasiveness of surgery were superior in the EVLT group. These results are consistent with those of Gauw et al[23], who conducted a 5-years randomized controlled trial.
It is important to note that this study had some limitations. This was a retrospective study at a single center with a relatively small number of participants. Statistical power and research value may have been weakened due to the retrospective design and low number of patients. It is possible that additional potential factors could have influenced the allocation of patients to different groups, other than the nine covariates included in PSM to eliminate selection bias and other confounding factors.
It is important for surgeons to choose the correct surgical method for the treatment of varicosis, and this selection should be made on a case-by-case basis. The results of our study suggest that EVLT should not always be considered the best possible option. The development of novel procedures with significantly longer treatment lengths provides promising future treatment strategies, although further refinements in both technique and technology are required.
Great saphenous vein (GSV) varicosis is a common condition, predominantly affecting women. It can result in chronic ulcers, impacting patients' quality of life. Varicose veins affect a substantial portion of the adult population, necessitating effective clinical treatments.
Current surgical treatments, particularly high ligation and stripping, have limitations such as postoperative recurrence, slow recovery, and scarring. Minimally invasive endovenous laser treatment (EVLT) has gained popularity, with claims of better patient outcomes compared to conventional surgery (CS).
This study aims to compare perioperative and postoperative outcomes of EVLT and CS in GSV varicose vein patients, while mitigating bias through propensity score matching (PSM) to address confounding factors.
Data from patients with GSV varicose veins treated at a specific medical center were retrospectively reviewed. Propensity score matching was used to ensure balanced groups, and statistical analyses were conducted.
Before PSM, EVLT showed benefits in surgical time, hospital stay, and invasiveness but was associated with higher recurrence rates and postoperative pain compared to CS. After PSM, there were no significant differences in hematoma incidence or local hematoma. However, EVLT continued to exhibit a higher recurrence rate and postoperative pain compared to CS.
The study suggests that EVLT, while less invasive, may not always be the best choice for GSV varicose vein treatment due to higher recurrence rates and pain. The choice of treatment should be tailored to individual cases. Novel procedures with longer treatment lengths may offer future treatment strategies.
The study's retrospective design and relatively small sample size pose limitations. Further refinements in both technique and technology are needed to enhance treatment outcomes. Surgeons should make treatment decisions on a case-by-case basis, considering the specific needs and characteristics of patients.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Methodology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): 0
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Beeraka NM, India S-Editor: Yan JP L-Editor: A P-Editor: Zhao S
| 1. | Mousa A, El Azzazi M, Elkalla MA. Different management options for primary varicose veins in females: A prospective study. Surg Open Sci. 2019;1:25-33. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 6] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 2. | Kemp MT, Obi AT, Henke PK, Wakefield TW. A narrative review on the epidemiology, prevention, and treatment of venous thromboembolic events in the context of chronic venous disease. J Vasc Surg Venous Lymphat Disord. 2021;9:1557-1567. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 3. | Lim CS, Gohel MS, Shepherd AC, Davies AH. Secondary care treatment of patients with varicose veins in National Health Service England: at least how it appeared on a National Health Service website. Phlebology. 2010;25:184-189. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 18] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 4. | Healy DA, Kimura S, Power D, Elhaj A, Abdeldaim Y, Cross KS, McGreal GT, Burke PE, Moloney T, Manning BJ, Kavanagh EG. A Systematic Review and Meta-analysis of Thrombotic Events Following Endovenous Thermal Ablation of the Great Saphenous Vein. Eur J Vasc Endovasc Surg. 2018;56:410-424. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 81] [Article Influence: 11.6] [Reference Citation Analysis (0)] |
| 5. | Fischer R, Linde N, Duff C, Jeanneret C, Chandler JG, Seeber P. Late recurrent saphenofemoral junction reflux after ligation and stripping of the greater saphenous vein. J Vasc Surg. 2001;34:236-240. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 157] [Cited by in RCA: 127] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 6. | Castro-Ferreira R, Quelhas MJ, Freitas A, Vidoedo J, Silva EA, Marinho A, Abreu R, Coelho A, Dias PG, Sampaio SM. Vascular training does matter in the outcomes of saphenous high ligation and stripping. J Vasc Surg Venous Lymphat Disord. 2019;7:732-738. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 7. | Li Y, Wu W, Li Y, Li J, Sun M. Efficacy and safety of endovenous microwave ablation vs laser ablation for great saphenous vein varicosis: study protocol for a multicentre, randomised controlled non-inferiority trial. BMJ Open. 2022;12:e059213. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |
| 8. | Yang L, Wang X, Wei Z, Zhu C, Liu J, Han Y. The clinical outcomes of endovenous microwave and laser ablation for varicose veins: A prospective study. Surgery. 2020;168:909-914. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 20] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 9. | van Groenendael L, Flinkenflögel L, van der Vliet JA, Roovers EA, van Sterkenburg SM, Reijnen MM. Conventional surgery and endovenous laser ablation of recurrent varicose veins of the small saphenous vein: a retrospective clinical comparison and assessment of patient satisfaction. Phlebology. 2010;25:151-157. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 21] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 10. | Liu JJ, Fan LH, Xu DC, Li X, Dong ZH, Fu WG. The endovenous laser treatment for patients with varicose veins. Pak J Med Sci. 2016;32:55-58. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 11. | Whing J, Nandhra S, Nesbitt C, Stansby G. Interventions for great saphenous vein incompetence. Cochrane Database Syst Rev. 2021;8:CD005624. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 17] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 12. | Zollmann M, Zollmann C, Zollmann P, Veltman J, Cramer P, Stüecker M. Recurrence types 3 years after endovenous thermal ablation in insufficient saphenofemoral junctions. J Vasc Surg Venous Lymphat Disord. 2021;9:137-145. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 13. | Brake M, Lim CS, Shepherd AC, Shalhoub J, Davies AH. Pathogenesis and etiology of recurrent varicose veins. J Vasc Surg. 2013;57:860-868. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 57] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 14. | Winokur RS, Khilnani NM, Min RJ. Recurrence patterns after endovenous laser treatment of saphenous vein reflux. Phlebology. 2016;31:496-500. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 18] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 15. | Go SJ, Cho BS, Mun YS, Kang YJ, Ahn HY. Study on the Long-Term Results of Endovenous Laser Ablation for Treating Varicose Veins. Int J Angiol. 2016;25:117-120. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 16. | Little RJ, Rubin DB. Causal effects in clinical and epidemiological studies via potential outcomes: concepts and analytical approaches. Annu Rev Public Health. 2000;21:121-145. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 477] [Cited by in RCA: 477] [Article Influence: 19.9] [Reference Citation Analysis (0)] |
| 17. | Tauraginskii RA, Lurie F, Agalarov R, Simakov S, Borsuk D. Blood flow from competent tributaries is likely contributor to distally increasing reflux volume in incompetent great saphenous vein. J Vasc Surg Venous Lymphat Disord. 2022;10:69-74. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 18. | Raetz J, Wilson M, Collins K. Varicose Veins: Diagnosis and Treatment. Am Fam Physician. 2019;99:682-688. [PubMed] |
| 19. | Nesbitt C, Bedenis R, Bhattacharya V, Stansby G. Endovenous ablation (radiofrequency and laser) and foam sclerotherapy versus open surgery for great saphenous vein varices. Cochrane Database Syst Rev. 2014;CD005624. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 47] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 20. | Farah MH, Nayfeh T, Urtecho M, Hasan B, Amin M, Sen I, Wang Z, Prokop LJ, Lawrence PF, Gloviczki P, Murad MH. A systematic review supporting the Society for Vascular Surgery, the American Venous Forum, and the American Vein and Lymphatic Society guidelines on the management of varicose veins. J Vasc Surg Venous Lymphat Disord. 2022;10:1155-1171. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 32] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 21. | Roopram AD, Lind MY, Van Brussel JP, Terlouw-Punt LC, Birnie E, De Smet AA, Van der Ham AC. Endovenous Laser Ablation versus Conventional Surgery in the Treatment of Small Saphenous Vein Incompetence: Short-Term Results of a Multicenter Randomized Controlled Trial. J Vasc Surg Venous Lymphat Disord. 2013;1:106. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 22. | Shrestha O, Basukala S, Thapa N, Karki S, Pant P, Paudel S. Endovenous laser ablation versus conventional surgery (ligation and stripping) for primary great saphenous varicose vein: a systematic review and meta-analysis. Ann Med Surg (Lond). 2023;85:4509-4519. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 23. | Gauw SA, Lawson JA, van Vlijmen-van Keulen CJ, Pronk P, Gaastra MT, Mooij MC. Five-year follow-up of a randomized, controlled trial comparing saphenofemoral ligation and stripping of the great saphenous vein with endovenous laser ablation (980 nm) using local tumescent anesthesia. J Vasc Surg. 2016;63:420-428. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 58] [Article Influence: 5.8] [Reference Citation Analysis (0)] |